Understanding Pulmonary Emphysema: Symptoms, Causes, and Pathophysiology
Pulmonary emphysema, a type of obstructive respiratory disorder, is a progressive lung disease that affects the air spaces in the lungs. This condition is primarily caused by long-term exposure to irritants like tobacco smoke and air pollution. The damage to the alveoli leads to symptoms such as shortness of breath. Pathophysiologically, emphysema involves the destruction of airspaces, reducing the gas exchange capacity of the lungs. Different subtypes exist based on the extent of acinar involvement, with smoking and genetic factors playing key roles in its development.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
GROUP 1 PRESENTATION OBSTRUCTIVE RESPIRATORY DISORDER
OBSTRUCTIVE RESPIRATORY DISORDER Obstructive respiratory disorder is a category of respiratory disease characterized by airway obstruction. This means that the airways in the lungs are narrowed, making it difficult to breathe in and out.
0BSTRUCTIVE RESPIRATORY DISORDER INCLUDES: Pulmonary Emphysema Chronic Bronchitis Bronchiectasis Cystic Fibrosis Bronchiolitis Asthma Primary Ciliary Dyskinesia
PULMONARY EMPHYSEMA
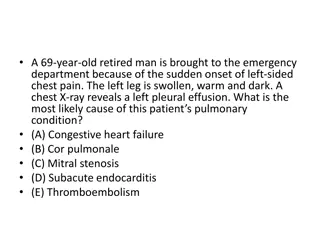
Pulmonary Emphysema Pulmonary emphysema, a progressive lung disease, is a form of chronic obstructive pulmonary disease (COPD). Emphysema is primarily a pathological diagnosis that affects the air spaces distal to the terminal bronchiole. In people with emphysema, the air sacs in the lungs (alveoli) are damaged. Over time, the inner walls of the air sacs weaken and rupture creating larger air spaces instead of many small ones. This reduces the surface area of the lungs and, in turn, the amount of oxygen that reaches your bloodstream.
Pathophysiology The clinical manifestations of emphysema are the consequences of damage to airways distal to terminal bronchiole, which include respiratory bronchiole, alveolar sacs, alveolar ducts, and alveoli, collectively known as the acinus. There is abnormal permanent dilatation of the airspaces and destruction of their walls due to the action of the proteinases. This results in a decrease in the alveolar and capillary surface area, which decreases the gas exchange. The part of the acinus affected determines the subtype. It can be subdivided pathologically into the following: Centrilobular (proximal acinar) is the most common type and is commonly associated with smoking. It can also be seen in coal workers' pneumoconiosis. Panacinar is most commonly seen with alpha one antitrypsin deficiency. Paraseptal (distal acinar) may occur alone or in association with the above two. When it occurs alone, the usual association is a spontaneous pneumothorax in a young adult.
Symptoms You can have emphysema for many years without noticing any signs or symptoms. The main symptom of emphysema is shortness of breath. Causes The main cause of emphysema is long-term exposure to airborne irritants, including: Tobacco smoke Marijuana smoke Air pollution Chemical fumes and dust Rarely, emphysema is caused by an inherited deficiency of a protein that protects the elastic structures in the lungs. It's called alpha-1-antitrypsin deficiency emphysema.
Risk factors: Factors that increase your risk of developing emphysema include: Smoking. Emphysema is most likely to develop in cigarette smokers, but cigar and pipe smokers also are susceptible. The risk for all types of smokers increases with the number of years and amount of tobacco smoked.
Risk factors contd Age. Exposure to secondhand smoke. Occupational exposure to fumes or dust. Exposure to indoor and outdoor pollution. Complications People who have emphysema are also more likely to develop: Collapsed lung (pneumothorax). A collapsed lung can be life-threatening in people who have severe emphysema, because the function of their lungs is already so compromised. This is uncommon but serious when it occurs.
Complications contd Heart problems. Emphysema can increase the pressure in the arteries that connect the heart and lungs. Large holes in the lungs (bullae). Some people with emphysema develop empty spaces in the lungs called bullae. They can be as large as half the lung. In addition to reducing the amount of space available for the lung to expand, giant bullae can increase your risk of pneumothorax.
