Assessment of Epidemiological Capacity in 27 Big Cities: Key Findings and Implications
Delve into the recent assessment of epidemiological capacity in 27 major cities, with insights from experts Jessica Arrazola, Chrissie Juliano, and Meghan McGinty. Explore the objectives, results, and unique aspects of the assessment, shedding light on strategies to enhance public health service delivery and data availability at the local level. Acknowledgments and details about BCHC and CSTE enrich the discussion, providing a comprehensive overview of the vital work being done in these urban centers for community health and equity.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Assessing Epi Capacity in 27 Big Cities: Results from a Recent Assessment & Implications for Practice Jessica Arrazola, DrPH, MPH, CHES (Senior Program Analyst, CSTE) Chrissie Juliano, MPP (Director, BCHC) Meghan McGinty, PhD, MPH, MBA (Deputy Director, BCHC)
Outline of Session Outline of Session Who are BCHC and CSTE? What is the ECA? Overview of BCHC results Overview of state results Interesting differences between BCHC and state Q/A discussion
Acknowledgements CSTE would like to acknowledge and thank our colleagues for their support and guidance on the project: Nancy Binkin, Beth Daly, Rich Danila, Jeff Engel, Aaron Fleischauer, Bob Harrison, Sara Huston, Mia Israel, Chrissie Juliano, Becky Lampkins, Jennifer Lemmings, Meredith Lichtenstein Cone, Amanda Masters, Joe McLaughlin, Meghan McGinty, Dhara Shah, Kathy Turner, Patty Quinlisk, Sharon Watkins, BCHC, and the NACCHO local epidemiology workgroup. This project was supported in part by CDC cooperative agreement numbers 5U38OT000143-04 and 5U38OT000143-05. The contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC. BCHC also thanks its foundation funders and Members for enabling and supporting our participation in this work.
Learning Objectives Learning Objectives 1. Compare innovative ways to structure local public health departments that maximize resources to enhance service delivery to the community 2. Describe approaches to refining and developing sub- county measures and metrics to enhance local data availability and unmask health gaps.
About BCHC About BCHC Founded in 2002 Operated out of NYC until 2012 when it moved to NACCHO Mission: Advancing equity and health for present and future generations Vision: Healthy, more equitable communities through big city innovation and leadership
30 Member Cities 30 Member Cities Austin Baltimore Boston Charlotte (Mecklenburg Cty) Chicago Cleveland Columbus Dallas Denver Detroit Fort Worth (Tarrant Cty) Houston Indianapolis (Marion Cty) Kansas City Las Vegas (S. NV Hlth District) Los Angeles (Cty) Long Beach Miami (Miami-Dade Cty) Minneapolis New York City Oakland (Alameda Cty) Philadelphia Phoenix (Maricopa Cty) Portland (Multnomah Cty) San Antonio San Diego (Cty) San Francisco San Jose (Santa Clara Cty) Seattle (Seattle-King Cty) Washington, D.C. About 55 million or 1 in 6 Americans covered by BCHC-member LHDs
About CSTE About CSTE Formed in 1951 to define and recommend nationally notifiable diseases and conditions for CDC Membership association and community of practice on issues of surveillance and informatics o Over 2000 members
Background Background Epi Capacity Assessment Epi Capacity Assessment CSTE has conducted ECAs in 2001, 2004, 2006, 2009, 2013, & 2017 ECA Objectives o Enumerate the epidemiology workforce at State and Territorial health departments o Describe epi capacity by subject area and Essential Public Health Services (EPHS) o Describe the funding supporting the epi workforce o Identify areas of concern among epi leadership
Why State & Local? Prior limitation is focus on state HDs, not capturing numeric and functional capacity of locals Partnered with BCHC to assess the local epidemiology capacity in large urban health departments CSTE and BCHC solicited input from local epis to tailor the ECA to locals
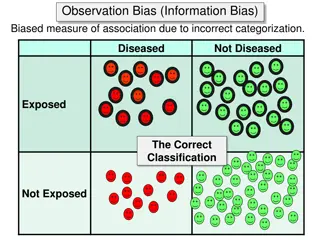
Definitions Definitions Capacity: The ability to lead activities, provide subject matter expertise, and apply for, receive, and manage resources to conduct key activities Epidemiologist: o All those employed by the state; all those working at the state level who are either federal assignees (e.g. EISO, CEFO, PHAP) or contract employees (e.g. CSTE trainee, contracted from school of public health to work at or for the State Health Department); and state employees assigned to work at a local or regional level (e.g. to conduct investigations for a region of the state). o An investigator who studies the occurrence of disease or other health related conditions or events in defined populations. The control of disease in populations is often also considered to be a task for the epidemiologist.
