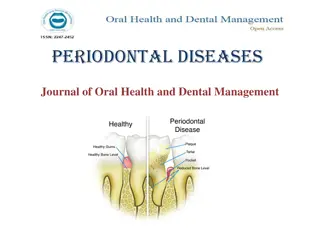
Periodontal Treatment Considerations for Medically Compromised Patients
Patients with significant medical conditions may require special considerations for periodontal treatment. Medical issues such as hemorrhagic disorders, renal diseases, liver diseases, pulmonary diseases, infectious diseases, pregnancy, medications, and cancer therapies can impact oral health and treatment outcomes. It is essential for clinicians to identify and address these medical concerns through thorough health history assessments, clinical examinations, and laboratory tests to provide safe and effective periodontal care.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
PERIODONTAL TREATMENT OF MEDICALLY COMPROMISED PATIENTS PRESENTED BY: KURESHI NAVAL ANJUM
WHAT THE PERIODONTALTREATMENT HAS TO DO WITH THE MEDICALLY COMPROMISED PATIENTS? Many patients seeking dental care might have significant medicalconditionwhichmay alter the course of their oral disease and therapy provided. The therapeutic responsibility of clinician includesidentificationof medicalproblems andconsultationwithorreferral of the patient toappropriatephysician maybe indicated.
Hemorrhagicdisorders Renaldiseases Liverdiseases Pulmonarydiseases Infectiousdiseases Pregnancy Medicationsandcancertherapies Prostheticjointreplacement.
HEMORRHAGIC DISORDERS...........!!!! . ,
Patients with a history of bleeding problems caused by the disease or drugsshould bemanaged tominimize risksof hemorrhage. Identificationof thesepatientscan be donebythefollowing methods: 1)Healthhistory 2) Clinicalexamination 3) Laboratorytests
1) HEALTH HISTORY Thehealthquestioningshouldcover 1) Historyof bleedingafterprevious surgeryortrauma 2)Past and present drug history (drugs thatinterferewith hemostasis are: aspirin,anticoagulants,alcohol,anticancer drug,antibiotics)
3) illnessesassociatedwithpotential bleedingproblems: Generalized hemostaticdefectorlocaldefect bleeding from multiplesites,spontaneousor excessivebleedingafterinjury Inherited defectoracquired
Is bleeding suggestive of vascular, platelet or coagulation disorder ? Vascular/plateletdisorders easy bruising,spontaneousbleeding fromsmallvessels especiallyintoskin (purpuraandecchymosis) Coagulationdisorders hemarthrosis,musclebleeds, bleedingafterinjuryorsurgery.
History of bleeding problems among relatives to know whetheritisgenetic in nature Medical history Liver disease Renal disease Malignancies Poornutrition(vitkorcdeficiency)
Ecchymoses Petechiae Hemarthrosis Epistaxis GI bleeding Softtissuebleeding
3) LABORATORY TESTS Itincludes : Bleedingtime Prothrombin time (PT) Partial thromboplastin time (PTT) Complete blood cell count(CBC) Tourniquet test Coagulation time
PT measuresextrinsicand commonpathways (factors I,II,VII and X) Normal INR = 1 Abnormal INR > 1.5 PTT measuresintrinsicandcommonpathways (factorsIII,IX,XI,I,II,V,X,XII) Normal : 25 -40 secs abnormal : >1.5 timesnormal Plateletcount(normal 1,50,000 3,00,000 / mm ) Bleeding time(normal 1 to6 minutes) 3
Well!!Nowits timefor the confirmation..Let s hope for the best result.. Findings causes Peripheral destruction of platelets,abnormal bone marrow production Platelet count Abnormal bleedingtime Aspirin or NSAID therapy Liverdisease,Vonwilebrand disease,DIC,acuteleukemia Abnormal aPTT Oneof the hemophiliac states Abnormal PTwith or without abnormal aPTT Abnormal reduction in the vit k dependent clotting factors (factors II,VII,IX,X)or factor V Presenceof more than 10petechiae Thrombocytopenia
HEMORRHAGIC DISORDERS Itcan beclassifiedas Coagulationdisorders(inherited oracquired) Disorderof vessels Disorderof platelets(quantityorfunction)
TYPE (inherited) PROLONGED NORMAL TREATMENT Hemophilia A (deficiency of factor viii) PTT PT Bleedingtime DDAVP(Desmopressin)factorVIIIconcentrate Freshfrozen plasma Freshwhole blood Tranexamicacid, eaminocaproic acid (amicar) Hemophilia B (deficiency of factor ix) PTT PT Bleedingtime Purified prothrombin complex concentrates Factor IXconcentrates Freshfrozen plasma Von willebrand s disease (deficiency of vonwillebrand factor) PTT Bleeding time Variable factor VIII deficiency PT Platelet count DDAVPFactor VIII Concentrate or cryoprecipitate
Acquiredtype Liverdisease Renaldisease Anticoagulanttherapy Disseminated intravascularcoagulation Vitkdeficiency
TREATMENT: Probing,scaling,prophylaxiscan bedonewithout medical modification. More invasive treatment such as local block anesthesia, rootplaningorsurgeryrequireprior physicianconsultation. Completewoundclosureand applicationof pressure will reducehemorrhage. Antihemostaticagentssuchasoxidized celluloseor purified bovinecollagen maybeplacedoversurgical sitesorextractionsockets.
