Ultrasound Rounds: Clinical Case Study of 31-Year-Old Female with Abdominal Pain
31-year-old female presents to the emergency department with sudden onset severe abdominal pain localized to the RLQ. Her clinical history and examination findings are detailed, along with lab results showing positive beta-hCG. Ultrasound examination techniques including transabdominal and transvaginal approaches are described for further evaluation of the patient's condition.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Ultrasound rounds Sample Journal Club Presentation
Clinical case 31 y/o female presents to the emergency department 6 hour history of abdominal pain. The pain was of sudden onset, has been constant, 6/10 in severity, and it is well-localized to the RLQ. Vital Signs: HR 98, RR 16, 116/72, T 37.0, sats 99% on room air
Clinical Case Hx: She has had no urinary symptoms, no N/V, and she denies any recent febrile illness. Her last bowel motion was earlier today and was normal . She is pretty sure her LMP was 6 weeks ago. She denies any vaginal discharge or bleeding, and she has no known history of STI. She is not using any contraception.
Clinical case On examination: She appears fairly comfortable. No acute distress. She winces slightly when you palpate the RLQ, but there is no evidence of peritonitis. You don t appreciate any masses. A pelvic exam is negative for any CMT or palpable adnexal masses.
labs Nurse informs you that the urine is beta-hCG positive Subsequent quantitative results: Beta-hCG 1200 mIU/mL CBC Hgb 121, WBC 9, plts 156 G&S A+, Ab screen negative
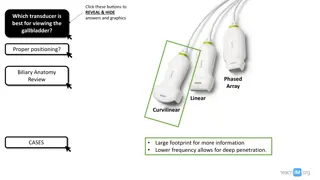
What now? Time for some ultrasound!! Transabdominal OB EDE: - curved array probe - bladder full to provide optimum acoustic window - Advantage: More convenient and improved patient comfort, easily comprehensible spatial orientation
TA OB ede1 (1) Place the probe in the longitudinal plane in the midline, just above the pubic symphysis. (2) Identify the bladder and juxtaposed uterus. (3) Center the uterus by adjusting the depth, and heeling the probe cephalad or caudad. (4) Sweep through the uterus and the endometrial stripe. (5) Rotate the probe 90 counterclockwise and sweep through the uterus in the transverse plane.
TV OB EDE 1 Endocavitary probe, usually 5.0-7.5 MHz. No need for acoustic windows. Higher frequency = better axial resolution. Use sterile gel, and avoid air bubbles in the cover tip.
TV OB EDE 1 (1) Insert the probe in the vagina in the sagittal plane. (2) Identify the bladder. (3) Identify the uterus and center it on the screen. (4) Sweep through the uterus and the endometrial stripe. (5) Rotate the probe and sweep through the uterus in the coronal plane.
OB ede1 Criteria for confirming an IUP: (1) Bladder-uterine juxtaposition (2) Myometrial mantle > 5mm (3) Decidual Reaction (strongly echogenic white lining) (4) Gestational Sac (anechoic fluid collection within the decidual reaction) (5) Yolk Sac within the Gestational Sac ***The conclusion drawn from this scan is binary: either IUP or NDIUP, there is no middle ground.
Clinical case (reassess) You complete the TA + TV OB EDE on the patient. You visualize a full bladder with good vesico-uterine juxtaposition. You visualize the uterus, including the endometrial stripe, in all of the pertinent views. There is no identifiable decidual reaction, no gestational sac, and no evidence any yolk sac. You document NDIUP in the patient s chart.
Practice points Is our patient appropriate for an urgent surgical/OB consult? Does the magnitude of the quantitative beta-hCG level help us with our diagnosis? Does it influence our management plan?
literature Doubilet, Peter et al. Further Evidence Against the Reliability of the Human Chorionic Gonadotropin Discriminatory Level Where: Brigham and Women s Hospital, USA When: January 1, 2000 through December 31, 2010 What: retrospective analysis reviewed charts from women who had been found to have a positive Beta with a NDIUP sought correlations between beta-levels and subsequent pregnancy outcomes.
subjects PATIENTS: women who met the following criteria (1) Serum -hCG testing and transvaginal sonography were performed on the same day; (2) -hCG was positive and sonography showed no intrauterine fluid collection; (3) a live intrauterine pregnancy was subsequently documented on a follow-up sonogram showing embryonic or fetal cardiac activity.
Scans 1stTM First-trimester outcomes: (1) live if there was either a live birth or a second- or third-trimester scan showing cardiac activity. (2) demise if there was a first-trimester scan showing spontaneous demise or a note in the medical record documenting a miscarriage. (3) uncertain if neither of these criteria were met.
Term outcomes Final pregnancy outcomes: (1) liveborn if a live baby was delivered after 25 weeks gestation (2) demise if there was a spontaneous pregnancy loss at any gestational age (3) uncertain if neither of these criteria were met.
results 202 patients met the inclusion criteria: 162 had -hCG levels below 1000 mIU/mL 19 had levels of 1000 to 1499 mIU/mL 12 had levels of 1500 to 1999 mIU/mL 9 had levels > 2000 mIU/mL.
results First-trimester: 174 (89.7%) of the women had a live pregnancy at the end of the 1sttrimester 18 (10.3%) had a spontaneous 1st-trimester pregnancy loss Term Outcomes: Of 158 cases with known final pregnancy outcomes, 135 (85.4%) were live born.
