Respiratory Assessment
Conducting a thorough respiratory assessment is crucial in detecting early signs of deterioration in patients. This guide covers the key aspects of respiratory assessment, including assessing breathing, identifying different types of hypoxia, indications for assessment, pulse oximetry, visual and tactile examinations, and more.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Respiratory Assessment Nurse Practitioner Led Outreach Team (NLOT) 2022 William Osler Health System | Ontario Health Team
Respiratory Assessment Breathing is usually the first vital sign to alter in a deteriorating patient Purpose of assessment to determine the adequacy of gas exchange (O2& CO2) Ventilation(air movement) Diffusion(gas exchange between lung and RBC) Perfusion (delivery to RBC) Respiratory rate and depth are controlled by the respiratory center in the brain stem
Hypoxia Anaemic: Reduced Hgb or Carbon Monoxide poisoning Hypoxic: Reduced gas exchange in the lungs Circulatory: Reduced blood supply Histotoxic: Inability of tissues to use oxygen
Respiratory Assessment Indicated: Initial assessment, changes from baseline, fluids, response to medications or treatments, patients with respiratory conditions Vitals with oxygen saturation History, baseline respiratory status Medications (treat symptoms, induce symptoms) Is there pain Are there other system changes Ex. Neurological, abdominal, etc. Blood Sugar Look, feel and listen
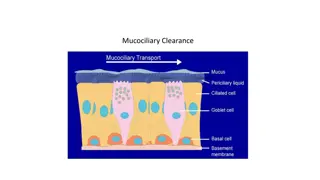
Pulse Oximetry Uses probe to transmit light through tissue Pulse oximetry can be unreliable when: Peripheral vasoconstriction (shock) Excessive movement Artificial nails or nail polish Carbon monoxide poisoning (will register as 100% SpO2)
Look Depth of breathing (shallow, normal, deep) Respiratory rate Pattern (regular vs laboured) Movement (symmetrical vs asymmetrical) Abnormal Pursed lips, nasal flaring, accessory muscle use, cyanosis, clubbed fingers Is there a cough? Sputum (note quantity, colour) Level of consciousness (alert vs depressed) Confusion Tracheal deviation
Feel Chest movement (symmetrical vs asymmetrical) Lightly place hands on each side of the chest wall, thumbs together at midline. Thumbs should move apart on inspiration and fall back together on expiration.
Listen Distinguish between normal and abnormal Breathing should be quiet Listen with diaphragm of the stethoscope from side to side, top to bottom https://www.nursingtimes.net/clinical-archive/assessment-skills/how-to-perform-chest- auscultation-and-interpret-the-findings-06-01-2020/
Normal Auscultation https://www.nursingtimes.net/clinical-archive/assessment-skills/how-to-perform-chest-auscultation-and- interpret-the-findings-06-01-2020/
Abnormal Sounds Include: crackles/rales, wheezes and rhonchi Caused by: Consolidation of secretions, compression or airway (mass), pleural effusion, collapsed lung Absent, diminished or adventitious breath sounds
Crackles/Rales Due to atelectasis or fluid in the small airways Heard on inspiration possible pulmonary edema or pneumonia More significant if not cleared with coughing Can be fine or coarse
Wheezing High pitched whistling Can occur with inspiration or expiration, but usually more pronounced on expiration Occurs with airway narrowing
Rhonchi Resembling a snoring or gurgling sound Suggests secretions in large airways
Cardiac Assessment Also important to perform a cardiac assessment including: Blood pressure and heart rate Heart rate: regular vs irregular Peripheral edema
Oxygen Humidify oxygen when greater than 4L/min or if into a tracheostomy tube CAUTION with COPD Excessive supplemental O2 removes a COPD s residents hypoxic respiratory drive hypoventilation carbon dioxide levels, apnea (pauses in breathing) ultimately respiratory failure CO2 retention = hypercapnia
Nebulizers Turns liquid medication into a mist Use saline to dilute NOT water RINSE mouth after antibiotics/steroids to avoid oral candidiasis Used when: Residents who have difficulty controlling and coordinating the use of inhalers (acutely ill, dementia) Inhalers are found to be ineffective in managing chronic lung disease or respiratory symptoms
Inhalers Short acting beta2-adrenorecptors agonists: Salbutamol (Ventolin) Long Acting beta2 agonists: Salmeterol (Serevent) Inhaled Steroids: Flovent Anticholinergics: Strovent, Spiriva If using more than one, short acting bronchodilator should be administered first Spacing devices, masks, or nebulisation if trouble with administration
Suctioning Used to help clear airways Used in residents who are too weak to expectorate sputum, unconscious or semi-conscious Can be done through tracheal, oral or nasal pharyngeal
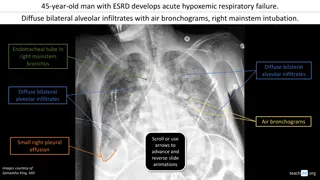
Chest X-Ray Used for suspected pneumonia, pleural effusion and/or cardiac disease https://www.kaggle.com/datasets/paultimothymooney/chest-xray-pneumonia
COPD Exacerbation Cardinal Symptoms: Increased dyspnea Increased sputum volume Increased sputum purulence Please note: Presentation with only one of the cardinal symptoms may not require antibiotics
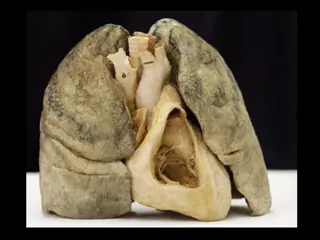
Pneumonia Infection and associated inflammation of the lungs Viral vs bacterial vs aspiration vs retention of lung secretions PEARLS: Always rule out aspiration in the setting of repetitive pneumonia
Antibiotics Considerations in choosing agent and dose selection: Antibiotics used in the past 3 months Updated Creatinine Clearance Is the resident on Coumadin Are there any allergies?
Case Study #1 85 year-old female PMHx of Diabetes Type II, Hypertension, Osteoporosis Vitals signs: RR 24bpm, B/P 110/70, HR 97bpm, T 37.5, SpO2 91% on R/A Non-productive cough No shortness of breath Chest sounds:
Case Study #2 78 year-old male PMHx of Benign Prostatic Hyperplasia, Hypertension, Hypothyroidism, COPD, Anemia, Arthritis Vitals signs: RR 28bpm, B/P 125/77, HR 105bpm, T 37.0, SpO2 88% on R/A Cough and shortness of breath present Chest sounds:
References Bennett, C. (2003). Nursing the breathless patient. Nursing Standard, 17(1): 45-51. Bickley, L., & Szilagyi, P. (2003). Bates Guide to Physical Examination and History Taking. Lipincott Williams & Wilkins, Philadelphia. Bradley, R. (2007). Improving Respiratory Assessment Skills. The Journal for Nurse Practitioners, 4: 276-277. Endacottt, R., & Jenks, C. (1997). Respiratory Assessment in A&E. Emergency Nurse, 5(4): 31-38. Ferns, T. (2007). Respiratory Auscultation: How to use a Stethoscope. Nursing Times, 103(24): 28-29. Hunter, J., & Rawlings-Anderson, K. (2008). Respiratory Assessment. Nursing Standard, 22(41): 41-43. Owen, A. (1998). Respiratory Assessment Revisited. Nursing, 4: 48-49.