Understanding Medications and Pharmacological Therapy for Urinary Incontinence
This learning module for clinicians discusses the physiology of bladder control, age-related changes in the genitourinary system, medications that contribute to urinary incontinence, pharmacological treatments for UI, side effects of medications used for UI, and a senior-friendly approach to optimizing medications for older individuals with UI.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Urinary Incontinence - culprit medications and pharmacological therapy A learning module for clinicians Jillian Alston, MD, FRCPC
This module is part of the sfCare approach This module follows the Urinary Incontinence introductory module for clinicians Patient Handout 8.5 x 11 Poster PowerPoint Presentation 2
Objectives 1. Summarize the physiology of bladder control Objectives 2. Describe age-related changes to the genitourinary system Physiology of bladder control 3. Apply knowledge of bladder physiology in order to: Age-related changes Classify and identify medications that contribute to urinary incontinence (UI) and urinary symptoms Medications causing incontinence Classify and identify pharmacological treatments used for UI Medications to treat incontinence 4. Identify the side effect profile of medications used to treat UI Case study Summary 5. Apply a senior friendly approach to optimizing medications in an older person with UI Senior friendly approach 3
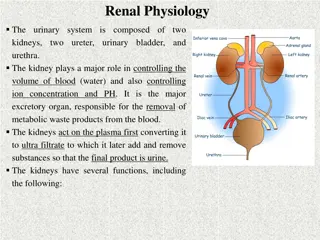
Physiology of Bladder Control Brain (micturition centre) Objectives Physiology of bladder control Sympathetic nervous system (SNS) (beta-adrenergic receptors) SNS inhibition Age-related changes Detrusor muscle Medications causing incontinence Spinal cord (thoracic and lumbar regions) Bladder Medications to treat incontinence Parasympathetic nervous system (PNS) (cholinergic receptors) Case study Internal sphincter (alpha- adrenergic receptors) Summary External sphincter Somatic (pudendal) nerve (Sacral region) Senior friendly approach Urethra Demaagd, G., & Davenport, T.C. (2012). Management of urinary incontinence. P & T : a peer-reviewed journal for formulary management, 37 6, 345-361H. Tannenbaum. Chapter 10. Evidence- Based Geriatric Medicine. 2012. 4
Physiology of Bladder Control Nervous System Control of Bladder Control Objectives Sympathetic Nervous System (SNS) Stores Urine: Alpha-adrenergic constricts internal sphincter Beta-adrenergic relaxes detrusor muscle Physiology of bladder control Age-related changes Somatic Input (via pudendal nerve): External sphincter contraction prevents release Medications causing incontinence PaRasympathetic Nervous System (PNS)- Releases Urine: Cholinergic activation contracts detrusor Coordination with SNS for sphincter relaxation Medications to treat incontinence Case study Frontal lobe and pontine micturition centre Inhibit until physiologically and socially acceptable Summary Senior friendly approach Tannenbaum. Chapter 10. Evidence-Based Geriatric Medicine. 2012. 5
Physiology of Bladder Control - Simplified Objectives Physiology of bladder control Age-related changes Medications causing incontinence Medications to treat incontinence Case study a Summary Senior friendly approach Tannenbaum. Chapter 10. Evidence-Based Geriatric Medicine. 2012. 6
Age-Related Changes to the Genitourinary System that Impact Continence Objectives Bladder wall fibrosis/ impaired collagen and elastin of bladder wall bladder capacity, post-void residual volume from impaired contractility Physiology of bladder control Age-related changes Detrusor instability Medications causing incontinence Altered outflow tract characteristics ( urethral tone, mostly in women) stress incontinence Medications to treat incontinence diurnal Anti-Diuretic Hormone (ADH) release ADH at night nocturia Case study Summary Senior friendly approach Geriatric Review Syllabus 9 Urinary Incontinence Siroky MB. The aging bladder. Rev Urol. 2004;6 Suppl 1(Suppl 1):S3 S7. 7