Chronic Bronchitis Bronchitis is inflammation of the breathing tubes called bronchi. This inflammation causes too much mucus production and other changes. There are different types of bronchitis. But the most common are acute and chronic. Chronic bronchitis is long-term inflammation of the bronchi characterized by a chronic cough and sputum production lasting for at least 3 months in a year for 2 consecutive years. People with chronic bronchitis tend to get lung infections more easily. They also have episodes of acute bronchitis, when symptoms are worse, and it is often secondary to COPD
Chronic Bronchitis contd It is important to note that Chronic bronchitis and Emphysema have similar characteristics but CB is a lung condition that destroys tiny hairs, called cilia, in the airways of the lungs leads to excessive mucus build-up in the bronchi while Emphysema occurs when the alveolar membrane breaks down .
Etiology There are many known causes of chronic bronchitis, but the most important causative factor is exposure to cigarette smoke, either due to active smoking or passive inhalation(Environment). Many inhaled irritants to the respiratory tract, such as smog, industrial pollutants, and toxic chemicals, can cause chronic bronchitis. Although bacterial and viral infections usually cause acute bronchitis, repeated exposure to infections can cause chronic bronchitis.
Pathophysiology Chronic bronchitis is caused by overproduction and hypersecretion of mucus by goblet cells. Epithelial cells lining the airway respond to toxic, infectious stimuli by releasing inflammatory mediators .There is also an associated decrease in the release of regulatory substances such as angiotensin-converting enzyme and neutral endopeptidase. During an actue phase of chronic bronchitis, the bronchial mucous membrane becomes hyperemic and inflamed with diminished bronchial mucociliary function.
Symptoms Cough, often called smoker s cough Coughing up mucus Chest discomfort Shortness of breath due to cough Frequent and severe infections that affect your airways Narrowing and plugging of your breathing tubes (bronchi) Peripheral cyanosis- Bluish fingernails, lips, and skin because of lower oxygen levels Wheezing and crackling sounds with breathing
Diagnosis Given thatbboth em[physma and chronic bronchitis are subtypes of COPD,it is crucial to receive a precise diagnosis to avoid mishandling one s course of therapy. The investigations which assist in confirming the diagnosis of chronic bronchitis are: 1-Blood test: This is to see if your symptoms could be due to anemia, or to see if the symptoms are due to the genetic marker alpha-1-antitrypsin deficiency( this rules out Emphysema) 2 - Chest x-ray 3- A culture of the sputum when a bacterial infection is suspected.
BRONCHIECTASIS Bronchiectasis is the persistent irreversible pathological dilation (and out pouching) of the bronchi and bronchioles secondary to destruction of airway cartilage and elastic tissue it s caused by recurrent airway infection and inflammation the segment bronchi fill up with mucus and pus(purulent sputum) and then becomes fibrotic ; could be focal or diffuse could be tubular, cylindrical, varicose or cystic could be caused by infection and non infectious causes it could be primary (the lung was normal) or secondary ( lung had a problem before the bronchiectasis)
Etiology Cystic fibrosis Infection : TB, severe pneumonia (viral or bacterial) Immotile cilliary syndrome leading to mucus stagnation Allergic bronchial pulmonary aspergillosis Focal bronchial obstruction Toxin inhalation
Pathophysiology Normal protective mechanism of the lung is altered ( the epithelial cells, goblets cell, mucocilliary apparatus, Antimicrobial peptide, cough mechanism) leading to permanent airway dilation and stagnation of sputum in the airway resulting in infection, which trigger inflammation, and this becomes a vicious cycle between infection and inflammation. There are 2 phases, which are: Initial insult to the airway epithelium: causes initial bronchodilation and the mucocilliary impairment, which predispose one to infection and inflammation the second phase is the ongoing inflammation cycle and further infection leading to permanent airway remodeling
Clinical Features Productive cough with cupful sputum that s thick, purulent and foul smelling Hemoptysis Sign: nail clubbing Diagnosis History taking Radiological findings The gold standard for diagnosis bronchiectasis is high resolution CT scan
CYSTIC FIBROSIS Definition: Cystic fibrosis (CF) is an inherited life- threatening disorder that damages the lungs and digestive system. CF is chronic and progressive Most common in white people than blacks CF affects the cells that produce mucus, sweat and digestive juices.