Conclusions?? Take home message: There was no significant relationship between initial -hCG level and either first-trimester outcome or final pregnancy outcome (p> .05) Interesting findings: The highest -hCG was 6567 mIU/mL, and the highest value that preceded a liveborn term baby was 4336 mIU/mL.
Discussion discriminatory zone Term coined by Kadar et al. in 1981 Seminal paper assessing the visibility of a normal intrauterine pregnancy on sonography in relation to the hCG level TA OB scans only No normal IUP visualized with levels <6000 They concluded that absence of a gestational sac above this level signifies ectopic pregnancy
discussion discriminatory zone since decreased with improved U/S resolution Since Kadar s paper, many hospitals in the U.S. began to employ protocols based on these thresholds This paper sought to debunk this practice
Critical appraisal Evidence of selection bias? Sampling bias inherent given the inclusion criteria Study design was retrospective and non-randomized Participant attrition Unclear prevalence given unknown total population from which the study sample was obtained.
Critical appraisal Who was performing the scans? Scans were generally performed by a sonographer and interpreted by a sonologist who subspecializes in sonography or emergency radiology Sonologist was most often in the scanning room for at least part of the transvaginal examination For all cases stored images and video clips were reviewed by the sonologist Proficiency/competency not objectively disclosed/tested
Critical appraisal How were the scans performed? Both transabdominal and transvaginal imaging performed, the latter using broadband transducers with frequencies of 5-9 MHz Images and video clips of the entire uterus and both adnexal regions were stored Largely meeting standard of care Lacks detail re: prep/views and IUP criteria used
Critical appraisal Indeterminates? These were OB scans so only IUP vs NDIUP Study selected NDIUPs only in patient s with -hCG < than or > than the apparent discriminatory zone of 1000-2000 Definition of NDIUP no intrauterine fluid collection Unclear how many 1st trimester scans in total were performed during the study period or how many were confirmed IUPs NO DENOMINATOR
Critical appraisal Quality assurance process? No formal QA process documented, although For cases with -hCG > 2000 mIU/mL stored images and clips were reviewed to assess the quality of the scan and determine whether the endometrium had been well seen Of the 9 patients with - hCG > 2000 mIU/mL All scans were adequate and complete , and none had fibroids or other anatomic features that interfered with visualization of the endometrium Criteria for determining a adequate or complete scan was not explicitly defined
Critical appraisal What was the gold standard? For 1sttrimester scans: follow-up imaging (either repeat 1stor 2nd/3rdtrimester scans) documenting fetal cardiac activity/miscarriage in medical records For final pregnancy outcomes: birth records or medical records documenting spontaneous loss at any gestational age Relationship between initial - hCG level and 1st trimester and final pregnancy outcomes assessed using the Fisher exact test and logistic regression **Unclear if laparoscopies performed to rule out ectopics
Critical appraisal Blinding? No intentional blinding of sonographers to the patients examination or with regards to the gold standard Follow-up? Not formalized observational study only 28 of the study cases uncertain 1st trimester outcome Of the remaining 174: 156 (89.7%) alive at the end of 1st trimester, and 18 (10.3%) had a spontaneous 1sttrimester pregnancy loss
Critical appraisal Limitations? Observational study only Lack of statistical rigor in design/methods EDE definition of IUP vs NDIUP not utilized Wide threshold for discriminatory zone with small sample sizes in higher -hCG subgroups (>1000) poorly powered Patients were asymptomatic Practice differences between Canada and U.S. with regards to management/policies
Critical appraisal What could have been done differently?.... Attempt a prospective study with formalized follow-up scans Ensure standardized methods of scanning/QA protocols, and documentation of gold standards, GA Characterize the denominator to assess for prevalence of missed early IUPs given -hCG above the discriminatory zone with an empty uterus on initial scan Perform analysis on individual subgroups Recruit larger sample sizes
Critical appraisal Will this impact our practice? Less likely to manage as an ectopic empirically given a discrete -hCG value above the discriminatory zone within the 1st trimester and no intrauterine collection on formal TVUS as many can progress to live birth
References 1. Doubilet PM, Benson CB. Further evidence against the reliability of the human chorionic gonadotropin discriminatory level. J Ultrasound Med 2011; 30:1637 1642. 2. Gilovich T. Too much from too little: the misinterpretation of incomplete and unrepresentative data. In: How We Know What Isn t So: The Fallibility of Human Reason in Everyday Life. New York, NY: The Free Press; 1991:29 48. 3. Kadar N, Bohrer M, Kemman E, Shelden R. The discriminatory hCG zone for endovaginal sonography: a prospective, randomized study. Fertil Steril 1994; 61:1016 1020. 4. Kadar N, DeVore G, Romero R. Discriminatory hCG zone: its use in the sonographic evaluation for ectopic pregnancy. Obstet Gynecol 1981; 58:156 161.