Medications that Cause Urinary Incontinence and Urinary Symptoms Medication Class Examples Mechanism Objectives Frequency, urgency urge UI Alcohol Physiology of bladder control Sedation, delirium, immobility functional UI Age-related changes Outlet obstruction (men) overflow incontinence -Adrenergic agonists Midodrine, clonidine, methyldopa Medications causing incontinence -Adrenergic blockers Alpha-1 blockers: Reduced internal sphincter tone (women) stress incontinence Flomax and Prazosin (selective), Trazadone (non-selective) Alpha 2:Mirtazapine Medications to treat incontinence ACE inhibitors Ramipril, lisinopril, perindopril Associated cough worsens stress and possibly urge leakage in older adults with impaired sphincter function Case study Summary SGLT-2 Inhibitors Empagliflozin, canagliflozin Urinary frequency, urinary tract infections Senior friendly approach Abrams et al. Incontinence. 5th International Consultation on Incontinence. 5th Edition, 2013. Geriatric Review Syllabus 9 Urinary Incontinence 8
Medications that Cause Incontinence Medication Class Examples Mechanism Impaired emptying, retention overflow UI Anticholinergics oxybutynin, amantadine Objectives Delirium, sedation functional UI Physiology of bladder control Constipation, fecal impaction retention overflow UI Age-related changes Anticholinergic effects retention, overflow UI Antipsychotics Risperidone, haloperidol, quetiapine, olanzapine Medications causing incontinence Rigidity, sedation, and immobility functional UI Calcium channel blockers Nifedipine, amlodipine, diltiazem Impaired detrusor contractility and retention overflow UI Medications to treat incontinence Dihydropyridine agents can cause pedal edema, leading to nocturnal polyuria Case study Summary Cholinesterase inhibitors Donepezil, rivastigmine Urinary frequency and urgency, potential interactions with anticholinergics Senior friendly approach Abrams et al. Incontinence. 5th International Consultation on Incontinence. 5th Edition, 2013. Geriatric Review Syllabus 9 Urinary Incontinence 9
Medications that Cause Incontinence Medication Class Examples Mechanism Urinary retention, fecal impaction urinary retention overflow UI Narcotic analgesics* Hydromorphone, morphine, codeine Objectives Physiology of bladder control Sedation, delirium functional UI NSAIDs Ibuprofen, naproxen Pedal edema causing nocturnal polyuria Age-related changes Sedation, delirium, immobility functional UI Sedative hypnotics* Lorazepam Medications causing incontinence Thiazolidinediones Pedal edema causing nocturnal polyuria Anticholinergic effects urinary retention, overflow UI Tricyclic antidepressants Medications to treat incontinence Sedation functional UI Loop diuretics furosemide Polyuria, frequency, urgency Case study Lithium Polyuria from diabetes insipidus Summary Estrogen (oral) Worsens stress and mixed leakage in women Senior friendly approach Sedation, dizziness functional UI GABAergic agents* gabapentin, pregabalin Pedal edema causing nocturnal polyuria Abrams et al. Incontinence. 5th International Consultation on Incontinence. 5th Edition, 2013. Geriatric Review Syllabus 9 Urinary Incontinence 10
Pharmacological Management of Urinary Incontinence Objectives For most patients, trial of non-pharmacological treatment prior to drug therapy. Physiology of bladder control Consider starting on drug therapy earlier if: Few medications Cognitively intact Significant reduction in patient s quality of life Age <65 years old (more evidence about adverse effects, fewer adverse effects) Few comorbidities Age-related changes Medications causing incontinence Medications to treat incontinence Case study Summary Senior friendly approach Abrams et al. (2017). Incontinence, 6th International Consultation on Incontinence. 11
Medications for Treating Urinary Incontinence Stress Urinary Incontinence: Objectives Topical vaginal estrogen may be useful for postmenopausal women with atrophy or estrogen deficiency Oral/transdermal NOT recommended Caution in women at increased risk of estrogen dependent cancers - Premarin (0.625mg/g vaginal cream) - 0.5g twice/week - Vagifem 10mcg vaginal tab - 1 tab pv twice/week - Estring 2mg vaginal ring 1ring PV every 90days Physiology of bladder control Age-related changes Medications causing incontinence Medications to treat incontinence No approved oral pharmacological therapies in Canada Duloxetine (SNRI antidepressant) is approved in the UK - Consider to treat depression/UI concurrently - May reduce incontinence episodes - 1/3 patients report adverse effects Case study Summary Senior friendly approach NICE clinical guideline 40; October 2006:1- 14. 2 SOGC clinical practice guidelines. J Obstet Gynaecol Can2012 Nov;34(11):1092-101 Mariappan P. Cochrane Database of Systematic Reviews 2005, Issue 3 12
