Understanding Haemodynamic Consequences of Acute Pulmonary Embolism
Haemodynamic consequences of acute pulmonary embolism (PE) include increased mean pulmonary artery pressure, rise in right ventricular preload and end-diastolic pressure, risk of right ventricular failure, and decreased pulmonary blood flow leading to low systolic blood pressure. Arterial hypoxia can result from factors like decreased cardiac output, low mixed venous PaO2, and inadequate oxygenation. A patient with confirmed PE may require risk stratification using clinical risk scores like PESI and sPESI for appropriate management decisions.
- Pulmonary Embolism
- Haemodynamic Consequences
- Arterial Hypoxia
- Risk Stratification
- Clinical Risk Score
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Which of the following is not a haemodynamic consequence of acute PE: 1. Mean PAP increases once at least 50% of the vascular bed is occluded due to clot 2. Rise in PAP leads to increase in RV preload and subsequent increase in RV end diastolic pressure 3. RV will fail if PAP acutely reaches 40mmHG or above 4. A rise in PAP leads to decrease in Pulmonary Blood flow and resulting decrease in LV filling and low systolic BP 5. Low mixed venous PaO2 is one of the mechanisms of hypoxia in PE
Which of the following is not a haemodynamic consequence of acute PE: 1. Mean PAP increases once at least 50% of the vascular bed is occluded due to clot 2. Rise in PAP leads to increase in RV preload and subsequent increase in RV end diastolic pressure 3. RV will fail if PAP acutely reaches 40mmHG or above 4. A rise in PAP leads to decrease in Pulmonary Blood flow and resulting decrease in LV filling and low systolic BP 5. Low mixed venous PaO2 is one of the mechanisms of hypoxia in PE
Arterial Hypoxia 1. Decreased Cardiac Output 2. Low mixed venous PaO2 3. Increased perfusion to remaining alveoli and inadequate oxygenation of this blood
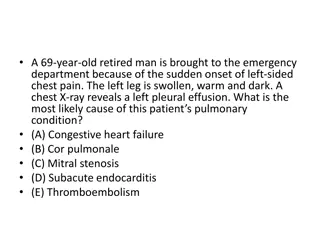
A patient presents to Ambulatory Care from the GP surgery with pleuritic chest pain and a raised D-Dimer. She is 67, was fully treated for breast cancer 10 years ago with no recurrence; she has no other PMH. Her HR is 105, BP 115 systolic, sats 94% on RA. She has a confirmed PE on CT with some suggestion of RHS. What is her sPESI Score 0 1 2 3 4 5
A patient presents to Ambulatory Care from the GP surgery with pleuritic chest pain and a raised D-Dimer. She is 67, was fully treated for breast cancer 10 years ago with no recurrence; she has no other PMH. Her HR is 105, BP 115 systolic, sats 94% on RA. She has a confirmed PE on CT with some suggestion of RHS. What is her sPESI Score 0 1 2 3 4 5
Risk Stratification BTS recommends that patients with a confirmed PE should be risk stratified using validated clinical risk score. Options: PESI, sPESI, Hestia criteria. Clinical Exclusion Criteria If PESI or sPESI is low, OP Rx can be used, with followinexclusion crieteria: 1. Haemodynamic instability 2. Sats <90% 3. Active bleeding/risk of major bleed 4. Already anticoagulated prior to PE 5. Severe pain 6. Other co-morbidities requiring admission 7. CKD 4 or 5 8. HIT within 1 year 9. Social reasons
A patient presents to Ambulatory Care from the GP surgery with pleuritic chest pain and a raised D-Dimer. She is 67, was fully treated for breast cancer 10 years ago with no recurrence; she has no other PMH. Her HR is 105, BP 115 systolic, sats 94% on RA. She has a confirmed PE on CT with some suggestion of RHS. What is the next stage of your plan for her? 1. Request an ECHOcardiogram to determine if she can be discharged 2. Send troponin and judge suitability for discharge on result 3. Admit to RSU/CCU and monitor overnight 4. Discharge home with follow up ECHO in 4 weeks 5. Admit to acute medicine or respiratory ward
A patient presents to Ambulatory Care from the GP surgery with pleuritic chest pain and a raised D-Dimer. She is 67, was fully treated for breast cancer 10 years ago with no recurrence; she has no other PMH. Her HR is 105, BP 115 systolic, sats 94% on RA. She has a confirmed PE on CT with some suggestion of RHS. What is the next stage of your plan for her? 1. Request an ECHOcardiogram to determine if she can be discharged 2. Send troponin and judge suitability for discharge on result 3. Admit to RSU/CCU and monitor overnight 4. Discharge home with follow up ECHO in 4 weeks 5. Admit to acute medicine or respiratory ward
BTS Guidance on risk stratification Caveats Measurement of RV:LV ratio or assesment of RV function on echocardiogram is not obligatory to identify low risk However, normal cardiac biomarkers identify low risk patients with abnormal imaging findings (elevated markers should prompt admission) B/L US, ECG, D-Dimer or lactate are not useful at identifying those at low risk of adverse outcomes Patients with suspected PE should where reasonable have investigation the same day. If not, anticoagulation and OP imaging within 24 hours for those who have been deemed low risk.
