Focus on Respiratory Diseases and Diagnostic Investigations in General Practice
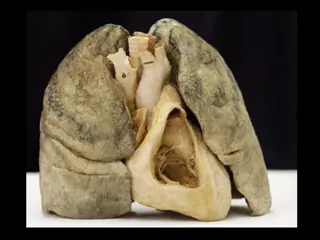
Dr. Andrew Thurston, a GP, emphasizes the importance of investigations like PEFR, spirometry, and more in the diagnosis of respiratory conditions such as asthma, COPD, and pulmonary fibrosis. The provided spirometry results for a 56-year-old woman prompt consideration of the most likely diagnosis. Spirometry is a key tool performed in GP practices for patients with chronic breathlessness and chronic cough. Additionally, guidance on when to request spirometry and considerations for performing the test are highlighted.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Focus on AKT RCGP Curriculum: Investigations: PEFR, Spirometry, Pulse Oximetry, Sputum Culture Indications for CXR, CT, MRI, Bronchoscopy Disease Scoring Tools e.g. CURB65 Conditions: - URTI, LRTI - Ephysema - PE - Asthma - Chronic Cough - Stridor / Hoarseness - Fibrosis - Use of Oxygen - Bronchiectasis - Pneumothorax - Pleural Effusion - COPD - Respiratory Malignancies - Occupational Lung Diseases - Respiratory Failure - Connective Tissue Disorders
Focus on AKT RCGP Curriculum: Investigations: PEFR, Spirometry, Pulse Oximetry, Sputum Culture Indications for CXR, CT, MRI, Bronchoscopy Disease Scoring Tools e.g. CURB65 Conditions: - URTI, LRTI - Bronchiectasis - Ephysema - Pneumothorax - PE - Pleural Effusion - Asthma - COPD - Chronic Cough - Respiratory Malignancies - Stridor / Hoarseness - Occupational Lung Diseases - Fibrosis - Respiratory Failure - Use of Oxygen - Connective Tissue Disorders
DISCLAIMER I wrote all the questions to fit with the topics They were designed to be similar to AKT questions. Please ask if anything isn t clear or looks wrong.
Question 1 A 56 year old woman presents with exertional breathlessness, worsening over 6 months. Spirometry shows: FVC 1.98 (predicted 3.51) FEV1 1.64 (predicted 2.82) FEV1/FVC 83% (predicted 80%) What is the most likely diagnosis? A) Asthma B) Bronchiectasis C) COPD D) Pulmonary Fibrosis E) Extrinsic Allergic Alveolitis
Question 1 A 56 year old woman presents with exertional breathlessness, worsening over 6 months. Spirometry shows: FVC 1.98 (predicted 3.51) FEV1 1.64 (predicted 2.82) FEV1/FVC 83% (predicted 80%) What is the most likely diagnosis? A) Asthma B) Bronchiectasis C) COPD D) Pulmonary Fibrosis E) Extrinsic Allergic Alveolitis
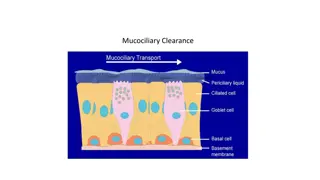
Spirometry Available at most practices Done by practice nurses Technique dependant check comments on report Patient needs to be well need to see best effort Useful in patients with: Chronic Breathlessness Chronic Cough
Requesting Spirometry in GP With or Without Reversibility? If you think it could be asthma ask for reversibility Anything else Post-Bronchodilator Spiro Is the patient capable of performing the test? Need to be able to follow instructions. Is the patient well enough? Wait 4 weeks after any chest infection
Interpreting Spirometry Obstructive Restrictive Asthma COPD e.g. Fibrosis FVC Normal or Normal or FEV1 FEV1/FVC Normal Reversibility X X Forced Vital Capacity (FVC) total vol. expired air Forced Expiratory Volume in 1 second (FEV1) Vol. Air expired in 1st second of forced expiration FEV1/FVC ratio Normal FEV1 should be >70% of FVC Reversibility = >12% improvement in FEV1
Interpreting Spirometry Example: FVC FEV1 FEV1/FVC Pre 2.67 2.80 1.48 2.24 54% 80% Predicted Diagnosis?
