Strategic Insights for Managed Care in Healthcare
Explore strategic considerations for managed care in the healthcare sector, including market analysis, contract renegotiation, and practice positioning. Learn about key factors influencing managed care strategy and effective approaches for navigating payer relationships and operational challenges.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
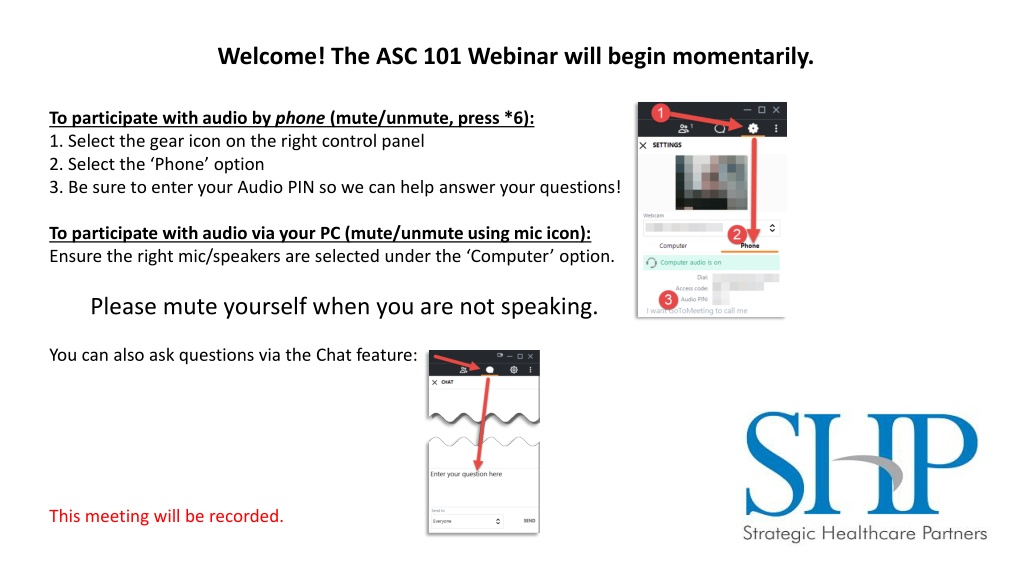
Welcome! The ASC 101 Webinar will begin momentarily. To participate with audio by phone (mute/unmute, press *6): 1. Select the gear icon on the right control panel 2. Select the Phone option 3. Be sure to enter your Audio PIN so we can help answer your questions! To participate with audio via your PC (mute/unmute using mic icon): Ensure the right mic/speakers are selected under the Computer option. Please mute yourself when you are not speaking. You can also ask questions via the Chat feature: This meeting will be recorded.
ASC 101: Managed Care Strategy in the Age of the No Surprises Act shpllc.com | 912-691-5711
ASC Historical Approach to Managed Care Stay out if possible, out of net reimbursement tended to be pretty lucrative. If forced to contract, go for highest rates; use carveouts if necessary. Ensure ASC can see all patients. Ensure all individual procedures are profitable. shpllc.com | 912-691-5711
The Difference Between A Managed Care Strategy and Go Renegotiate My Anthem Agreement Managed care strategy is based on understanding several factors: Practice position in the market. Portion of specialty provided locally. Overall cost effectiveness to a provider; at least Medicare cost scoring. Overall payer landscape and that particular payer s position in the market (both today and in the future). Payer Performance Admin burdens under which the payer forces the provider to operate. Full case denial rates, line item denial rates, underpayment rates, claim turn/days in AR. Changing legal/regulatory landscape (ala No Surprises; CON; DOI/DCH support). shpllc.com | 912-691-5711
Managed Care Strategy vs. Renegotiating Contracts Market Analysis Who are the major payors? Governmental vs. commercial participation Financial Proformas In-network vs. out-of-network reimbursement Understanding your case costs (direct vs indirect) Operational Issues Are there administrative burdens that the ASC needs to solve to see patients? Inability to obtain authorizations Redirection of care concerns shpllc.com | 912-691-5711
Practice Positioning in the Market What portion of the market for our specialty does our practice represent? If we don t participate (MD side), do we create a real problem for a carrier? Are we growing? Growing significantly? MD and ASC sides? Can we support that we are cost effective? (Medicare data or otherwise) Does the practice or ASC have capacity issues leading to long appointment lead times or other possible customer service issues a payer might know about? Are our payer relationships good? Do they see us as market critical? shpllc.com | 912-691-5711
The Payer Landscape: The Payer Landscape: What Market Forces are Changing All This? What Market Forces are Changing All This? shpllc.com | 912-691-5711
Shifting Payer Market in Georgia Payer Mix in Georgia has been relatively stable for the last five years but that is rapidly changing thanks to expansion & growth of governmental carriers Commercial Plan growth really limited to the Big Five .Aetna, Anthem, Cigna, Humana & United Exchange plan growth has disrupted this established hierarchy: With the bolstered exchange plan subsidies, enrollment in the Exchange remains off the charts. From 2021 to 2022, Georgia enrollment jumped from 514,000 to 653,990. In 2022, five new payers entered the Georgia market. Has launched significant shift in payer diversification from the market consolidation we saw five years ago. To most practices outside of Atlanta, Ambetter (Exchange) is now bigger than Aetna and Humana at least. shpllc.com | 912-691-5711
