Overview of Gastrointestinal Secretions and Structural Considerations
In this informative presentation by Assistant Professor Dr. Emre Hamurtekin, the focus is on gastrointestinal secretions including salivary, gastric, pancreatic, biliary, and intestinal fluids. Structural considerations such as the surface area for absorption, sphincters, villi, and crypts are discussed in detail. Salivary secretion, its constituents, control mechanisms, functions, and influencing factors like chewing and fear are highlighted. The process of gastric secretion and anatomic considerations related to the gastrointestinal system are also covered.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
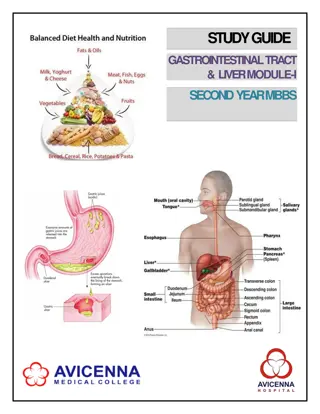
GASTROINTESTINAL PHYSIOLOGY Chapter-I (Gastrointestinal Secretions) Ass. Prof. Dr. Emre Hamurtekin EMU Faculty of Pharmacy
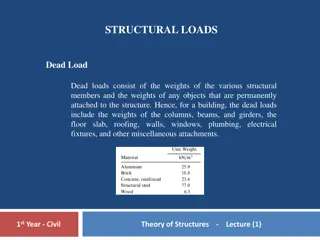
STRUCTURAL CONSIDERATIONS The intestine has a very substantial surface area for absorption. Sphincters: upper & lower esophageal sphincters pylorus ileocecal valve inner & outer anal sphincters
STRUCTURAL CONSIDERATIONS Throughout the small intestine, it is folded up into fingerlike projections called villi. Crypts are the infoldings between the villi.
GASTROINTESTINAL SECRETIONS Salivary secretion Gastric secretion Pancreatic secretion Biliary secretion Intestinal fluid
SALIVARY SECRETION Saliva is produced by 3 pairs of salivary glands: Parotid gland Submandibular gland Sublingual gland Constituents: Amylase (initiate digestion) IgA, lysozyme (protect oral cavity from bacteria) Mucin (lubricate the food) Saliva is hypotonic and alkaline Salivary secretion is almost entirely controlled by neural influences: Parasympathetic*: most important role Sympathetic: composition of saliva (little influence on volume)
SALIVARY SECRETION Chewing Sleep Fear Fatigue Smelling/Seeing food Nausea Salivary secretion Functions of saliva: Facilitates swallowing Initiates digestion Keep the mouth moist Solvent for molecules that stimulate the taste buds Aids speech Keep the mouth and teeth clean (mechanical&antibacterial)
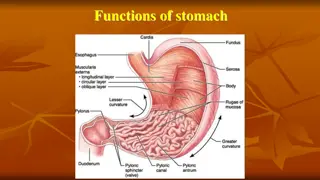
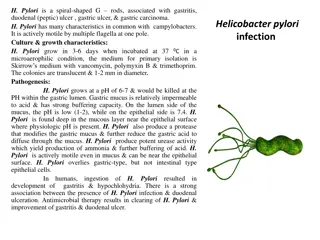
ORIGIN & REGULATION Cephalic phase (before the meal is taken) Gastric phase (most significant) Intestinal phase (when the meal left the stomach) SECRETIONS: (fundus/body of stomach) Surface mucous cells: mucus, bicarbonate, trefoil peptide Parietal cells: hydrocholoric acid, intrinsic factor ECL cell: histamine secretion Chief cell: pepsinogen AND gastric lipase
ORIGIN & REGULATION There are 3 primary stimuli of gastric secretion: Gastrin Histamine Acetylcholine GASTRIN: Gastrin is a hormone released by G cells in the antrum of the stomach. It is released in response to, a) GRP (bombesin) which is relesed from enteric nerve endings b) oligopeptides in the gastric lumen. Carried to fundic glands by bloodstream Binds to receptors on parietal, chief cells(?) to activate secretion and also ECL cells to activate histamine release HISTAMINE: Binds to H2 receptors on parietal cells and activate parietal cell secretion. ACETYLCHOLINE: Enteric nerve endings release acetylcholine Stimulates parietal and chief cells
ORIGIN & REGULATION During the cephalic phase of gastric secretion, secretion is activated by vagal input originates from the brain region. Vagal outflow to the stomach releases acetylcholine and GRP initiating secretory function. Meal constituents trigger gastrin release + distension of stomach activates strech receptors which provoke vago-vagal and local reflexes that further amplify gastric secretion. Somatostatin (released from antral D cells) inhibits both G and ECL cells as well as parietal cell acid secretion.