ETIOLOGY AND PATHOPHYSIOLOGY It is caused by a mutation in gene (CFTR) CFTR- Cystic Fibrosis Transmembrane Conductance Regulator It contains CFTR protein that function normally as a chloride channel, allowing chloride ions passage across cell membrane Mutations in CFTR gene = THICK and STICKY mucus in the respiratory, digestive and reproductive systems(urogenital organs) as well as increased salt in sweat They obstruct passageways making breathing difficult Thick mucus cannot be readily cleared and becomes an environment for bacteria to grow and cause infections CF is inherited in an autosomal recessive manner
SYMPTOMS It could be typical or atypical. The later the symptoms manifest, the milder the disease. They include: Persistent cough Wheezing Repeated or frequent lung infections (recurrent pneumonia or bronchitis) Difficulty in breathing
RISK FACTOR Family history DIAGNOSIS Genetic tests Sweat tests Chest X-rays Lung function tests Sputum culture
BRONCHIOLITIS Bronchiolitis is a viral lower respiratory tract infection, leading to small airway inflammation and edema. Bronchiolitis is a common respiratory infection that primarily affects infants and young children under the age of 2 it is rare in adults . The most common cause of bronchiolitis is a viral infection, which is respiratory syncytial virus (RSV) being the leading culprit. However, other viruses can also cause bronchiolitis, Including: Rhinovirus, Influenza virus, Human metapneumovirus, Coronavirus
Symptoms Rapid breathing Wheezing Cough Runny nose Fever Decreased appetite Fatigue
PATHOPHYSIOLOGY Virus infection: The virus that causes bronchiolitis can directly damage the cells lining the bronchioles. This damage can lead to inflammation, swelling, and mucus production. Cytokines: The virus can also release cytokines, which are chemicals that cause inflammation. These cytokines can further damage the bronchiolar cells and lead to airway obstruction. Immune response: The body's immune system responds to the virus infection by sending white blood cells to the airways. These white blood cells can also damage the bronchiolar cells and contribute to airway obstruction. Airway hyperreactivity: In some children, bronchiolitis can lead to airway hyperreactivity, which is a narrowing of the airways that can occur in response to triggers such as cold air, smoke, or exercise. This airway hyperreactivity can make it more difficult for children to breathe and can lead to wheezing.
Mechanism of action Inflammation Mucus production Cilia dysfunction Bronchoconstriction
Risk Factors Age:it is mostly common in children below 2years old Prematurity: Infants who are born prematurely are at an increased risk of developing bronchiolitis. This is because their lungs are not fully developed and they may have a weaker immune system. Low birth weight: Infants who are born with low birth weight (less than 5 pounds, 5 ounces) are also at an increased risk of developing bronchiolitis. Congenital heart disease: This is because their hearts may not be able to pump blood effectively, which can lead to fluid buildup in the lungs. Chronic lung disease: Children with chronic lung diseases,are at an increased risk of developing bronchiolitis. This is because their lungs are already damaged and they may have a harder time fighting off infection.
ASTHMA Asthma is a disease that affects your lungs. It causes repeated episodes of wheezing, breathlessness, chest tightness, and nighttime or early morning coughing. Asthma can be controlled by taking medicine and avoiding the triggers that can cause an attack. You must also remove the triggers in your environment that can make your asthma worse.
Common asthma attack triggers include: Air pollution Dust molds Exercise Molds Pests Tobacco smoke Strong chemical or smells Certain occupational exposures Strong emotional state/ stress.
Pathophysiology Asthma is a condition of acute, fully reversible airway inflammation, often following exposure to an environmental trigger. The pathological process begins with the inhalation of an irritant (e.g., cold air) or an allergen (e.g., pollen), which then, due to bronchial hypersensitivity, leads to airway inflammation and an increase in mucus production. This leads to a significant increase in airway resistance, which is most pronounced on expiration. Airway obstruction occurs due to the combination of: Inflammatory cell infiltration. Mucus hypersecretion with mucus plug formation. Smooth muscle contraction. These irreversible changes may become irreversible over time due to: Basement membrane thickening, collagen deposition, and epithelial desquamation.