Payer Mix - Medicare Advantage Biggest shift in payer market continues to be traditional Medicare to Medicare Advantage plans. From 2019 to 2022, traditional Medicare has decreased from around 25% of total patient population to less than 20%. Biggest beneficiary of that growth in the market has been Humana. This trend is certain to continue; current projections anticipate that nationally, Medicare Advantage will account for over half of all Medicare enrollments by CY 2030. https://www.kff.org/medicare/issue-brief/medicare-advantage-in-2021-enrollment- update-and-key-trends/ Has caused carrier feeding frenzy due to automatic ability to compete with Anthem for provider pricing, thus, mechanism for payer diversification in market. shpllc.com | 912-691-5711
Payer Mix - Medicaid/CMO Developments Medicaid CMO RFP Medicaid Managed Care will come back up for bid in late 2022 with planned contract implementation of 7/1/2024. New carriers interested in Georgia: Humana Molina Aetna UHC Critical Letter of Intent (LOI) Process during rebid- to be released early 2023. Rumors: Full expansion still off the table. Traditional Medicaid population moving to CMOs on the table. Adding a 4th CMO definitely on the table. shpllc.com | 912-691-5711
Payer Mix- State Health Benefit Plan Developments SHBP has been extended with same carriers through at least 12/31/24. 9th year of 5 year agreement. Market share within SHBP continues to be: Anthem- 99% market share for active enrollees. UHC- 99% market share for retirees. When bid finally comes, we suspect that the following will pursue: Aetna Kaiser Humana shpllc.com | 912-691-5711
Understanding What the Carriers Want To move to standardized facility payment methodology (COPPS) Protect/Grow Commercial Market Share Big push towards more competitive/equalized rates to allow carrier competition Protect market share/repel market diversification in Exchange/Medicare Advantage space. Medicaid is a huge target for traditional commercial carriers. SHBP when it finally comes back to market. shpllc.com | 912-691-5711
Payer Performance: Payer Performance: From Pain in the Rear to Real Hits From Pain in the Rear to Real Hits shpllc.com | 912-691-5711
Restrictive Payer Policies Redirection of care Outsourcing services to third-party vendors Network panel closures Practice/ASC Issues: Restrictive in house lab lists. Lab bundling in ASC setting. Slow pre-auth/excessive/small $ pre-auth. shpllc.com | 912-691-5711
New ASC Reimbursement Methodologies Starting to see some drift away from traditional grouper methodology/ limitation on carveouts. More Commercial plan attempts to tie-ins to Medicare methodology; particularly for the Exchange plan carriers. Anthem COPPS Methodology Anthem attempt to standardize facility reimbursement method to a Hospital Ambulatory Payment Category (APC) methodology. Over 50 groupings; no carveouts. Based on overall base rate similar to Medicare RBRVS. shpllc.com | 912-691-5711
Payer Performance Measurement Days in AR by carrier vs. overall. Initial claim reject rate. Overall % of expected allowable collection rate by payer. Claim zero pay rate by payer. Line item zero pay rate by payer. Soft measurements: % of payer volume requiring pre-auth. Payer pre-auth turnaround. shpllc.com | 912-691-5711
The Regulatory/Legal Landscape: The Regulatory/Legal Landscape: No Surprises and What Else? No Surprises and What Else? shpllc.com | 912-691-5711
No Surprises Act What is the No Surprises Act? The No Surprises Act protects people covered under group and individual health plans from receiving surprise medical bills when they receive most emergency services, non- emergency services from out-of-network providers at in-network facilities, and services from out-of-network air ambulance service providers. How does it Impact ASCs? For insured beneficiaries, nonparticipating provider cannot bill a patient for an amount that exceeds the cost sharing requirement for such item or service unless the provider or facility satisfies the notice and consent criteria. For self-pay/non-insured beneficiaries, ASC must provide a good faith estimate for all services and providers. When did it take effect? January 1, 2022 shpllc.com | 912-691-5711