Interpreting Spirometry Example: FVC FEV1 FEV1/FVC Pre 2.67 2.80 1.48 2.24 54% 80% Predicted Diagnosis? Obstructive Airways Disease
Interpreting Spirometry Example: FVC FEV1 FEV1/FVC Pre 2.67 2.80 1.48 2.24 54% 80% Predicted Post 2.80 2.01 71% Diagnosis?
Interpreting Spirometry Example: FVC FEV1 FEV1/FVC Pre 2.67 2.80 1.48 2.24 54% 80% Predicted Post 2.80 2.01 71% Diagnosis? Obstructive Airways Disease with Reversibility (i.e. Asthma)
Question 2 A 66 year old man with no PMH attends with 4 days of productive cough and SOB. O/E there are crackles at the right lower zone. Temp 37.5, Pulse 86 reg, BP 100/54, RR 24, Sats 92%. He does not appear confused. Using CRB-65 score what should you do? A) CRB=1 - Manage in the community with oral antibiotics B) CRB=2 Manage in community with oral antibiotics and arrange follow up in 24 hours. C) CRB=2 Arrange admission for IV antibiotics D) CRB=3 Arrange admission for IV antibiotics E) CRB-65 score is irrelevant in this case
Question 2 A 66 year old man with no PMH attends with a productive cough and SOB. O/E there are crackles at the right lower zone. Temp 37.5, Pulse 86 reg, BP 100/54, RR 24, Sats 92%. He does not appear confused. Using CRB-65 score what should you do? A) CRB=1 - Manage in the community with oral antibiotics B) CRB=2 Manage in community with oral antibiotics and arrange follow up in 24 hours. C) CRB=2 Arrange admission for IV antibiotics D) CRB=3 Arrange admission for IV antibiotics E) CRB-65 score is irrelevant in this case
Symptoms of LRTI Cough - productive or dry - Generally lasts 7 days can linger for 3-4 weeks Sputum - Green = Dead cells -Yellow/Brown = Bacteria Breathlessness Systemic Features e.g. fever Chest Pain / Pleurisy / Abdominal Pain
CRB-65 Score for CAP NICE CKS If a person has clinical symptoms and signs suggestive of CAP, assess the severity of the illness using the CRB-65 score for mortality risk. The score is calculated by giving 1 point for each of the following prognostic features: C = Confusion (new disorientation in person, place, or time). R = Raised respiratory rate (30 breaths per minute or more). B= Low blood pressure (diastolic 60 mmHg or less, or systolic less than 90 mmHg). 65 = Age 65 years or more.
CRB-65 Score for CAP NICE CKS Scoring: 0 = Low Severity 1-2 = Intermediate Severity >2 = High Severity Management: 0-1= Community 2= Admission advised 3+= Urgent Admission Cautions: O2 Sats still need to be considered oxygen saturation below 94% indicates the need for urgent hospital admission. - NICE Mortality score doesn t always accurately predict mortality risk use clinical judgement - NICE - - -
Question 3 A 43 year old smoker with no PMH attends with a 3 day history of a cough productive of yellow sputum. He doesn t appear confused. There are crackles at the left base, Temp 38.0, Pulse 76 reg, BP 138/78, RR 16, Sats 97%. You decide he requires oral antibiotics, what would you prescribe? A) Amoxicillin 500mg TDS for 7 days B) Amoxicillin 500mg TDS + Clarithromycin 500mg BD for 7 days C) Amoxicillin 500mg TDS for 5 days D) Doxycycline 200mg single dose then 100mg OD for 4 days E) C0-Amoxiclav 625mg TDS for 7 days
Question 3 A 43 year old smoker with no PMH attends with a 3 day history of a cough productive of yellow sputum. He doesn t appear confused. There are crackles at the left base, Temp 38.0, Pulse 76 reg, BP 138/78, RR 16, Sats 97%. You decide he requires oral antibiotics, what would you prescribe? A) Amoxicillin 500mg TDS for 7 days B) Amoxicillin 500mg TDS + Clarithromycin 500mg BD for 7 days C) Amoxicillin 500mg TDS for 5 days D) Doxycycline 200mg single dose then 100mg OD for 4 days E) C0-Amoxiclav 625mg TDS for 7 days
Managing CAP Self Care rest, fluids, antipyretics Advise to STOP SMOKING No evidence for Cough Medicines Arrange a CXR for anyone over 60 and smokes BTS/NICE - high risk group for Lung Cancer (vague on timings suggests definitely needed at 6 weeks post onset but ?also at time of acute illness)
Managing CAP Prescribe Antibiotics: If CRB-65 = 0 Amoxicillin 500mg TDS for 5 days Penicillin allergy Doxycycline or Clarithromycin for 5 days Review at 3 days and increase to 7 day course if response is poor NICE If CRB-65 = 1-2 Consider Dual Therapy for 7-10 days e.g. Amoxicillin + Clarithromycin
Managing CAP NICE guide on prognosis: Explain to the person that after starting antibiotic treatment, symptoms should improve, although the rate of improvement will vary with the severity of illness. Discuss the natural history of pneumonia symptoms, that by: 1 week - fever should have resolved. 4 weeks - chest pain and sputum production should have substantially reduced. 3 months - most symptoms should have resolved but fatigue might still be present. 6 months - symptoms should have fully resolved.
