Heart Failure: Challenges and Strategies for Optimizing Care
Heart failure is a prevalent clinical syndrome with significant impact on healthcare systems. With rising prevalence and costs, optimizing disease management through timely interventions, specialized care, and community support is crucial for improving patient outcomes and reducing hospital admissions and readmissions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Sukhan Wilkins Lead Heart Failure Nurse, ACERS
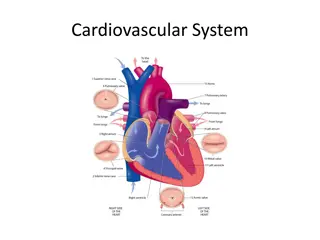
Clinical syndrome that results from any structural or functional cardiac disorder that reduces the ability of the heart to function as a pump Around 1-2 million people in UK have HF Increasing prevalence; CHD and hypertensive heart disease, aging population Costs NHS around 625m per year, accounts for 5% of medical admissions to acute care Half of service users admitted with HF are readmitted within 3 months (NICE 2010).
MI CHD Congenital heart disease Age HTN Diabetes BMI Smoking Elevated LDL Alcohol Sleep apnoea AF Ethnicity Gender
Recorded prevalence of HF in London 0.32- 0.75%, national average 0.79% City and Hackney 1879 patients with heart failure on GP practice registers, prevalence rate 0.6% (2014/15 QOF) Average cost of echocardiography 135 BNP testing recommended by NICE as cost effective tool for diagnosis (costing average 30 per test).
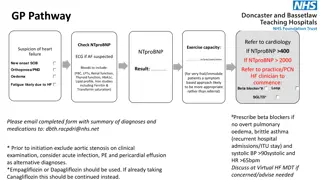
Level does not differentiate between HFpEF and HFrEF <400ng/L in those untreated means HF diagnosis unlikely 400-2000ng/L; refer for specialist assessment and echo within 6 weeks >2000ng/L ;within 2 weeks Obesity, Afro-Caribbean origin and HF meds can reduce BNP Age >70, LVH, ischaemia, tachycardia, CKD, COPD, diabetes, cirrhosis liver can raise BNP.
Average HF admission costs 3796* Effective community care known to reduce admission rates In London, 56% of patients are referred to HF nurse service, 18% referred for cardiac rehab*. *London Clinical Network/NHS England 2018
Optimising disease modifying meds in timely manner, under close monitoring More people feeling supported to self manage condition, less anxious and more in control, accessible & personalised information/advice Multidisciplinary specialist care Greater levels of access to appropriate services Fewer inappropriate hospital admissions and readmissions.
Nurse led service, integrated with ACERs team Cardiorespiratory nurse consultant, lead HF nurse, 4 community HFSN, 1 inpatient HFSN, 1 cardiorespiratory assistant practitioner, 1 admin assistant Care delivered via GP based clinics, St Leonards, Homerton and Fountayne Road Health Centre, home visits for housebound 9-5, Monday to Friday, excluding bank holidays.
Adults registered with a City and Hackney GP, or resident but not registered with any GP All patients should have confirmed diagnosis of heart failure by echo and raised NT-proBNP if done Aged 18 and over.
New diagnosis Difficult to control symptoms Following hospital admission for HF Referrals accepted from all primary, community & secondary HCPs, and via eRS (choose and book).
HFrEF - optimise evidence based HF medication as per guidelines HFpEF - follow cardiologist management plan to treat symptoms, manage co-morbidities Link to cardiologists at HUH, weekly meeting to discuss management complex patients Refer for device therapy Decompensation unable to be managed safely in community, arrange hospital admission through inpatient HF nurse Work closely with wider MDT, including respiratory, oxygen, CR, psychology, palliative teams.
1 hour assessment to include education, tailored self care and lifestyle advice Consultations entered direct on EMIS same day, any action required communicated to GP within 24 hours Recognise/explore intentional and non- intentional non-adherence and liaise with primary care team.
Declines service or failure to respond Non compliant with treatment and full mental capacity Preference is expressed to attend GP for ongoing management Repeated DNAs When stable, and optimised on anti-heart failure medications Discharged patients can self refer if HF decompensates, and our advice/input is required NICE guidelines recommend heart failure register at surgery and 6 monthly follow ups.
SHIFT trial Reduces mortality/hospitalisation of symptomatic patients EF 35% or below, HR 75 bpm or above, on maximum tolerated BB Slows HR through inhibition of If channel in the sinus node Should only be used in SR.
NYHA II to IV and LVEF 35% or less In SR, HR 75bpm or more despite treatment with beta blocker, or unable to tolerate/contraindicated Initiated by HF specialist with access to MDT HF team Dose 2.5mg to 7.5mg bd.
Paradigm-HF trial, reduction in all cause mortality and hospitalisation Sacubitril = Neprilysin Inhibitor (ARNI) Natriuretic peptides (A and B type) inhibit renin and aldosterone release Neprilysin degrades natriuretic peptides As Sacubitril inhibits Nelprilysin, levels of these peptides increase, resulting in diuresis, natriuresis, myocardial relaxation, vasodilation and reduced remodelling.
LVEF 35% or less Symtomatic despite taking stable dose ACEI or ARB (NTHA II-IV) Concomitant use of ACEI contraindicated, must be stopped and have 36 hr washout period prior to commencing Initiated under specialist guidance Dose 24/26mg, 49/51mg or 97/103mg, bd.
LVEF 35% or less Treatment options depend on NYHA class, QRS duration and presence of LBBB LV electrical dyssynchrony contributes to cardiomyopathy and symptoms Synchronised biventricular pacing can lead to increased stroke volume, reverse remodelling.
No treatment has been shown convincingly to reduce morbidity or mortality Manage co-morbidities Diuretics usually improve symptoms Evidence for ARB/ACEI, MRA and BB to improve symptoms and mortality is lacking.