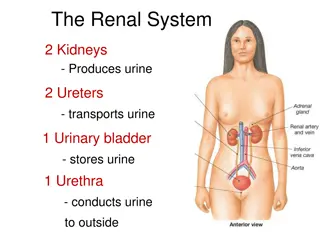
Pathology of the urinary system
Focal segmental glomerulosclerosis (FSGS) is characterized by sclerosis of some glomeruli, while membranous nephropathy (MN) involves subepithelial immunoglobulin deposits. FSGS can lead to end-stage renal disease, with poor response to corticosteroid therapy. MN, on the other hand, shows diffuse capillary wall thickening and is associated with various secondary causes. Both conditions have distinct clinical courses and pathological features.
Download Presentation
Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
Presentation Transcript
Pathology of the urinary system Dr.Mohanad Al-Hindawi lecture two
Focal segmental glomerulosclerosis (FSGS) is characterized by sclerosis of some (but not all) glomeruli that involves only a part of each affected glomerulus Primary cases or Secondary to HIV infection (HIV nephropathy), Heroin abuse (heroin nephropathy) or Secondary to other forms of GN (e.g., IgA nephropathy), to nephron loss and hereditary defects in Podocin Primary FSGS accounts for approximately 20% to 30% of all cases of the nephrotic syndrome Etiology: injury to podocytes (unknown mechanisms) severe enough to cause proteins and lipids to deposit focally Hyalinosis eventual sclerosis
Morphology of FSGS 1. segment of glomerulus affected 2. Capillaries lost 3. Matrix material accumulated 4. With time all the glomerulus affected (global sclerosis)
Clinical course of FSGS It is important to distinguish FSGS from minimal-change disease because the clinical courses and responses to therapy are markedly different(both present with nephrotic syndrome and are due to podocyte injury) FSGS-associated proteinuria is nonselective the response to corticosteroid therapy is poor. 50% of patients with FSGS develop end-stage renal disease within 10 years of diagnosis.
Membranous nephropathy characterized by subepithelial immunoglobulin-containing deposits along the GBM (autoimmune response). well-developed cases show diffuse thickening of the capillary wall adults between the ages of 30 and 60 years and follows an indolent and slowly progressive course. Up to 80% of cases of membranous nephropathy are primary
Secondary MN 1. Infections (chronic hepatitis B) 2. Malignant neoplasms, particularly carcinoma of the lung and colon 3. SLE 4. Drugs (penicillamine, captopril, nonsteroidal anti-inflammatory agents) Dome and spikes in membranous nephropathy
Pathognesis : a form of chronic immune complex glomerulonephritis, antibodies reacting in situ to endogenous or planted glomerular antigens podocyte injury and proteinuria Morphology: The main histologic feature of membranous nephropathy is diffuse thickening of the capillary wall on routine H&E stains Electron microscope: subepithelial deposits separated by spike-like protrusions from GBM (spike and dome pattern) Immunofluorescence microscopy shows typical granular deposits of immunoglobulins and complement along the GBM
Clinical course of membranous nephropathy 40% progress to renal failure over variable time (2-20years) Nephrotic syndrome: non- selective proteinuria, poor response to corticosteroids
Membranoproliferative Glomerulonephritis(MPGN) MPGN is manifested histologically by alterations in the GBM(membrano-) and mesangium and by proliferation of glomerular cells(proliferative-) 5% to 10% of cases of idiopathic nephrotic syndrome in children and adults Some patients present with combined nephrotic and nephritic syndromes Tow types : Type I MPGN( more common) and dense deposit disease Type I: deposition of circulating immune complexes or by in situ immune complex formation
Morphology and course of MPGN I large glomeruli Hypercellular glomeruli(proliferation of cells and leukocytes infiltration) thickened GBM, duplicated GBM tram track appearance electron microscope: subendothelial deposits of C3 and IgG..etc 40% progress to renal failure, others persistent nephrotic syndrome and variable renal insufficiency (poor outcome)
Acute Post-infectious (Post-streptococcal) Glomerulonephritis Acute postinfectious GN is caused by glomerular deposition of immune complexes resulting in the proliferation of and damage to glomerular cells and infiltration of leukocytes, especially neutrophils. Several infectious microorganisms other than streptococci can cause it(bacteria: pneumococci , viruses: mumps, measles ..etc) The typical case of post-streptococcal GN develops in a child 1 to 4 weeks after he or she recovers from a group A - hemolytic streptococcal infection of the pharynx or skin
By light microscopy, the most characteristic change in postinfectious GN is increased cellularity of the glomerular tufts that affects nearly all glomeruli hence the term diffuse GN Electron microscopy: deposited immune complexes arrayed as subendothelial, intramembranous, or, most often, subepithelial humps nestled against the GBM(without spikes) Immunofluorescence description: "bumps and humps" (granular) deposition
The most common clinical presentation is acute nephritic syndrome Edema and hypertension are common, with mild to moderate azotemia. Urine is typically smoky brown rather than bright red due to oxidation of hemoglobin to methemoglobin. serum anti streptolysin O antibody titers are elevated in post-streptococcal cases Recovery occurs in most children with post- streptococcal disease, but some develop rapidly progressive GN owing to severe injury with the formation of crescents, or chronic renal disease from secondary scarring
IgA Nephropathy IgA nephropathy is one of the most common causes of recurrent microscopic or gross hematuria and is the most common glomerular disease worldwide affects children and young adults and begins as an episode of gross hematuria that occurs within 1 or 2 days of a nonspecific upper respiratory tract infection. Typically, the hematuria lasts several days and then subsides, but it recurs periodically, usually in the setting of a viral infection
Pathogenesis: abnormal form of IgA attack and bind with normal IgA in the blood then the complex deposited in the mesangium Genetic predisposition is thought to exist, with increased synthesis of IgA in response to infections IgA nephropathy is sometimes associated with celiac disease The characteristic immunofluorescence picture is of mesangial deposition of IgA Variable clinical course, some patients (25-50%) progress over 20 years to end-stage renal disease
Rapidly Progressive Glomerulonephritis (crescentic GN) RPGN is characterized by the presence of crescents (crescentic GN) and in most cases appears to be immunologically mediated It is a clinical syndrome and not a specific etiologic form of GN RPGN is characterized by rapid loss of renal function, laboratory findings typical of the nephritic syndrome, and often severe oliguria. If untreated, it can rapidly lead to renal failure within a period of weeks to months.
causes 1. Anti-GBM antibody mediated crescentic GN (Goodpasture disease) 2. Immune complex mediated crescentic GN: complicate other glomerular diseases(poststreptococcal GN, systemic lupus erythematosus, IgA nephropathy) 3. Pauci-immune type crescentic GN is defined by the lack of anti-GBM antibodies or significant immune complex deposition. Prognosis: some patients require dialysis or transplantation others benefit from plasma exchange( Goodpasture disease)
Morphology of RPGN The glomeruli show cellular proliferation outside the capillary loops. These distinctive proliferative lesions outside the capillary loops are called crescents owing to their shape as they fill Bowman s space. Crescents are formed both by the proliferation of epithelial cells and by migration of monocytes/macrophages into Bowman s space