Question 4 Which is the most common cause of Community Acquired Pneumonia? A) Mycoplasma Pneumoniae B) Streptococcus Pneumoniae C) Staphlococcus Aureus D) Legionella Pneumophilia E) Haemophilus Influenzae F) Viral Infections G) Pseudomonas Aeuriginosa
Question 4 Which is the most common cause of Community Acquired Pneumonia? A) Mycoplasma Pneumoniae B) Streptococcus Pneumoniae C) Staphlococcus Aureus D) Legionella Pneumophilia E) Haemophilus Influenzae F) Viral Infections G) Pseudomonas Aeuriginosa
CAP causative organisms BTS Audit No Pathogen Identified Steptococcus Pneumoniae All Viruses Haemophilus Influenzae Mycoplasma Pneumoniae Staphlococcus Aureus Legionella Pneumophilia 45.3% 36.0% 13.1% 10.2% 1.3% 0.8% 0.4%
Pseudomonas Aeruginosa You are going through your results and a sputum result comes through showing Pseudomonas. What do else do you need to know? Any chronic respiratory conditions? Why was sputum sent? How is the patient now? Any previous Sputum results? What should you do with this result? If they ve had it before and are well Nothing Never had it before Treat - speak to Micro should aim to eradicate before it colonises. Had it before and unwell Treat - speak to Micro
Pseudomonas Aeruginosa Gram Negative Rods Common in soil and standing water Opportunistic infection in humans - chest, wounds, nails, otitis externa Survivor very hard to eradicate once it has infected Leads to cycles of recurrent infection and colonisation especially in Bronchiectasis and CF Contributes to deterioration in chronic respiratory diseases e.g. Early infection if CF is a bad prognostic indicator Chronic infection is associated with worse lung function Rust coloured sputum (apparently tastes metallic) Makes nails and wounds green Only oral antibiotic option is Ciprofloxacin always speak to micro (or check Respiratory clinic letters) as may need IV IV treatment = aminoglyosides e.g. Tobramycin, Gentamycin
Question 4 A 19 year old male student has just returned home for the holidays and now attends with a 5 week history of a persistent dry cough, sore throat, and a rash. He thinks a few other students in his halls have had the same thing. He denies foreign travel and doesn t smoke. On examination his observations are all normal. His chest and throat are clear. Abdomen is SNT with no organomegaly. There is no lymphadenopathy. The rash is on the trunk and consists of raised target lesions. What is the most likely diagnosis? A) Glandular Fever B) Whooping Cough C) Atypical Pneumonia D) Tuberculosis E) Post Infective Cough
Question 4 A 19 year old male student has just returned home for the holidays and now attends with a 5 week history of a persistent dry cough, sore throat, and a rash. He thinks a few other students in his halls have had the same thing. He denies foreign travel and doesn t smoke. On examination his observations are all normal. His chest and throat are clear. Abdomen is SNT with no organomegaly. There is no lymphadenopathy. The rash is on the trunk and consists of raised target lesions. What is the most likely diagnosis? A) Glandular Fever B) Whooping Cough C) Atypical Pneumonia D) Tuberculosis E) Post Infective Cough
Question 5 A 19 year old male student has just returned home for the holidays and now attends with a 5 week history of a persistent dry cough, sore throat, and a rash. He thinks a few other students in his halls have had the same thing. He denies foreign travel and doesn t smoke. On examination his observations are all normal. His chest and throat are clear. Abdomen is SNT with no organomegaly. There is no lymphadenopathy. The rash is on the trunk and consists of raised target lesions. What is the most likely diagnosis? A) Legionella Pneumophilia B) Mycoplasma Pneumonia C) Chlamydia Psittaci (Psittacosis) D) Klebsiella E) Coxiella Burnetii
