Understanding Histamine and Antihistaminics: A Comprehensive Overview
Histamine is a vital autacoid synthesized and stored in mast cells, playing a key role in various physiological processes and allergic reactions. This article delves into its synthesis, storage, release, and receptors like H1, H2, and H3, along with the pharmacology of antihistamines. Explore the intricate mechanisms and biological activities of histamine and its modulation in different tissues and systems.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Histamine and Antihistaminics Prof. Sanjay Khattri Department of Pharmacology & Therapeutics King George s Medical University 1
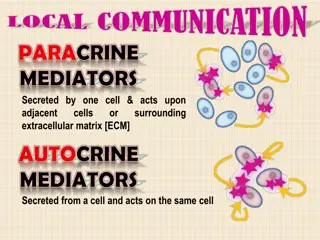
Autacoids These are diverse substances produced by wide variety of cells, having intense biological activity, but act locally at the site of synthesis and release Types of autacoids: Amine autacoids - Histamine, 5-HT (Serotonin) Peptide autacoids - Plasma kinins (Bradykinin, Kallidin), Angiotensinogen Lipid autacoids - Prostaglandins, Leukotrienes, PAF 2
Histamine - Introduction Meaning tissue amine (histos tissue) abundantly present in animal tissues also in plants like stinging nettle Mediator of hypersensitivity and tissue injury reaction Physiological role The primary site the mast cell granules (or basophils) skin, intestinal and gastric mucosa, lungs, liver and placenta Other sites central nervous system: neurotransmitter the fundus of the stomach: major acid secretagogues, epidermis, gastric mucosa and growing regions also blood, body secretions, venoms & pathological fluids 3
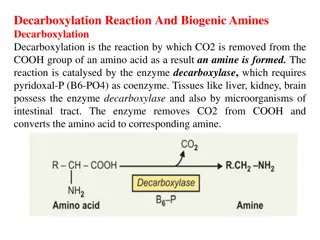
Synthesis & Storage Histamine is formed by the decarboxylation of the amino acid histidine by the enzyme L-histidine decarboxylase, found in every mammalian tissue that contains histamine. The chief site of storage in most tissues is the mast cell; in the blood, it is the basophil. These cells synthesize histamine and store it in secretory granules. 4
Histamine synthesis, storage and release Metabolized by P450 system, 2 pathways: Methylation to N-methyl histamine (N-methyl transferase), and to N-methyl imidazole acetic acid (MAO) - eliminated in urine Oxidative deamination to imidazole acetic acid (DAO), and to imidazole acetic acid riboside - eliminated in urine In mast cells held by acidic protein and heparin (-ve charged) histamine is +ve charged Ineffective orally liver destroys all absorbed from intestine 5
Histamine Receptors H1 H2 H3 Selective agonist 2-Methylhistamine 4-Methylhistamine -Methylhistamine Selective antagonist Mepyramine Cimetidine Ranitidine Thioperamide Effector Pathway IP3/DAG cAMP Ca++ influx K+ channel activation Smooth muscle (intestine, airway, uterus)-contraction Blood vessels NO and PGI2 release Vasodilatation Smooth muscle of large vessels-vasoconstriction Afferent nerves stimulation Ganglion cells stimulation Adrenal medulla CA release Brain - transmitter Gastric glands acid secretion Blood vessels (smooth muscle) dilatation Heart: Atria: + chronotropy and ventricles: + inotropy Uterus relaxation Brain (post synaptic) impulse Brain inhibition of Histamine release- sedation Lung, spleen, gatric mucosa decrease histamine release Ileum inhibition of Ach release Distribution 6
Pharmacological actions of Histamine CNS - - H3 agonists reduce the release of acetylcholine, amine, and peptide transmitters in various areas of the brain and in peripheral nerves Histamine is a powerful stimulant of sensory nerve endings, especially those mediating pain and itching.. No BBB penetration On Intracerebrovascular injection: * in BP, cardiac stimulation * Vomiting, ADH release 7
Histamine - Pharmacological actions Blood vessels: Dilatation of small vessels arterioles, capillaries and venules SC administration flushing, heat, increased HR and CO little fall in BP Rapid IV injection: Fall in BP early (H1) and persistent (H2) only H1 effect with low dose Dilatation of cranial vessels H1 component vasodilatation mediated indirectly by EDRF .. But H2 component - mediation is directly on smooth muscle of blood vessels Larger arteries and veins constriction mediated by H1 receptor Increased capillary permeability exudation of plasma 8