FOR PATIENTS UNDER ANTICOAGULANT MEDICATION: Theeffectivenessof anticoagulationtherapyisdetermined bythePT laboratorytest. Therecommended levelof therapeuticanticoagulation for most patients is an INR of 2 to 3, with prosthetic heart valves itis intherangeof 2.5 to3.5 INR lessthan 3 infiltrationanesthesia,scaling,root planing . INR lessthan 2 to2.5 blockanesthesia, minor periodontalsurgery,simpleextractions INR lessthan 1.5 to2 complexsurgeryormultiple extractions
FOR PATIENTS UNDER ANTI PLATELET MEDICATION : Aspirinupto325 mg perday noneed todiscontinue themedication beforeperiodontalprocedures Aspirin more than 325 mg per day should discontinuethetherapy7 to10daysbeforesurgical procedures.
Thrombocytopenic purpura Thrombocytopeniaisdefined asaplateletcountof less than 100000/mm3 It may be seen in the cases of radiation therapy,chemotherapy,leukemiaorinfections Purpurasarehemorrhagicdiseasescharacterised by theextravasationof blood intothetissuesunderthe skin or mucosa producing petechiae (small red patches)orecchymoses(bruises)
Periodontal therapyforpatientswiththrombocytopenicpurpura Removalof local irritants Oral hygieneinstructionsand frequentmaintenancevisits 1 Scalingand rootplanningaresafe(plateletcountshould not belessthan 60,000/mm3) 2 Local hemostatic measuresshould beapplied Nosurgical procedures should bedoneuntil theplatelet countof morethan 80000/mm3 Platelettransfusionmayberequired beforesurgery 3
Non thrombocytopenic purpura Itisduetoeithervascularwall fragilityor thrombasthenia Causes: Vascularwall fragility scurvy,infections,chemicals (phenacetin,aspirin),dysproteinemia Thrombasthenia vonwillebrand sdisease,aspirin ingestion,uremia
TREATMENT: Directpressureapplied foratleast15 minutes Surgicaltherapyshould beavoided
LEUKEMIA Leukemia is a malignant progressive disease in which the bone marrow and other blood forming organs produceincreased numbersof immatureorabnormal leucocytes The treatment plan is based on the effects of chemotherapy,bleeding tendency,susceptibility to infections
TREATMENT: Referthepatientformedicalevaluationand treatment Monitorhematologiclaboratoryvaluessuchas bleeding time,coagulation time,PTand plateletcount Administerantibioticcoverage beforeanyperiodontal treatment Extractall hopeless, potentiallyinfectiousteethatleast 10 daysbeforechemotherapy(if systemicconditionsallow) Scaling,rootplaning should beperformed Topical hemostaticagentscan beused Twicedailyrinsingwith 0.12% chlorhexidine gluconateis recommended afteroral hygieneprocedures
ACUTE LEUKEMIA : Antibiotictherapycombinedwith nonsurgicalor surgicaldebridementis indicated. CHRONICLEUKEMIA : scalingand rootplaningcan beperformed . periodontalsurgeryshould beavoided.
AGRANULOCYTOSIS Itincludesthecyclicneutropeniaand granulocytopenia Early,severeperiodontaldestruction Periodontal treatmentshould bedoneduring periods of diseaseremission Treatmentshould beasconservativeaspossible Scaling,rootplaning should beperformed under antibioticprotection Extractioncan bedoneafterconsultationwiththe physician
Mostcommoncauses of renal failureare: Glomerulonephritis Kidneycysticdisease Renovascular disease Drug nephropathy Obstructiveuropathy hypertension
Renal failure may result in : Severeelectrolyteimbalances Cardiacarrhythmias Pulmonarycongestion Congestiveheartfailure Prolonged bleeding The patient in chronic renal failure has a progressive disease that ultimately may require dialysis or kidney transplantation.So , it is preferable to treat before ,rather than after .transplant or dialysis.