Question 5 A 19 year old male student has just returned home for the holidays and now attends with a 5 week history of a persistent dry cough, sore throat, and a rash. He thinks a few other students in his halls have had the same thing. He denies foreign travel and doesn t smoke. On examination his observations are all normal. His chest and throat are clear. Abdomen is SNT with no organomegaly. There is no lymphadenopathy. The rash is on the trunk and consists of raised target lesions. What is the most likely diagnosis? A) Legionella Pneumophilia B) Mycoplasma Pneumonia C) Chlamydia Psittaci (Psittacosis) D) Klebsiella E) Coxiella Burnetii
Atypical Pneumonia Risk Factors: Close community settings e.g. university halls, army barracks, cruise ships, schools Immunosuppression Key Features: Persistent Cough (can be productive or dry) Sore throat / Pharynigitis Recent community exposure Age <50 Clinical signs usually mild or absent Lungs look worse on CXR then they sound on examination CAP that hasn t responded to penicillin
Atypical Pneumonia BMJ Best Practice Investigations: CXR looking for consolidation Bloods - WCC, CRP, with mycoplasma can sometimes get anaemia + ALT Sputum culture I would consider doing all the above in any LRTI not responding to usual treatment Also consider (depending on history / level of suspicion) Legionella Urine Antigen Serology for Mycoplasma / Chlamydia / Coxiella
Atypical Pneumonia BMJ Best Practice Managment: 1st line Macrolide (Azithromycin / Clarithromycin) Alt 1st line Doxycycline 2nd line Fluroquinolone (Levoflocacin / Moxyfloxacin) I would think about consulting microbiology for advice
Atypical Pneumonia Mycoplasma: Community Outbreaks approx every 4 years Usually late summer / autumn Most common in children and young adults Can have associated headache Associated with various rahes usually self limiting maculopapular type classically... Erythema Multiforme Chest usually sounds clear CXR patchy consolidation Micro Sputum or Throat swabs Not a notifiable disease
Atypical Pneumonia Legionella: Standing water e.g. Air conditioning, spa pools, showers/taps. Caught from these sources rather then infected individuals. Outbreaks often in hotels, cruise ships, hospitals, nursing homes. Can be associated with Diarrhoea Legionella urine antigen negative result doesn t exclude Sputum culture Notifiable disease Psitticosis: Chlamydia Psittaci carried by birds Suspect if exposure to commercial (poultry farmers) or pet birds (parrots / budgies) Chlamydia swab of throat sputum testing is risk to Lab staff
Atypical Pneumonia Coxiella Burnetti: Associated with livestock: Farmers, Vets, Abattoir workers all at risk. Micro lab workers also at risk Usually as outbreaks with other workers affected. Usually self limiting flu-like illness but... Can cause hepatitis hepatomegaly (less common) and endocarditis (rarely). Recommendation is to treat with antibiotics for 14 days in any symptomatic patient with clinical suspicion. Serology testing is the usual diagnostic test I would discuss with micro if ever suspecting
Question 6 A 30 year old woman, originally from Somalia, attends with a 3 week history of weight loss and malaise. In last week she has noticed a mild but productive cough. She had been back to Somalia 5 weeks ago to visit a relative in hospital. Which test is most likely to be diagnostic: A) Sputum Culture for Acid Fast Bacilli B) Full blood count and CRP C) Thick blood film D) QuantiFERON E) Chest Radiograph
Question 6 A 30 year old woman, originally from Somalia, attends with a 3 week history of weight loss and malaise. In last week she has noticed a mild but productive cough. She had been back to Somalia 5 weeks ago to visit a relative in hospital. Which test is most likely to be diagnostic: A) Sputum Culture for Acid Fast Bacilli B) Full blood count and CRP C) Thick blood film D) QuantiFERON E) Chest Radiograph