Consent Timing Under the No Surprises Act If an individual makes an appointment for the relevant items or services at least 72 hours before the date that the items and services are to be furnished, these notice and consent documents must be provided to the individual, or the individual s authorized representative, at least 72 hours before the date that the items and services are to be furnished. If the individual makes an appointment for the relevant items or services within 72 hours of the date the items and services are to be furnished, these notice and consent documents must be provided to the individual, or the individual s authorized representative, on the day the appointment is scheduled. Where an individual is provided the notice and consent documents on the day the items or services are to be furnished, including for post-stabilization services, the documents must be provided no later than 3 hours prior to furnishing the relevant items or services. shpllc.com | 912-691-5711
Consent Requirements Under the No Surprises Act State that the healthcare provider is a nonparticipating provider. Include the good faith estimated amount the nonparticipating provider may charge the participant. Provide a statement that prior authorization may be required in advance of receiving such items or services. State the consent to receive such services from the nonparticipating provider is optional and they may seek to receive care from a participating provider. shpllc.com | 912-691-5711
No Surprises Act for Uninsured & Self Pay Patients ASCs must provide a good faith estimate to uninsured and self-pay patients. Estimates must include: All expected charges for items or services Items of services that may be provided by co-providers - other facilities/groups (i.e. anesthesia, etc.) Good faith estimate must use clear and understandable language and include an itemized list of each item or services, grouped by each provider offering care. ASC is usually considered the convening provider ; when they received the request for an estimate, they are responsible for collecting estimates from any co-providers. Estimate must be provided within one business day of scheduling or within three days of a request even if service is not scheduled. If a patient receives a good faith estimate and is billed for at least $400 higher than the estimate, he patient can begin an independent dispute resolution process to determine the payment amount. shpllc.com | 912-691-5711
How will Payers React to the No Surprises Act? Potential for more aggressive negotiation tactics For providers who render care in emergency settings, real concern that payers will begin terminating network participation to take advantage of established qualified payment amounts set by federal government. Incentive to contract for non-emergent services. Movement towards the lowest common denominator if they are using the Qualified Payment Amounts (QPAs) from Independent Dispute Resolutions process to set market rates. shpllc.com | 912-691-5711
What other Leverage Exists? Any Willing Provider Statute Push towards managed care adequacy regulations defined at a state level. Regulatory Agency Support Some support offered via: Department of Insurance Department of Community Health Who else??? CMS, Veterans Affairs, ERISA based plans don t really get involved in healthcare provider disputes. So what happens then? Best avenue is building relationships with your local, state and federal legislators to encourage them to take action when needed. shpllc.com | 912-691-5711
