UK Survey on Endovascular Treatment of Acute Pulmonary Embolism
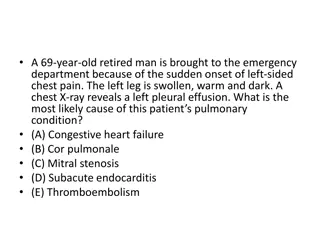
Acute pulmonary embolism (PE) is a significant issue in hospitalized patients, with current treatments focusing on anticoagulation and systemic thrombolysis. Surgical treatments have shown poor outcomes, leading to a rise in endovascular techniques aimed at reducing clot burden. A survey conducted in the UK evaluated practice patterns and preparedness for endovascular therapy in patients with high-risk PE features. The survey covered geographical spread of respondents, availability of catheter-directed therapies, service design, institutional treatment pathways, and barriers to uptake of such therapies.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
U K s u r v e y o f c a t h e t e r U K s u r v e y o f c a t h e t e r d i r e c t e d e n d o v a s c u l a r d i r e c t e d e n d o v a s c u l a r t r e a t m e n t o f a c u t e t r e a t m e n t o f a c u t e p u l m o n a r y e m b o l i s m ( P E ) p u l m o n a r y e m b o l i s m ( P E ) Nadir Khan, Ali Zafar and James Harding on behalf of the Audit and Registry Committee of the British Society of Interventional Radiology
Disclosures The authors declare no conflict of interest. 2 BSIR 2023
Introduction Acute pulmonary embolism (PE) is significant cause of morbidity and mortality in hospitalized patients [1]. Current standard treatments are anticoagulation and systemic thrombolysis for sub-massive and massive PE [2]. Open surgical treatments have generally poor outcomes [3]. Increasing role of endovascular techniques which aim to reduce clot burden [4, 5]: Catheter mediated thrombus fragmentation Catheter mediated thrombus aspiration Rheolytic thrombectomy Catheter directed thrombolytic infusion Ultrasound assisted thrombolytic infusion 3 BSIR 2023
Purpose To evaluate practice patterns in the UK and preparedness for endovascular therapy of patients with acute PE with high risk (massive) and intermediate high-risk features. 4 BSIR 2023
Methods and Materials Electronic survey created using Survey Monkey, approved by the BSIR Audit and Registry Committee. Survey was distributed to members of the BSIR by email during April 2023 and remained open for 4 weeks. Data were analyzed using Microsoft Excel 365. 5 BSIR 2023
Methods and Materials A total of 22 questions were included in the survey. Data gathered on: Geographical spread of respondents Type of hospital settings Availability of catheter directed therapies for PE Service design including PE response teams (PERT) Institutional treatment pathways Key clinical decision-making factors Barriers to uptake of CDTs. 6 BSIR 2023
Results University / Teaching hospital / Tertiary referral centre 59% 59% Total responses 58 58 Consultant 88% 88% Fellow 3% 3% Institutions 44 44 Local general hospital / DGH / Secondary 41% 41% Trainee 9% 9% 7 BSIR 2023
Results Geographical distribution of responders of the survey Scotland 7% North-West England 9% North-East & Yorkshire 9% Wales 2% London 17% South-East England 17% Midlands 24% 8 BSIR 2023
Results 29/58 (50%) of responders offered catheter directed PE intervention at their local institutions. 25/29 (96%) responses indicated that IRs offered CDT as the main / primary operators. Potential barriers to providing this service Of the 29 who did not offer CDT, 12 (41%) (41%) are considering offering this in the future 20/29 (69%) offer CDT during both normal working hours and out-of- hours 12 9 BSIR 2023
Results 18/29 (62%) responded to have a referral pathway in their hospital setting for acute PE management with catheter directed therapies. 12/29 (41%) had a PE response team (PERT) in their local setting. 20/29 (80%) would offer CDT to intermediate high risk or high-risk patients. Settings in which patients are typically managed in the peri- operative period Types of catheter-directed therapy being utilized Catheter-directed thrombolysis Methods utilized to risk stratify patients for acute PE Clinical status (Shock or hypotension) 96.30% 80.77% Intensive care unit 76.92% Ultrasound-assisted CDT (USAT) 26.92% Pulmonary Embolism Severity Index (PESI) 51.85% Large-bore thrombo-aspiration (e.g. FlowTriever, AngioVac) 57.69% Signs of RV dysfunction on imaging 85.19% High dependency unit 19.23% Small-bore thrombo-aspiration (e.g. Indigo, AngioJet) Other (please specify) 38.46% Laboratory Markers (e.g. troponin I or T, NT-proBNP) 59.26% Ward level care 3.85% 3.85% Others 14.81% 10 BSIR 2023
Conclusions This is the first study which gathers information on availability and preparedness for delivery of catheter directed therapies for management of acute PE in the United Kingdom. There has been significant uptake of new technologies although there remains some skepticism from the interventional radiology community in regard to both the clinical benefit and cost effectiveness of these procedures. High quality evidence (e.g. RCTs) needed to evaluate clinical outcomes and cost effectiveness. BSIR in collaboration with other relevant societies is well positioned to inform national guidelines as to the appropriate use of catheter directed therapies in acute PE . 11 BSIR 2023
References 1) Pulido T, Aranda A, Zevallos MA, Bautista E, Mart nez-Guerra ML, Santos LE, Sandoval J. Pulmonary embolism as a cause of death in patients with heart disease: an autopsy study. Chest. 2006 May;129(5):1282-7. doi: 10.1378/chest.129.5.1282. PMID: 16685020. 2) Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest [Internet]. American College of Chest Physicians; 2016 [cited 2020 Sep 7];149:315 52. Available from: 3) Lee T, Itagaki S, Chiang YP, et al. Survival and recurrence after acute pulmonary embolism treated with pulmonary embolectomy or thrombolysis in New York State, 1999 to 2013. J Thorac Cardiovasc Surg 2018; 155: 1084 1090.e12 4) Naidu, S., Knuttinen, M., Kriegshauser, J., Eversman, W., & Oklu, R. 2017 Sep 28. Rationale for catheter directed therapy in pulmonary embolism. Cardiovascular Diagnosis and Therapy. [Online] 7:3 5) Nosher JL, Patel A, Jagpal S, Gribbin C, Gendel V. Endovascular treatment of pulmonary embolism: Selective review of available techniques. World J Radiol. 2017 Dec 28;9(12):426-437. doi: 10.4329/wjr.v9.i12.426. PMID: 29354208; PMCID: PMC5746646. 12 BSIR 2023