Tuberculosis Mycobacterium Tuberculosis Needs specific culture medium to grow in lab and ZN staining need to ask for AFB when requesting culture Spread by droplet from people with active pulmonary TB Increasing number of cases in UK Many born outside UK in a high prevalence areas (India, Pakistan, Somalia most common) 70% of all UK cases come from the 40% most deprived areas Homeless, overcrowded conditions, prison population Other risk factors : Alcohol / Drug misuse, Comorbidities (diabetes, HIV), Immunosuppression, Previous incomplete TB treatment,
Tuberculosis Active Pulmonary TB (majority of cases 55%) Persistent Productive Cough +/- Haemoptysis Weight Loss, Fever, Night sweats Infectious Extra-pulmonary TB (rare) More likely in children from high risk areas CNS (Meningitis), Bone (Spinal = Pott s Disease), Pericarditis. Latent TB (10% of cases) No symptoms, non-infectious, Can become active often when immunocompromised Detected during screening Multi-drug Resistant TB (10% of cases on the rise) Defined as resistance to 2 first line drugs
Tuberculosis Investigations (NICE CKS) Pulmonary TB: Chest X-ray 3 x sputum cultures for AFB (at least 1 early morning) If positive refer all to respiratory TB clinic Extra-pulmonary TB: Chest X-ray depends on suspected site e.g. spine plain X-ray Latent TB Don t actively screen in primary care Refer to TB clinic if suspected contact From 2012, all people resident in a country with high TB prevalence applying for a UK visa for more than 6 months are required to have pre-entry screening
Tuberculosis Screening Tests: Tuberculin Skin Testing e.g. Heaf Test Liable to reader bias / error False positives if previous BCG vaccination QuantiFERON Interferon Gamma Release Assay detects the immune response to TB Used mainly for Latent TB diagnosis Can t differentiate between Active and Latent Disease Limitations in sensitivity and specificity mean it s not currently recommended for non-specialist use
Tuberculosis Treatment: Managed by secondary care usually Respiratory or Infectious Diseases. In Bolton TB clinic run by Respiratory Notifiable Disease in the UK Contact tracing close contacts also need treating 6 months multi-drug therapy usually Isoniazid and Rifampicin. +/- Ethambutol and Pyrazinamide TB nurses keep regular contact to ensure compliance biggest cause of treatment failure, multi-drug resistance, and risk of spreading TB
Question 7 Following a positive sputum AFB, you referred the 30 year old Somali woman to Respiratory, who confirmed the diagnosis and started treatment for TB. She has been on treatment for 2 months and returns to see you complaining of reduced vision. Which drug is most likely to be responsible? A) Ethambutol B) Rifampicin C) Isoniazid D) Pyrazinamide E) Not likely to be a drug side effect
Question 7 Following a positive sputum AFB, you referred the 30 year old Somali woman to Respiratory, who confirmed the diagnosis and started treatment for TB. She has been on treatment for 2 months and returns to see you complaining of reduced vision. Which drug is most likely to be responsible? A) Ethambutol B) Rifampicin C) Isoniazid D) Pyrazinamide E) Not likely to be a drug side effect
TB Drug Side Effects Ethambutol Visual disturbance Peripheral Neuropathy (common) Hyperuricaemia (Gout flares) Isoniazid Peripheral Neuropathy (common) Liver Failure (rare) Pyrazinamide Hyperuricaemia (Gout flares) Rifampicin Turns secretions orange will stain soft contact lenses and clothing Thrombocytopoenia Nausea / Vomiting
TB Drug Side Effects Essentially: If a patient on TB treatment presents with any of; Peripheral Neuropathy Visual Disturbance Acute Gout Flare Deranged LFTs Suspect the TB drugs as a cause and advise the patient to inform their TB clinic urgently. Don t stop any TB treatment without consulting the specialist first
Asthma Key Features Symptoms: - Wheeze - Cough - Chest Tightness - Breathlessness Quality of the Symptoms: - Episodic - Diurnal Variation (worse at night or early morning) - Triggered by e.g. exercise, allergens. infection, cold air Other Associations: - Family History - Atopic Eczema, Allergic Rhinitis - Occupation Lab work, baking, animals, welding, paint spraying - Drugs e.g. NSAIDs and Beta Blockers