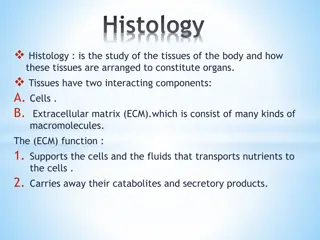
Understanding Tissue Repair Mechanisms: Regeneration and Fibrosis
Tissue repair involves complex mechanisms like regeneration by parenchymal cells or fibrosis leading to scar formation. Inflammatory cells play a crucial role in tissue repair, along with processes like ECM synthesis and cell migration. Different types of cells in the body have varying regenerative capacities, from labile continuously dividing cells to permanent non-proliferative cells. Extracellular signaling via soluble mediators occurs through autocrine, paracrine, synaptic, and endocrine pathways. The repair process includes angiogenesis, fibroblast migration and proliferation, ECM deposition, and tissue remodeling.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Tissue Repair Stimuli that induce death in some cells can trigger the activation of replication pathways in others; recruited inflammatory cells not only clean up the necrotic debris but also elaborate mediators that drive the synthesis of new extracellular matrix (ECM). -Regeneration of injured tissue by parenchymal cells of the same type. -Replacement by connective tissue (fibrosis), resulting in a scar. - Regeneration and scarring involve essentially similar mechanisms including cell migration, proliferation, and differentiation, as well as matrix synthesis. - Regeneration of epithelium requires an intact basement membrane (BM) matrix.
Mechanisms of tissue repair. In this example, injury to the liver is repaired by regeneration if only the hepatocytes are damaged, or by laying down of fibrous tissue if the matrix is also injured.
The cells of the body are divided into three groups on the basis of their regenerative capacity: 1-Labile cells: These are continuouslydividing (and continuously dying) and include: -The Hematopoietic cells in the bone marrow. -The stratified squamous surfaces of the skin, oral cavity, vagina, and cervix. -The cuboidal epithelia of the ducts draining exocrine organs (e.g., salivary glands, pancreas, biliary tract). -The columnar epithelium of the gastrointestinal tract, uterus, and fallopian tubes. -The transitional epithelium of the urinary tract. 2-Stable cells:quiescent in their normal state, but are capable of undergoing rapid division in response to injury. These include: -The parenchyma of most solid glandular tissues, including liver, kidney, and pancreas. -The Endothelial cells lining blood vessels, and the fibroblast and smooth muscle connective tissue (mesenchymal) cells. 3-Permanent cells: Terminally differentiated and nonproliferative in postnatal life. The majority of neurons and cardiac muscle cells belong to this category.
Extracellular signaling via soluble mediators occurs in four different forms: 1-Autocrine signaling, in which a soluble mediator acts the cell that secretes it. This pathway is important in the immune response (cytokines) and in compensatory epithelial hyperplasia (e.g., liver regeneration). 2-Paracrine signaling: mediators affect cells only in the immediate vicinity. This pathway is important for recruiting inflammatory cells to the site of infection and for the controlled process of wound healing. 3-Synaptic: activated neural tissue secretes neurotransmitters at a specialized cell junction (synapse) onto target cells such as other nerves or muscle. 4-Endocrine, in which a regulatory substance, such as a hormone, is released into the bloodstream and acts on target cells at a distance.
General components of repair process: -Formation of new blood vessels (angiogenesis). -Migration and proliferation of fibroblasts. -Deposition of ECM. -Maturation and reorganization of the fibrous tissue (remodeling). Blood vessels are assembled by two processes: -Vasculogenesis: in embryonic development occure by angioblasts (endothelial cell precursors). -Angiogenesis (neovascularization) by which preexisting vessels send out capillary sprouts to produce new vessels. Four general steps occur in the development of a new capillary vessel: -Proteolytic degradation of the parent vessel BM to form of a capillary sprout. -Migration of endothelial cells from the original capillary toward an angiogenic stimulus. -Proliferation of the endothelial cells. -Maturation of endothelial: this includes recruitment and proliferation of pericytes (for capillaries) and smooth muscle cells (for larger vessels) to support the endothelial tube and provide accessory functions.