Essential Public Health Services Defined Essential Public Health Services Defined CSTE measured capacity in four primary Essential Public Health Services (EPHS) most relevant to epidemiology: o EPHS #1 Monitoring health status o EPHS #2 Investigating community health problems and hazards o EPHS #9 Evaluating the effectiveness of public health interventions o EPHS #10 Conducting research
Response Rate Response Rate BCHC: 27/30 (90%) member city/county health departments States: All (100%) 50 states and the District of Columbia responded along with 3 out of /6 Territories
BCHC Results BCHC Results
Structure and General Organization Structure and General Organization 48% indicated the epi workforce decentralized 37% indicated centralized w/in one division or office 15% reported the epi workforce is a hybrid structure 82% indicated the presence of on or more lead epis 78% indicated they have generalists supporting multiple program areas
BCHCs with Specific Program Areas & Formal Lead Epis in These Areas 100% Infectious disease 85% 100% MCH 74% 100% Preparedness 41% 93% Chronic disease 48% 92% Vital statistics 67% 85% Environmental health 41% 67% Injury 48% 63% Informatics 37% 60% Substance abuse 33% 56% Oral health 15% 33% Mental health 15% 19% Occupational health 4% 0% Genomics 0% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Program Lead
Number of Epidemiologists by Program Area Infectious disease 474 201 Environmental health 90 46 Vital statistics 40 40 Substance abuse 40 38 MCH 35 34 Preparedness 31 16 Oral health 5 1 Genomics 0 0 100 200 300 400 500 Number of Epidemiologists
Unmet Staffing Needs Unmet Staffing Needs
Essential Public Health Services Capacities 100% 93% 90% 78% 80% 70% 60% 50% 41% 37% 40% 33% 33% 30% 30% 26% 20% 15% 7% 10% 4% 4% 0% Monitoring health status Diagnosing/investigating problems Evaluation Research Minimal to none Partial Substantial to full
Current Capacity & Perceived Need for Improvement Essential Public Health Services 100% Infectious disease 89% 93% MCH 81% 89% Chronic disease 93% 89% Injury 88% 81% Preparedness 74% 78% Vital statistics 74% 78% Environmental health 89% 74% Substance abuse 85% 56% Informatics 85% 48% Mental health 89% 37% Oral health 67% 15% Occupational health 56% 0% Genomics 73% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Current capacity Need for improvement
BCHC Salary Ranges by Degree and Title BCHC Salary Ranges by Degree and Title
State Results State Results
Staffing levels are Inadequate Staffing levels are Inadequate [There is a] lack of funding and state positions to expand capacity in areas with existing epidemiologic activities and to create capacity in areas without current epidemiologic activities. [A challenge is] balancing resources to meet emerging issues, basic responsibilities and cooperative agreement deliverables We are challenged with continued increasing reporting and work requirements in most program areas despite level or decreasing federal funding.