Medications for Treating Urinary Incontinence Mixed Urinary Incontinence: Objectives Treat as per the dominant category (urge/overactive bladder vs stress UI) Physiology of bladder control Age-related changes Medications causing incontinence Medications to treat incontinence Case study Summary Senior friendly approach 13
Medications for Treating Urinary Incontinence Urge Urinary Incontinence/ Overactive Bladder: Objectives Two main classes Antimuscarinics (aka anticholinergics) Beta3-adrenoceptor agonist (mirabegron) Physiology of bladder control Age-related changes Choice of medication based on the patient s comorbidities, current medications, side effect profile of medications tolerability, ease of use, cost/if covered Medications causing incontinence Consider vaginal estrogen in estrogen deficient women (may improve subjective symptoms) Medications to treat incontinence Case study Summary Senior friendly approach NICE clinical guideline 40; October 2006:1- 14. 2 SOGC clinical practice guidelines. J Obstet Gynaecol Can2012 Nov;34(11):1092-101 14
Antimuscarinics Modest efficacy vs placebo UI episodes and symptoms Low cure rates Objectives Physiology of bladder control Contraindications: gastric retention, urinary retention, untreated narrow angle closure glaucoma, myasthenia gravis and supraventricular tachycardia Age-related changes Medications causing incontinence Avoid in those with dementia, those on cholinesterase inhibitors and those on anticholinergic agents Medications to treat incontinence Associated with dementia Cost: Case study Range from $14 per month (oxybutynin IR) to $102 per month (oxybutynin ER) LU code 290 for all except oxybutynin Summary Senior friendly approach Ann Intern Med. 2012;156(12):861-874 SOGC clinical practice guidelines. J Obstet Gynaecol Can2012 Nov;34(11):1092-101 15
Antimuscarinic Agents Start with the lowest dose 4-12 weeks for full effect Titrate prn based on response and side effects Objectives Physiology of bladder control Treatment failure: Check adherence, check tolerability Age-related changes Extended release (ER) preparations or patch minimize side effects, preferred over immediate release (IR) IR useful for prn continence at specific times Medications causing incontinence Medications to treat incontinence Monitoring: side effects and signs of urinary retention Case study Adverse effects: anticholinergic side effects such as dry mouth, constipation, blurred vision for near objects, tachycardia, drowsiness, falls and decreased cognitive function Summary Senior friendly approach Ann Intern Med. 2012;156(12):861-874 Madhuvrata P. Cochrane Database Syst Rev. 2012 16
Antimuscarinic Agents Drug Dosing Notes ER (ditropan XL ): 5mg daily, up to 30mg daily IR: 2.5mg BID, up to 5mg QID ($0.10/tablet) Patch : 36mg, twice/wk Less selective ?more CNS side effects Reduce maximum dose for older adults CYP3A4 metabolized Oxybutynin (Ditropan 2.5mg tab ) dose for moderate renal or hepatic impairment, avoid in severe renal or hepatic impairment Metabolized by CYPs 3A4 and 2D6; max 2 mg daily with strong CYP3A4 inhibitors QTc prolonging avoid if on other QTc prolonging medications or if prolonged QTc Tolterodine (Detrol) ER (Detrol LA): 2mg once daily, up to 4mg once daily ($0.49 / capsule) IR: 1mg BID up to 2mg BID 4mg, up to 8mg ($1.5 per tablet) * active metabolite of tolterodine Fesoterodine (Toviaz) Avoid if soy allergy dose for moderate renal or hepatic impairment CYP3A4 metabolized max 4mg with strong CYP3A4 inhibitors =non-formulary IR = immediate release, ER = extended release - In most cases do not use IR Common CYP3A4 inhibitors: Cyclosporine, grapefruit juice, protease inhibitors, azole antifungals, amniodarone, dronedarone, verapamil, diltiazem, clarithromycin, erythromycin, colchicine Ann Intern Med. 2012;156(12):861-874 17