Histamine The Triple Response Subdermal histamine injection causes: 1. Red spot (few mm) in seconds: direct vasodilation effect , H1 receptor mediated 2. Flare (1cm beyond site): axonal reflexes, indirect vasodilation, and itching, H1 receptor mediated 3. Wheal (1-2 min) same area as original spot, edema due to increased capillary permeability, H1 receptor mediated 9
Pharmacological actions Heart : It increases the force of contraction of both atrial and ventricular muscle slow atrioventricular (AV) conduction Atria: +ve chronotropy Ventricles: +ve inotropy Due to H2 receptors Slowed AV conduction (-ve dromotropic effect) which involves mainly H1 receptors If histamine is given i.v., direct cardiac effects of histamine are overshadowed by baroreceptor reflexes elicited by the reduced blood pressure Overall: H1 decreased AV conduction; H2 - Increased Chronotropy and automaticity 10
Pharmacological actions (contd.) Visceral Smooth Muscles - Bronchoconstriction - Abd. Cramps & colic Glands - in gastric secretion Sensory nerve endings - IV itching , Pain Autonomic ganglia & Adrenal medulla - Release of Adrenaline secondary in BP 11
Pathophysiological roles Gastric Secretion Allergic Phenomena As transmitter Inflammation Tissue growth and repair 12
Uses Of Histamine No Therapeutic Use Diagnostic Uses: * Secreting (Acid) capacity of stomach * Pheochromocytoma * Bronchial hyper-reactivity in Asthmatics H1 Selective Histamine Analogue: Betahistine(used to control vertigo in Meniere s disease) 13
Antagonists of Histamine Physiological antagonists : Adrenaline effects are opposite to effects of histamine Histamine release Inhibitors : Mast cell stabilizers : Cromoglycate Histamine receptor blockers : H1 blockers and H2 blockers 14
H1-RECEPTOR ANTAGONISTS 1st Generation: Highly sedatives: Diphenhydramine, Dimenhydrate, Promethazine and Hydroxyzine Moderately: Pheniramine, Cyproheptadine, Meclizine, Buclizine and Cinnarizine Mild: Chlorpheniramine, Dexchlorpheniramine, Dimethindene, Cyclizine, Clemastine 2nd Generation: Fexofenadine, Loratidine, Desloratidine, Cetrizine, Levocetrizine, Azelastine, Mizolastine, Ebastine and Rupatidine 15
Antihistaminics (Pharmacokinetics) Absorption: Antihistaminics (H1 receptor antagonists) are well absorbed from oral and parenteral routes Distribution: widely in the body and enter brain. Newer compounds penetrate the brain poorly. Metabolism: In liver Excretion: In urine 17
Pharmacological Actions CNS depression: (More with first generation) Sedation and drowsiness Some have antiemetic and antiparkinsonian effects Antiallergic action: Type- I reactions are suppressed Anticholinergic actions generation) Dryness of mouth , Blurring of vision Constipation Urinary retention (More with first 18
Pharmacological Actions BP -Fall in BP with IV injection (all) but not with Oral direct smooth muscle relaxation or adrenergic blockade Antagonism of Histamine - Effectively block: * Bronchoconstriction * Contraction of sm. Mus. * Triple response - 19
Pharmacological Actions Antimotion sickness effect: Dimenhydrinate, Promethazine Antiemetic: Promethazine Antiparkinsonism: Diphenhydramine, orphenadrine, promethazine(IV) Antivertigo: cinnarizine 21
Antihistaminics (Uses) Allergic disorders, Other conditions involving histamine: Insect bite, Ivy poisoning etc. Pruritides Common cold Motion sickness Vertigo Pre anesthetic medication Cough Parkinsonism Acute muscle dystonias As sedative, hypnotic, anxiolytic 22
H2 receptor antangnists Cimetidine , Ranitidine, Famotidine Clinical uses- Peptic Ulcer and Duodenal Disease Gastric Ulcer: reduce symptoms promote healing for benign gastric ulcers Gastroesophageal Reflux Disorder (erosive esophagitis) Hypersecretory Disease: Zollinger-Ellison syndrome: acid hypersecretion -- caused by gastrin-secreting tumor Systemic mastocytosis and multiple endocrine adenomas: 23
THANK YOU 24