Epis Epis Enumerated Range, number epidemiologists/ state 5-208 Number of states 51 Number of epidemiologists 3370 Median number/state 59 Rate/ 100,000 1.0 Median rate/100,000^ N/A Category United States State size* Small# Medium Large 15 17 19 406 997 1967 8-102 5-118 29-208 23 55 93 2.4 1.5 0.8 2.3 1.4 0.9 Geographic area Northeast Midwest South West *Small: < 2 million, medium: 2-6 million; large: >6 million; see Figure 1 for map. Population figures from 2016 US Census estimates 9 711 684 1209 766 19-208 9-142 13-136 5-195 58 61 71 59 1.3 1.0 1.0 1.0 1.8 1.2 1.2 1.5 12 17 13 Based on sum of all epidemiologists within a category and total population in that category ^Median of state-specific rates/100,000 #Kruksal-Wallis for difference between median rate/100,000 = 0.002
Ideal Number of Epis Ideal Number of Epis Ideal (current + additional) 2177 443 441 344 187 173 159 153 122 Need currently met (%)* 84% 72% 69% 65% 51% 64% 64% 77% 48% 43% 9% 42% 18% 76% 74% Increase needed to reach ideal (%) 18% 38% 45% 55% 95% 56% 56% 30% 109% 134% 1058% 139% 459% 31% 36% Program area Infectious disease MCH Chronic disease Environmental health Informatics Vital statistics Injury Preparedness Substance abuse Occupational health Mental health Oral health Genomics Other TOTAL Current 1838 321 304 222 96 111 103 118 59 28 Additional 338 122 137 122 91 62 57 36 64 38 42 25 20 45 67 46 43 25 189 4569 4 18 4 143 3370 1199 *current/ideal *100 (ideal-current)/current *100
Trends in Epis Trends in Epis Trends in number of epidemiologists by program area, 2004-2017, 50 States and DC and variable number of territories in 2004 and 2006, ECA 2000 1800 1600 1400 1200 1000 800 600 400 200 0 ID BT/Prep Chronic Env MCH Injury Occup Oral 2004 2006 2010 2013 2017
Specific skillsets are needed Specific skillsets are needed One of my main concerns is having a workforce prepared to function in the new world of public health epidemiology. We are facing big changes right now in how we receive information, the volume of data/information, emerging programs related to [hospital acquired infections] with large expectations [and] rapid changes in lab testing . that affect the information we receive and the need to adapt all our investigation protocols accordingly. It is challenging to keep the workforce well prepared in the face of so much change at such a rapid pace. Transitioning from a number of one-off data systems to a more efficient interoperable system with enterprise-wide approaches to data collection, data parsing, data provisioning, data preparing, data analysis and data visualization requires additional training in informatics and data analytics. There is a need for epidemiologists to be able to think critically about the diseases and risk factors under surveillance and to be able to look beyond the mechanics of just data analysis.
EPHS Capacity EPHS Capacity EPHS capacities, 50 states and DC, ECA, 2017* 100% 92% 90% 84% 80% 70% 60% 50% 41% 39% 39% 39% 40% 30% 22% 20% 16% 20% 8% 10% 0% 0% 0% Monitoring health status Diagnosing/investigating Evaluation Research problems Minimal to none Partial Substantial to full
EPHS Capacity by Program Area EPHS Capacity by Program Area EPHS capacity by Program Area, 50 states and DC, ECA, 2017* Genomics Mental health Occupational health Informatics Oral health Substance abuse Vital statistics Injury Preparedness Environmental health Chronic disease MCH Infectious disease 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% None to minimal Partial Substantial to full
Need to Improve EPHS Need to Improve EPHS Perceived need to improve EPHS capacity by program area, 50 states and DC, ECA, 2017* Mental health (32) 94% Substance abuse (48) 93% Informatics (47) 93% Injury (51) 90% Chronic disease (51) 88% Environmental health (49) 88% Occupational health (36) 85% MCH (51) 84% Infectious disease (51) 80% Genomics (26) 80% Oral health (48) 74% Vital statistics (48) 73% Preparedness (50) 64% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
Priority to Improve EPHS Priority to Improve EPHS Priority to improve EPHS capacity by program area, 50 states and DC, ECA, 2017* High priority Medium priority Low or not a priority Substance abuse (48) Informatics (47) Infectious disease (51) Mental health (32) Chronic disease (51) MCH (51) Environmental health (49) Injury (51) Preparedness (50) Vital statistics (48) Genomics (26) Oral health (48) Occupational health (36) 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%
Training Priorities Training Priorities Top training needs identified by State Epidemiologists, 50 states and DC, ECA, 2017* Data analytics 38 Systems thinking 12 Persuasive communication 12 Leadership development 12 Continuing education 11 Software skills 9 Assessments and evaluations 5 Fiscal management 2 Team-building 1 Cultural competency 0 0 5 10 15 20 25 30 35 40 Number of times cited
Uncertain funding affects staffing Uncertain funding affects staffing We have shrinking resources as our department becomes larger, yet we are expected to fill roles that we are not funded for. Increased attention and funding to specific program areas [is] followed by loss of attention and funding, but these threats have not resulted in acknowledgment of the need to maintain a basic level of readiness for all existing and emerging threats. The high level of dependency on federal funding sources limits the flexibility of the state to respond to emerging public health threats and increases vulnerability of the workforce to reductions in federal appropriations.