State Department of Insurance Official oversight of only fully insured commercial... No Health Exchange, Medicare Advantage, commercial self funded, Medicaid CMO, etc. However, tend to be only go to for all commercial issues, so try those anyway Anthem Market Conduct Review Largest fine in DOI history. Consent Order Potential for new Anthem Dispute Resolution Process with DOI oversight. New provider communication methods? DOI oversight over policy changes/unilateral contract issuances? So many issues submitted, DOI may initiate new market conduct review all over again. HB 888 (State Level Surprise Billing) - Out of Network portal open. Note: No one wants to get involved in negotiations/renegotiations so have to obtain support in other ways. shpllc.com | 912-691-5711
State Department of Community Health Oversight of traditional Medicaid, CMOs, and State Health Plan Leverage in regards to statewide network/network adequacy requirements. Key involvement drives from beneficiary impact: Patient harm Diminished/disrupted access to care Incorrect bills/patient liability based on payer inability to load contracts shpllc.com | 912-691-5711
Some Things Practices With ASCs Need to Know In spite of the obvious cost differential, the plans tend to not give a rip about the FFS savings and focus on lowest price to that provider in that setting. Carriers care more about specialist MD side participation than ASC participation. (They see you as 1 thing; you need to be a single package to them) If all procedures have to be profitable, without question, the final overall answer will be worse. Carriers are still very leery of ASC overutilization/self referral. At the end of the day, carriers still do not care about true patient quality. They only care about measurements of avoided future costs. shpllc.com | 912-691-5711
Emerging Market: ASC Bundles Platforms that bypass traditional mechanism of overall direction via general plan design to direct care for specific procedures to providers and facilities who agree to accept a single fee for all services covered. Typically involves surgical professional fee, pre-surgery labs, anesthesia, plus facility fee. Might further involve some pre-surgery prof fees and post surgical follow up. Versions: Large carrier based- Centers of Excellence or other directed mechanism which lowers/eliminates patient liability for pre-set contracted pricing. Generally some quality measurements as well. TPA or Bundling Admin based- Similar mechanically, however, provider defines bundles and pricing. shpllc.com | 912-691-5711
Value Based Initiatives CMS started the trend with their bundle programs Slowly transitioning over to Medicare Advantage & Commercial Payers Anthem Episode Based Payment Humana Site of Service Humana Total Joint Replacement Bundles Partnering with primary care providers as their base for specialist referrals to manage and access shared savings shpllc.com | 912-691-5711
Value Based Initiatives To learn more about how you can develop a value-based strategy, join us for ASC 201: Value Based Care on April 28 Value-Based Care has finally come for the specialists the first specialist based value models have arrived, primarily addressing bundled payments or site of care redirections. But beyond that, your primary care referral base are taking on more risk in managing the full direction and scope of care. Their value models have matured and they are accessing data and quality results on your services; including unit reimbursement, cost, volume, case mix scenarios, quality results, and overall margin targets for your payer strategy. So how do independent specialists and ASCs develop relationships as the preferred downstream provider in a value-based shared savings model? Join us to learn more about this and how you drive increased volume by becoming the preferred value based partners for your primary care community. Registration: https://teams.microsoft.com/registration/-nFbmCRclE-sko03BDvX- w,uRXPGd7QhkCkty52L2BMaQ,U_Y-RnC6OEGAzALeWP2qgA,mUR0- bNFqUKV71vSWgnkRA,rUV3GuG0JE2WqsazksOn4Q,aDPSHFmNl0SJ8Kx0C7Hzsw?mo de=read&tenantId=985b71fa-5c24-4f94-ac92-8d37043bd7fb shpllc.com | 912-691-5711
Wrap Up & Questions Unmute using *6 or the mic icon in the app or use the chat to ask. shpllc.com | 912-691-5711