ORAL MANIFESTATIONS OF RENAL DISEASE Halitosis Alteredtastesensation Xerostomia Gingivitis Enamel hypoplasia Infections
TREATMENT: Consultthepatient sphysician MonitorBlood Pressure(patientsinendstagerenal failureare usuallyhypertensive) Check laboratory values : PTT,PT,bleeding time,platelet count,blood ureanitrogen(donottreatif <60 mg /dl) andserum creatinine(do nottreatif <1.5 mg /dl) Periodontal treatmentshouldaimateliminating inflammation or infection and frequent recall appointments should be scheduled Drugsthatarenephrotoxicormetabolized bythekidneyshould notbegiven (eg: tetracycline,aminoglycosideantibiotics) . Acetaminophenmay beused foranalgesia,diazepam maybe used for sedation . Local anesthetics such as lidocaine are generallysafe
Thepatientswhoarereceivingdialysisrequires modification intreatmentplaning Modesof dialysis: 1].Intermittent Peritoneal Dialysis (IPD) 2].Chronicambulatoryperitonealdialysis (CAPD) 3].Hemodialysis
RECOMMENDATION FOR HEMODIALYSIS: Screen for Hepatitis B and C antigens antibodybefore any treatment. Provideantibiotic prophylaxis. Periodontal treatment should be providedon thedayafter dialysis due to theeffects of heparinization. Becareful toprotect the hemodialysis shunt or fistula whenthepatientisindentalchair. If theshuntorfistula isplaced in the arm do not cramp that limb and do not use that limb for injectionof medication. BPreadingshould betaken from theotherarm. Patients with leg shunts should avoid sitting with the leg dependentformorethan1 hour
RECOMMENDATION FOR RENAL TRANSPLANTPATIENT HepatitisBand Cscreening Determination of level of immunesystem compromise resulting from anti rejectiondrug therapy Prophylactic antibiotics (using AHA recommendationsor specific regimens based on physician consultation)
LIVER DISEASES
Liver is the site of production for most of the clotting factors,excessivebleedingduringorafterperiodontal treatment may occur in patients with severe liver disease Manydrugsaremetabolized intheliver. Sotheliver diseasealtersthenormaldrug metabolism
Majorcausesof liverdiseasesincludes: Drug toxicity Cirrhosis Viral infections(hepatitisBand C) Neoplasms Biliarytractdisorders
ORAL MANIFESTATIONS OF LIVER DISEASE Candidiasis Angularcheilitis Atropicglossitis Petechiae Lichenplanus
TREATMENT : Consultation with the physician concerning current stage of disease, risk forbleeding,potentialdrugstobeprescribed during treatmentand requiredalterationstoperiodontal therapy. Screening forhepatitisBand C Check laboratoryvaluesforPTand PTT Check laboratoryvaluesforINR Teeth with severe bone and attachment loss, furcation invasion, periodontal abscesses or extensive surgical requirements should beextracted beforethetransplantprocedure Conservative,nonsurgical periodontaltherapycan bedone wheneverpossible If surgeryisrequired INR should belessthan 2 Plateletcountshould bemorethan 80,000/mm3
Pulmonary diseases
Pulmonary diseases range from obstructive lung diseases (eg: asthma,emphysema,bronchitis) to restrictive ventilatory disorders caused by muscle weakness,scarring,obesityoranyconditionthatcould interferewitheffectiveventilation Acuterespiratorydistressmaybecaused byslight airway obstruction or depression of respiratory function. Patients with acute respiratory distress might alter theirpositioninattemptstoimprovetheirventilatory efficiency
ORAL MANIFESTATIONS : Xerostomia Gingivitis Halitosis Candidiasis
TREATMENT: Identify and refer patients with signs and symptoms (increased respiratory rate,cyanosis,,clubbing of the fingers,chronic cough,chest pain,hemoptysis,dyspnea andwheezing) of pulmonarydiseasetotheirphysician regarding medications (antibiotics,steroids,chemotherapeuticagents)and severityof pulmonarydisease
Avoid elicitationof respiratorydepressionordistress : Minimizethestressof aperiodontalappointment.patientwith emphysema should be treated in the afternoon ,several hours aftersleeptoallowforairwayclearance. Avoid medicationsthatcould causerespiratorydepression (e.g. : narcotics,sedativesorgeneralanesthetics). Avoid bilateral mandibularblockanesthesiawhichcould cause increasedairwayobstruction Positionthepatienttoallow maximalventilatoryefficiency,keep thepatient sthroatclearandavoidexcessperiodontal packing Do notuseequipmentsthatproduceaerosols. eg: ultrasonicscalers.
Forasthmaticpatient inhalershould beavailable Infectiouspatientsshould notbetreated unlessthe periodontal procedureisanemergency