Understanding Liver Complications in Cystic Fibrosis: Latest Insights for 2024
Liver complications in cystic fibrosis (CF) have gained importance due to CFTR modulators impacting liver health. This presentation by Dr. Zachary M. Sellers delves into new definitions for CF liver disease, CFF recommendations for screening, management, and treatment of hepatobiliary issues in CF. It discusses the background, CF-associated liver disease, liver injury like fibrosis and cirrhosis, and newer terms like CF Hepatobiliary Involvement. The focus is on early indicators of liver damage, changes in bile ducts, and the significance of liver inflammation markers. The session aims to enhance understanding and management of liver complications in CF patients.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Liver Complications of Cystic Fibrosis: What s New in 2024 Zachary M. Sellers, MD, PhD Adjunct Professor of Pediatrics Stanford University School of Medicine Stanford CF Education Day March 9, 2024
Disclosures 4D Molecular Therapeutics: Contract consultant on gene therapy in rare pulmonary diseases, including CF. BridgeBio Pharma: Paid consultant on drug development in pancreatitis. Renexxion: Paid consultant on the development of therapeutics for CF gastrointestinal complications. I will not discuss any products under development. I have no financial interest in these companies.
Objectives Review background on liver complications in CF Discuss new definitions for CF Liver Disease Present new CFF recommendations for screening, management, and treatment of hepatobiliary complications in CF
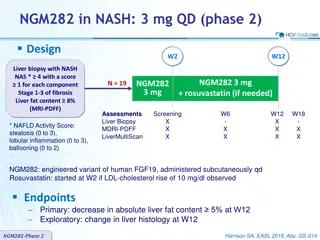
Background Liver and biliary complications are well known to occur in CF Increased attention with CFTR modulators causing increases in blood markers of liver inflammation (e.g. AST, ALT) CFTR is expressed in cholangiocytes, cells that line the bile ducts inside and outside of the liver Earliest indicators of injury in liver originate from bile ducts (e.g., GGT, alkaline phosphatase) When hepatocyte markers of inflammation (e.g., AST, ALT) are increased, more advanced liver inflammation (not localized to bile ducts) Elevations in bilirubin indicate widespread and significant liver damage less common and occurs late in disease World J Gastro. 2019;25(44):6483-6494 National Cancer Institute: www.cancer.gov
CF-Associated Liver Disease Obliterative Portal Venopathy Non-Cirrhotic Portal Hypertension Lancet Gastroenterol Hepatol. 2017;2(6):446-455
Liver Complications Cystic Fibrosis-Associated Liver Disease or CFLD is common term, but what does it really mean? Newer definitions: CF Hepatobiliary Involvement (CFHBI) Advanced CF Liver Disease (aCFLD) CF LIVER DISEASE Transient Elevations in LFTs Fibrosis Focal Biliary Cirrhosis Chronic Elevations in LFTs Multilobular Cirrhosis Recommend not using the terms CFLD or CF Liver Disease Steatosis Portal Hypertension Cholecystitis Cholangitis Hepatic Stones Non-Cirrhotic Portal Hypertension Liver Failure J Pediatr Gastroenterol Nutr. 2024;78(1):153-165 Hepatology. 2023; Online, PMID: 37934656
Liver Injury Fibrosis and Cirrhosis Liver inflammation can lead to fibrosis, which can either resolve or lead to scarring (cirrhosis) Cut on skin analogy: scab can fully heal with no change in skin texture/appearance or it can leave a scar CFTR dysfunction
Portal Hypertension Can occur when liver is cirrhotic (scarred and stiff) or In non-cirrhotic portal hypertension (portal vein is stiff)
CF-Associated Liver Disease Prior Guidelines Screening Recommendations Every Visit Annually AST, ALT, GGT PT, PTT, INR Liver and Spleen Physical Exam >1.5-2x ULN, Repeat in 6 months Hepatomegaly, firm liver edge, Splenomegaly AST, ALT, GGT PT, PTT, INR Persistent Abnormality ABD US with Doppler Liver Biopsy J Pediatr Gastroenterol Nutr. 1999;28 Suppl 1:S1-13
New Recommendations for CF Hepatobiliary Complications NOTE: Recommendations are for children and adults. I am only going to cover those for children.
Screening for Hepatobiliary Complications Everyone Annual measurement of serum bilirubin, AST, ALT, alkaline phosphatase, GGT, platelet count be done at time of clinical stability Annual physical exam evaluation of liver and spleen At 3 years-old or at diagnosis Initial abdominal ultrasound of liver and spleen, and then every two years after that until reach adulthood If hepatobiliary involvement Liver elastography to screen for advance liver disease If increase in bilirubin, GGT, or alkaline phosphatase AND abdominal pain consistent with biliary cause Undergo a MRCP
Monitoring for those with Hepatobiliary Involvement or Advanced Liver Disease If hepatobiliary involvement OR advanced liver disease At every in-person exam (at least annual) liver physical exam to monitor for disease progression Annual calculation of at least one liver fibrosis index (GPR, APRI, FIB-4, Forns) Liver ultrasound at least every 2 years Annual liver elastography Every 6 months (or longer if no changes), pharmacist review of medications to evaluate for potential added risk to liver health
Monitoring for those with Hepatobiliary Involvement or Advanced Liver Disease If advanced liver disease Every 6 months Liver physical exam Labs: AST, ALT, GGT, alkaline phosphatase, direct bilirubin, albumin, platelets, INR Nutritional assessment, preferably by dietitian familiar with advanced liver disease Annually Screening for CF-related diabetes, even if <10 years-old If cirrhosis: serum AFP to screen for hepatocellular carcinoma General Multidisciplinary care with pulmonary, GI/hepatology ( transplant center), endocrinology
Treatment of Hepatobiliary Complications Medications Everyone Ursodeoxycholic acid (ursodiol) should not be used to prevent cirrhosis Not enough data to provide a recommendation on whether CFTR modulators will improve liver outcomes CFTR modulators appear to be safe and potentially other organ benefits may benefit from treatment with CFTR modulators If advanced liver disease Those with intact liver function: not enough data on safety to provide a recommendation for use of CFTR modulators Those with compromised liver function: do not recommend use of CFTR modulators Not enough evidence in CF to recommend for or against use of beta-blockers to prevent variceal bleeding
Treatment of Hepatobiliary Complications Endoscopy If advanced liver disease Not enough data to provide a recommendation on if/when endoscopy should be done in PwCF who have not had a variceal bleed For those with variceal bleeding follow standard guidelines for those without CF in consultation with pulmonologist and anesthesiologist
Treatment of Hepatobiliary Complications Surgery If advanced liver disease and portal hypertension If intact liver function: consider shunt or liver transplant If compromised liver function: liver transplant as primary intervention. Shunt can be considered to buy time If pursuing liver transplant, evaluation for possible lung-liver (individually or at same time) should be done
Take Home Points We understand more about the variety of liver complications that can occur in PwCF and we now have more tools to diagnose and monitor these complications There is still a lot we don t know, especially in regard to treatment We hope these new recommendations will improve the diagnosis of liver complications and will help PwCF be healthier for longer There will be variations at individual CF Centers based on their local capabilities. At Stanford, we have all the capabilities to fulfill the recommendations We encourage you to discuss liver health with your CF team as part of comprehensive CF care 17