GASTRIC PARIETAL CELLS Stomach Lumen Acid secretion cAMP Ca Ca M3 H2 Basolateral membrane CCK-B Ach Histamine Gastrin
ANATOMIC STRUCTURE Exocrine pancreas is a compound alveolar gland. Duct cells : secrete bicarbonate HCO3 is secreted in exchange for Cl (Cl / HCO3 exchanger) Exocrine cells : secrete enzymes Zymogen granules are formed in the cell and discharged by exocytosis. The small duct radicles pancreatic duct of Wirsung ampulla of Vater papilla (sphincter of Oddi) Duct of Santorini duodenal
PANCREATIC JUICE Pancreatic juice is alkaline and has a high bicarbonate content. Most of the digestive enzymes in the pancreatic juice are released in inactive forms. Trypsin is main the activator of most of the pro-enzymes. Acute pancreatitis !!! Secretion of pancreatic juice is primarily under hormonal control: Secretin - rich in HCO3 and poor in enzymes CCK (cholecystokinin) rich in enzymes but low in volume The effect of secretin is mediated by cAMP The effect of CCK is mediated by phospholipase C Neuronal control: Acetylcholine - cause discharge of zymogen granules (mediated by phospholipase C)
INTRODUCTION FUNCTIONS: Digestion and absorption of fats (bile acids) Excretory fluid by which the body disposes of lipid soluble end products of metabolism lipid soluble xenobiotics cholesterol (native or as bile acids)
BILE Bile is made up of bile acids, bile pigments, and other substances dissolved in alkaline solution. Bilirubin and biliverdin pigments are responsible for the color of the bile. Bile acids is the most important component in bile for the digestion and absorption function of the biliary secretion. 4 major bile acids in humans: Cholic acid primary (principle) Chenodeoxycholic acid bile acids Deoxycholic acid Lithocholic acid
BILE Cholic acid Deoxycholic acid Colonic bacteria Chenodeoxycholic acid Lithocholic acid Colonic bacteria Ursodeoxycholic acid Colonic bacteria Seconder bile acids: Deoxycholic acid Lithocholic acid Ursodeoxycholic acid
BILE Bile acids reduce surface tension. Bile acids are responsible for emulsification of fat preparatory to its digestion and absorption in the small intestine (form micelles).
BILE 90-95% of the bile acids are absorbed from small intestine. Simple diffusion Na-bile salt co-transport system (terminal ileum) 5-10% are enter the colon and converted to deoxycholic acid (absorbed back) and lithocholic acid (mostly excreted in the stool) Absorbed bile acids are transported back to the liver (enterohepatic circulation) and excreted again in the bile.
Daily water turnover (ml) in GI tract INGESTED 2000 ENDOGENOUS SECRETIONS * Salivary glands 1500 * Stomach 2500 * Bile 500 * Pancreas 1500 * Intestine 1000 7000 TOTAL INPUT 2000 + 7000 = 9000 REABSORBED * Jejunum 5500 * Ileum 2000 * Colon 1300 8800 BALANCE IN STOOL 9000 - 8800 = 200
INTESTINAL FLUID In the small intestine, secondary active transport of Na is important in bringing about absorption of glucose, amino acids and bile acids. Presence of glucose in the intestinal lumen facilitates Na reabsorption. Between meals, Na and Cl are absorbed together by coupled activity of Na / H exchanger and Cl / HCO3 exchanger.
ELECTRONEUTRAL NaCl ABSORPTION IN THE SMALL INTESTINE and COLON Apical Basal 2K H 3Na Na, K ATPase NHE Na 3Na HCO3 CLD Cl Cl Modified from Ganong s Physiology
ELECTROGENIC Na ABSORPTION IN THE COLON K Na Apical 2K 3Na Na, K ATPase 2K Na Na Distal colon epithelium Basal Modified from Ganong s Physiology
Daily water turnover (ml) in GI tract INGESTED 2000 ENDOGENOUS SECRETIONS * Salivary glands 1500 * Stomach 2500 * Bile 500 * Pancreas 1500 * Intestine 1000 7000 TOTAL INPUT 2000 + 7000 = 9000 REABSORBED * Jejunum 5500 * Ileum 2000 * Colon 1300 8800 BALANCE IN STOOL 9000 - 8800 = 200
Cl SECRETION IN SMALL INTESTINE and COLON 2Cl Na Cl K 2Cl Cl Na K Lumen Na Na, K ATPase K Modified from Ganong s Physiology