Fibrosis (Scar Formation) Fibrosis, or scar formation, builds on the granulation tissue framework of new vessels and loose ECM that develop early at the repair site. The process of fibrosis occurs in two steps: (1) Emigration and proliferation of fibroblasts into the site of injury. (2) Deposition of ECM by these cells. The recruitment and stimulation of fibroblasts is driven by many of the growth factors, including platelet-derived growth factor (PDGF), FGF, and TGF- . The main source of these factores are activated Endothelium and Macrophages. Scar Remodeling Shifts in the composition of the ECM; even after its synthesis and deposition, scar ECM continues to be modified and remodeled. Degradation of collagens and other ECM components performed by metalloproteinases (zinc ions for their activity). These enzymes are produced by (fibroblasts, macrophages, neutrophils,synovial cells, and some epithelial cells)
Angiogenesis resulting from, A, the mobilization of bone marrow endothelial precursor cells (EPCs), and, B, from preexisting vessels at the site of injury. EPCs can be mobilized from the bone marrow and migrate to a site of injury and differentiate and form a mature network by linking with preexisting vessels. Endothelial cells from preexisting vessels become motile and proliferate to form capillary sprouts. Regardless of the mechanism of angiogenesis, vessel maturation requires the recruitment of pericytes and smooth muscle cells to form the periendothelial layer.
Phases Wound healing: include: 1-Inflammatory phase by the initial injury. (First 48 hours- 6 days). 2-proliferative phase (7 days to 6 weeks): -Parenchymal cell regeneration (where possible). -Migration and proliferation of both parenchymal and connective tissue cells -Synthesis of ECM proteins. 3-Remodeling phase (Maturation phase) (Day 8 through years). -For parenchymal elements to restore tissue function. -For connective tissue to achieve wound strength. Types of healing: 1-Healing by First Intention Healing of a clean, uninfectedsurgical incision approximated by surgical sutures. This is referred to as primary union, or healing by first intention. -Causes only focal disruption of epithelial basement membrane. -Death of a relatively few epithelial and connective tissue cells. -Epithelial regeneration.
Wounds during inflammatory Phase
Healing by Second Intention When cell or tissue loss is more extensive, as in infarction, inflammatory ulceration, abscess formation, or even just large wounds. -Regeneration of parenchymal cells alone cannot restore the original architecture. -Extensive ingrowth of granulation tissue from the wound margin, -Accumulation of ECM and scarring. This form of healing is referred to as secondary union, or healing by second intention. Secondary healing differs from primary healing in several respects: 1-Large tissue defects intrinsically have a greater volume of necrotic debris, exudate, and fibrin that must be removed. 2-Much larger amounts of granulation tissue are formed. 3-Secondary healing exhibits wound (contraction): Within 6 weeks, large skin defects may be reduced to 5% to 10% of their original size, largely by contraction. This may due to modified of fibroblasts to contractiblemyofibroblasts. -The accumulation of exuberant amounts of collagen can give rise to prominent, raised scars known as keloids.
Steps in wound healing by first intention (left) and second intention (right). In the latter, note the large amount of granulation tissue and wound contraction.
Secondary Wound Healing Wound contraction
Healing of skin ulcers. A, Pressure ulcer of the skin, commonly found in diabetic patients. B, A skin ulcer with a large gap between the edges of the lesion. C, A thin layer of epidermal re-epithelialization, and extensive granulation tissue formation in the dermis. D, Continuing re-epithelialization of the epidermis and wound contraction.
Keloid. A, Excess collagen deposition in the skin forming a raised scar known as a keloid. B, Thick connective tissue deposition in the dermis.
Keloid Scar Keloid