Funding Trends (Activities) Funding Trends (Activities) Trends in sources of funding for epidemiology activities, 2001-2017, 50 states and DC and variable number of territories in 2004 and 2006, ECA 90% 79% 77% 75% 80% 73% 70% 61% 60% 50% 37% 40% 27% 30% 23% 19% 19% 20% 10% 4% 2% 2% 2% 0% 0% Federal State Other 2001 2004 2009 2013 2017
Funding by Positions Funding by Positions Source of funding by program area, 50 states and DC, ECA, 2017* Preparedness (118) Occupational health (28) Substance abuse (59) Infectious disease (1838) MCH (321) Injury (103) Chronic Disease (304) Informatics (96) Environmental health (222) Vital statistics (111) Other (143) 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% CDC-supported CDC direct Other federal State Other sources
BCHC Vs States: Epis/100,000 people BCHC Vs States: Epis/100,000 people BCHC Median: 1.4 epis per 100,000 people Range of 0.4 to 7.5 State Median: 1.0 epis per 100,000 people
BCHC Vs States: Funding BCHC Vs States: Funding 47% of BCHC epi activities are from local sources State: 24% Federal: 27% More than three-quarters of state epi activities are from federal sources State: 20%
BCHC vs. States: Top Training Needs BCHC vs. States: Top Training Needs States 1. Data Analytics (38%) 2. Systems Thinking (12%) 3. Persuasive Communication (12%) 4. Leadership Development (12%) BCHC 1. Data Analytics (48%) 2. Systems Thinking (33%) 3. Persuasive Communication (26%)
BCHC vs. States: Current Program Capacity, Perceived BCHC vs. States: Current Program Capacity, Perceived Need to Improve Capacity, Priority to Improve Capacity Need to Improve Capacity, Priority to Improve Capacity States Substantial to Full Current Program Capacity ID 96%, CD 78%, MCH 73%, Prep 57% Need to Improve Capacity MH 94%, SA 93%, Infx 93%, Injury 90% High/Medium Priority to Improve Capacity SA 94%, Infx 79%, MH 78%, CD 78%, ID 74% BCHC Adequate Current Program Capacity ID 100%, MCH 93%, CD 89%, Injury 89% Need to Improve Capacity CD 93%, ID 89%, EH 89%, MH 89%, Injury 88% High/Medium Priority to Improve Capacity CD 74%, SA 74%, ID 67%, Infx 67%
So What Did We Learn? So What Did We Learn? Lack of predictable, sustainable funding hinders capacity building Role of epis not well understood Have epis for 20th century, not necessarily 21st century, PH challenges Technology/new tech remains a challenge
Q/A & Audience Discussion Q/A & Audience Discussion
Contact Information Contact Information Chrissie Juliano (cjuliano@naccho.org) Meghan McGinty (mmcginty@naccho.org) Big Cities Health Coalition www.bigcitieshealth.org Jessica Arrazola (jarrazola@cste.org) Council of State and Territorial Epidemiologists https://www.cste.org/ @BigCitiesHealth https://www.facebook.com/BigCitiesHealth @CSTEnews https://www.facebook.com/CSTE.org/ http://www.bigcitieshealth.org/front-lines-blog/
Additional Sessions Wednesday July 11, 2018 11:30 AM 12:00 PM | Big Cities Health Inventory: Local Data for Action (A) 1:30 PM 2:00 PM | Big Cities Health Inventory: Local Data for Action (B) 2:15 PM 3:45 PM | The First Nat l Data on the LHD Workforce: PH WINS 2017 2:15 PM 3:45 PM | More Bang for Your Buck: Learning Collaborative Partnerships Focused on Using Cost-Effectiveness Analysis in Decision Making