With regards to recent research into anticaogulation in PE, which of the following statements is false: 1. DOACs are non-inferior to LMWH/VKA in the treatment of PE 2. In the treatment of acute VTE or PE, DOACs were associated with significantly less bleeding 3. Single dose DOAC regimes offer faster time to therapeutic anticoagulation 4. BTS guidelines suggest that in confirmed PE patients should be offered a single drug regime 5. Patients with suspected PE may be treated in OP setting Apixaban or Rivaroxaban as an altenative to LMWH
With regards to recent research into anticaogulation in PE, which of the following statements is false: 1. DOACs are non-inferior to LMWH/VKA in the treatment of PE 2. In the treatment of acute VTE or PE, DOACs were associated with significantly less bleeding 3. Single dose DOAC regimes offer faster time to therapeutic anticoagulation 4. BTS guidelines suggest that in confirmed PE patients should be offered a single drug regime 5. Patients with suspected PE may be treated in OP setting Apixaban or Rivaroxaban as an altenative to LMWH
Options for OP management of confirmed PE 1. Apixaban 2. Rivaroxaban 3. LMWH and Edoxaban 4. LMWH and Dabigatran
A 36 year old female presents to Ambulatory care with small volume Peripheral PE, there are no obvious provoking factors, she takes no regular medications. Examination and systemic enquiry are normal, no FH, she is up to date with cervical smear. She was started on anticoagulation by her GP and you have continued it. With regards to follow up, which is the most appropriate next course of action? 1. Arrange a Abdominal-pelvic CT scan to look for underlying malignancy 2. Advise anticoagulation for 6months and send her home from ambulatory care with patient leaflet 3. Follow up in PE clinic and consider performing thrombophilia screen as OP 4. Arrange ECHO and PE clinic follow up 5. Send a thrombophillia screen
A 36 year old female presents to Ambulatory care with small volume Peripheral PE, there are no obvious provoking factors, she takes no regular medications. Examination and systemic enquiry are normal, no FH, she is up to date with cervical smear. She was started on anticoagulation by her GP and you have continued it. With regards to follow up, which is the most appropriate next course of action? 1. Arrange a Abdominal-pelvic CT scan to look for underlying malignancy 2. Advise anticoagulation for 6months and send her home from ambulatory care with patient leaflet 3. Follow up in PE clinic and consider performing thrombophilia screen as OP 4. Arrange ECHO and PE clinic follow up 5. Send a thrombophillia screen
Recommendations for follow up in PE NICE recommend considering further investigations for cancer with an abdomino- pelvic CT and a mammogram for women in all those aged >40 with a first episode of unprovoked PE or DVT. Hasn t shown to reduce cancer related mortality so far in studies
Thrombophillia Screening Consider testing: - Recurrent VTE - <40 years old with no obvious risks - VTE secondary to pregnancy/OCP/HRT - Unusual site (cerebral, mesenteric, portal, or hepatic veins) Don t test if: On lifelong anticoagulation/provoked clot NB Tests for all thrombophillias except Factor V Leiden and Prothrombin Gene Defect must be done off anticoagulation Thrombophillias AntiPhospholipid Syndrome AntiThrombin III Prothrombin Gene Defect Protein C or S Deficiency Factor V Leiden