Risk Factors Genetics Atophy Obesity Prenatal risk factors for asthma may include maternal smoking, diet and nutrition, stress, use of antibiotics and delivery by cesarean section. Childhood risk factors for asthma may include allergic sensitization, environmental tobacco smoke, exposure to animals, breastfeeding, decreased lung function in infancy, family size and structure, socio-economic status, antibiotics and infections, and sex and gender. Adult onset asthma: Occupational exposures constitute a common risk factor.Another risk factor is smoking tobacco/marijuana.
Diagnosis of Asthma Asthma can usually be diagnosed from your symptoms and some simple tests.A GP will probably be able to diagnose it, but they may refer you to a specialist if they're not sure. Seeing a GP The GP may ask: What symptoms you have When they happen and how often
Diagnosis of Asthma Contd If anything seems to trigger them If you have conditions such as eczema or allergies, or a family history of them They may suggest doing some tests to confirm if you have asthma. These cannot always be done easily in young children, so your child may be given an asthma inhaler to see if it helps relieve their symptoms until they're old enough to have the tests.
Tests For Asthma The main tests used to help diagnose asthma are: FeNO test Spirometry Peak flow test After you're diagnosed with asthma, you may also have a chest X-ray or allergy tests to see if your symptoms might be triggered by an allergy.
PRIMARY CILIARY DYSKINESIA (PCD)
Primary Ciliary Dyskinesia (PCD) Primary ciliary dyskinesia (PCD) : is a rare respiratory disease that occurs in neonates and is as a result of genetically heterogeneous recessive disorder of the cilia structure .
Pathogenesis Mutations in the dynein arm of the cilia ends in PCD. In the respiratory tract, cilia moves back and forth in a coordinated manner to clear mucus. This movement of mucus helps to eliminate fluid, bacteria, and particles from the lungs. Most babies with primary ciliary dyskinesia experience breathing problems at birth, suggesting that the cilia play an important role in clearing fetal fluid from the lungs. Affected individuals develop recurrent respiratory tract infections. patients with PCD may demonstrate mild fetal ventriculomegaly on prenatal ultrasound scans.
Risk Factors Genetics Symptoms of PCD 1. Chronic wet cough producing sputum, from infancy, that lasts for four weeks or longer. 2. Recurring pneumonia or chest colds 3. About half of all people who have PCD have bronchiestsis
Diagnosis The use of Electron microscopy Physical examination CT scan of the lungs and para nasal sinuses Prognosis Prognosis is generally based on early diagnosis and prompt treatment.
REFERENCES Primary ciliary dyskinesia ; genetic and rare disease information center (wickidoc.org) https://rarediseases.info.nih.gov/diseases/4484/primary-ciliary-dyskinesia Chronic Bronchitis - https://www.physio-pedia.com/Chronic_Bronchitis. Chronic Bronchitis (2019). Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-bronchitis. Widysanto, A. (2022) Chronic Bronchitis. https://www.ncbi.nlm.nih.gov/books/NBK482437/ Asthma: epidemiology, etiology and risk Factors https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2764772/ Risk factors for asthma https://www.webmd.com/asthma/asthma-risk-factors Asthma causes and risk factors https://www.google.com/amp/s/www.credihealth.com/blog/asthma-causes-and-risk- factors/amp/#ip=1 What Is Asthma? Symptoms, Causes, Diagnosis, Treatment, and Prevention https://www.everydayhealth.com/asthma/guide/ Asthma https://www.statpearls.com/ArticleLibrary/viewarticle/17920 Wagner T. Bronchiolitis.Pediatr Rev.2009 Oct;30(10) Bradley JP, Bacharier LB, Bonfiglio J, Schechtman KB, Strunk R, Storch G, Castro M. Severity of respiratory syncytial virus bronchiolitis is affected by cigarette smoke exposure and atopy.Pediatrics.2005 Jan Silver AH, Nazif JM. Bronchiolitis.Pediatr Rev.2019 Nov; Castro M, Schweiger T, Yin-DeClue H, Ramkumar TP, Christie C, Zheng J, Cohen R, Schechtman KB, Strunk R, Bacharier LB. Cytokine response after severe respiratory syncytial virus bronchiolitis in early life. J Allergy Clin Immunol.2008 Oct;