Antimuscarinic Agents Drug Dosing Notes 5mg once daily, up to 10mg once daily dose for moderate renal or hepatic impairment, avoid in severe hepatic impairment CYP3A4 metabolized; max 5 mg daily with CYP3A4 inhibitors QTc prolonging avoid if on other QTc prolonging medications or if prolonged QTc Solifenacin* (Vesicare) ($0.30 per tab) 7.5mg once daily, up to 15mg once daily ($1.61 per tablet) Darifenacin* (Enablex) CYP3A4 metabolized; maximum 7.5 mg daily with strong CYP3A4 inhibitors dose for moderate hepatic impairment, avoid in severe hepatic impairment IR: 20mg once daily, up to 20mg BID ($0.61 per tab) ER: 60mg once daily Trospium chloride* (Trosec) Take on empty stomach, avoid ETOH for 2hrs dose for reduced renal impairment, avoid in severe renal impairment No CYP metabolism *=newer agents, less blood brain barrier permeability Ann Intern Med. 2012;156(12):861-874 18
Medications for Treating UI Beta3-adrenoceptor agonist: only option = mirabegron (Myrbetriq, $1.46 per tab) Objectives Physiology of bladder control Selective beta receptor stimulation of the detrusor muscle smooth muscle relaxation bladder capacity Age-related changes Ontario Drug Benefits Limited Use (ODB LU) code: 290 Medications causing incontinence Clinical effectiveness similar to antimuscarinics Medications to treat incontinence Contraindications: severe uncontrolled hypertension, severe hepatic impairment, urinary retention Case study Potentially less dry mouth, constipation vs antimuscarinics Summary Senior friendly approach Wagg A, Age Ageing. 2014 Sep;43(5):666-75. NICE https://www.nice.org.uk/guidance/ta290/chapter/4-Consideration-of-the-evidence 19
Mirabegron Good candidates: Objectives Those who do not tolerate or respond to antimuscarinic agents Physiology of bladder control Age-related changes Sensitive to anticholinergic CNS impacts of antimuscarinics including: Dementia patients Those on cholinesterase inhibitors Medications causing incontinence Medications to treat incontinence Contraindication to antimuscarinic In combination with antimuscarinics when persistent symptoms (higher rates of retention) Case study Summary Senior friendly approach 20
Mirabegron Dose: 25 mg daily Increase to 50 mg daily if no effect by two to four weeks If hepatic impairment or CrCl 15-29, max dose is 25mg per day Objectives Physiology of bladder control Age-related changes Side effects: Urinary retention, diarrhea, dizziness, constipation, fatigue, increased blood pressure, increase heart rate, increased QTc Medications causing incontinence Medications to treat incontinence Monitoring: Monitor for urinary retention, consider routine PVR if available Blood pressure elevation Case study Summary Senior friendly approach 21
Case study: Mrs. X Mrs. X is an 87 year old female, living alone with her husband. She has nocturia, stress leakage with chronic cough, urinary frequency and urgency with urge incontinence. Her urge symptoms are most bothersome. She has 2-3 incontinence episodes a day and night time incontinence. Her symptoms impact her quality of life. Objectives Physiology of bladder control Age-related changes Medications causing incontinence She has enacted all non-pharmacological strategies outlined in the sfCare Learning Series for Clinicians: Urinary Incontinence (introductory module) including reduced caffeine, reduce fluid intake in the evening, physical exercise, kegels, pelvic physiotherapy and bladder training. Medications to treat incontinence Mrs. X comes to you to review her options for pharmacological management of her urinary incontinence. Case study Summary Senior friendly approach 22
Case study: Mrs. X Medications Ramipril 2.5mg bid Empagliflozin 10mg daily Amlodipine 5 mg po daily Furosemide 40 mg daily Quetiapine 50mg po qhs Donepezil 10mg po daily Hydromorphone 0.5mg po q8h PRN Tiotropium 18mcg inh daily Diltiazem 120mg po daily Apixaban 5mg po bid Objectives What is urinary incontinence? Prevalence and impact Causes Past Medical History Diabetes (well controlled) Hypertension Osteoarthritis of right knee Mild Alzheimer's Insomnia COPD Atrial Fibrillation Pedal edema How to treat Social History Retired nurse Has private drug coverage under husband s plan Needs assistance with finances and scheduling, otherwise independent Exercises 3x/week Case study Summary Senior friendly approach Questions 23
Case study: Mrs. X What approach would you take in regard to her current medications? Objectives Medication Plan What is urinary incontinence? May lead to cough and worsen stress incontinence substitute for an angiotensin-ll receptor blocker (ARB) Ramipril Prevalence and Urinary frequency consider another anti-diabetic agent Empagliflozin impact Pedal edema nocturia, furosemide prescription discontinue and optimize dose of ARB Amlodipine Causes How to treat Furosemide Discontinue Anticholinergic effects, sedation taper and discuss non- pharmacological approaches to sleep Quetiapine Case study Summary Urinary frequency and urgency discuss pros/cons of discontinuing Donepezil Senior friendly approach Sedation taper and optimize OA without opioids (Tylenol, topical NSAIDs, intraarticular joint injections) Hydromorphone Questions Diltiazem Ensure no overflow/retention, ensure constipation addressed 24
Case Study Mrs. X What approach would you take in regard to prescribing medications for urinary incontinence? Objectives Stress incontinence: Optimize control of COPD, discontinue ACE-inhibitor Try vaginal estrogen (Premarin cream twice weekly) No indication for duloxetine What is urinary incontinence? Prevalence and impact Urge urinary incontinence: Antimuscarinics: special considerations - Mild dementia, use of cholinesterase inhibitor - Anticholinergic side effects additive to quetiapine, tiotropium - Drug-drug interactions diltiazem = CYP3A4 inhibitor (avoid tolterodine, darifenacin, solifenacin) - If this class chosen, trospium chloride likely best candidate cost = (but drug coverage) Causes How to treat Case study Summary Senior friendly approach Questions Mirabegron: ensure blood pressure well controlled 25
Case Resolution Making alterations to Mrs. X s medications leads to partial relief of her symptoms. Objectives She tries per vaginal Premarin cream for 4 weeks which offers limited benefit. What is urinary incontinence? Prevalence and impact After discussing the pros and cons of the oral medications used to treat urge incontinence, she decides to try mirabegron. Causes How to treat Case study While she has no cure of her incontinence, she notes a clinically important reduction in incontinence episodes, reduced urinary urge and frequency, and improved quality of life. Summary Senior friendly approach Questions 26
Summary The pathophysiology behind continence is complex but important to the understanding of how medications worsen or improve bladder control Objectives What is urinary incontinence? Many common medications can contribute to UI in older adults Prevalence and impact Antimuscarinics and beta-3-adrenoreceptor agonists (mirabegron) can be used to improve urge UI symptoms, but cure rates are low. Balance with side effects and cost Causes How to treat Case study There are no approved medications for stress UI Summary Senior friendly approach Questions 27
The senior friendly approach How all healthcare providers can address urinary incontinence using a senior friendly care approach Objectives Recruit healthcare providers with the knowledge, skills, and attitude to provide comprehensive medication review regarding UI Organizational What is urinary incontinence? Organizational Support Support Prevalence and impact Prescribe medications impacting UI and treat UI in alignment with personal goals Emotional & Emotional & Behavioural Environment Behavioural Environment Causes Processes Processes of Care of Care How to treat Do not deny access to research studies on medications for UI based on age Case study Ethics in Clinical Ethics in Clinical Care and Research Care and Research Summary Senior friendly approach Physical Ensure optimal environment for independent medication administration Physical Environment Environment Questions 28
Discussion questions Objectives What medications have you used to treat urinary incontinence? What have been your experiences with benefit and side effects? What is urinary incontinence? Prevalence and impact Causes What is one thing you can do differently as a result of reviewing this module? How to treat Case study Summary Senior friendly approach Questions 29
The sfCare Learning Series received support from the Regional Geriatric Programs of Ontario, through funding provided by the Ministry of Health and Long-Term Care. V1 January 2020