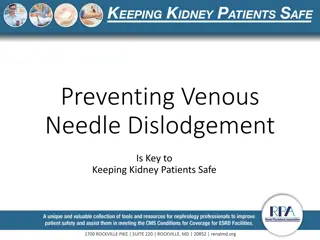
Understanding Venous Thromboembolism in Orthopedic Patients
This educational content covers the basics of deep vein thrombosis (DVT) and pulmonary embolism (PE), including definitions, pathophysiology, risk factors, prevention strategies, diagnosis, and treatment. Traumatic and non-traumatic risk factors for VTE in orthopedic patients are discussed, emphasizing the importance of timely recognition and intervention to prevent complications.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
VENOUS THROMBOEMBOLISM JOHN WESTON MD TENWEK HOSPITAL, BOMET KENYA Core Curriculum V5
Objectives Define DVT and PE and understand the basic pathophysiology Know risk factors for VTE in the orthopedic patient Understand evidence-based prevention strategies Diagnose VTE in a timely fashion Understand treatment strategies for DVT/PE Core Curriculum V5
Definitions Deep Vein Thrombosis (DVT) A pathologic coagulation of blood within a deep vein in an extremity Commonly in the lower extremity Popliteal fossa or proximal at highest risk of embolization Pulmonary Embolus (PE) A pathologic coagulation of blood within a pulmonary artery Ranges from small/subsegmental to massive Core Curriculum V5
Pathophysiology Coagulation Blood transforms from liquid to fibrin based clot Relies on interplay of endothelium, platelets, and circulating coenzymes Hemostasis is a balance between clot formation and dissolution Pathologic coagulation = thrombosis Ahsan ZS, Firoozibadi R. 2020. Venous Thromboembolic Disease in Patients with Skeletal Trauma. Tornetta, Paul, III, Rockwood and Green s Fractures in Adults 9e, Wolters Kluwer, 2020 Core Curriculum V5
Pathophysiology Virchow s Triad Endothelial injury Stasis Hypercoagulable state All three often present in patients with skeletal trauma Ahsan ZS, Firoozibadi R. 2020. Venous Thromboembolic Disease in Patients with Skeletal Trauma. Tornetta, Paul, III, Rockwood and Green s Fractures in Adults 9e, Wolters Kluwer, 2020 Core Curriculum V5
Traumatic Risk Factors Polytrauma Increasing Injury Severity Score Increased rates of VTE Blood transfusion Spinal cord injury Chest injury Head injury Core Curriculum V5
Fracture Specific Risk Factors Orthopedic trauma patients have 69% incidence of VTE in the absence of prophylaxis Pelvis and Acetabular fractures at greatest risk More proximal lower extremity fractures = greater risk 40% femoral shaft 43% tibial plateau 22% tibial shaft 12.5% tibial plafond Core Curriculum V5
Non-traumatic Risk Factors Age > 55 years Obesity Diabetes mellitus Malignancy Coagulopathy Tobacco use Oral contraceptives, hormone replacement Core Curriculum V5
Risk Assessment Caprini Index Establishes composite individual risk Stratifies patients into low (0-2 pts), moderate (3-4), high (5-8), or highest risk (>8) Major lower extremity fracture = high risk Moderate risk or greater may warrant chemoprophylaxis Ahsan ZS, Firoozibadi R. 2020. Venous Thromboembolic Disease in Patients with Skeletal Trauma. Tornetta, Paul, III, Rockwood and Green s Fractures in Adults 9e, Wolters Kluwer, 2020 Core Curriculum V5
Prevention Three primary modalities Mechanical Prophylaxis Inferior Vena Cava Filters Chemoprophylaxis Core Curriculum V5
Prevention Mechanical Prophylaxis Intermittent Pneumatic Compression (IPC) Stimulates venous flow in the extremities May be as effective as LMWH Per the American College of Chest Physicians (ACCP), chemoprophylaxis superior to mechanical alone Combined IPC and chemoprophylaxis superior to either alone Core Curriculum V5
Prevention Mechanical Prophylaxis Compressive Stockings Minimize venous stasis Multiple RCTs to suggest decreased incidence of DVT/PE Core Curriculum V5
Prevention Inferior Vena Cava Filter In theory prevents migration of DVT to the pulmonary artery Mixed evidence regarding efficacy Numerous complications if left long term ACCP recommends against use of IVC filters in polytrauma patients Core Curriculum V5
Prevention Chemoprophylaxis Unfractionated Heparin (UFH) Binds to antithrombin III inactivates thrombin, factor Xa Half life of 1-2 hours (dosed 2-3 times daily) Reversible with protamine Heparin Induced Thrombocytopenia (HIT) a potential complication Core Curriculum V5
Prevention Chemoprophylaxis Low-Molecular-Weight Heparin (LMWH) Also binds antithrombin III, but reduced anti-factor IIa activity Half life of 4-5 hours (dosed once or twice daily) Lab monitoring not required Superior to UFH in terms of PE risk reduction Concerns over wound drainage/bleeding complications HIT still possible, but lower risk compared to UFH Core Curriculum V5
Prevention Chemoprophylaxis Fondiparinux Indirect factor Xa inhibitor Half life of 17 hours (once daily administration) No risk of HIT Superior reduction of VTE compared to LMWH in hip fracture patients Core Curriculum V5
Prevention Chemoprophylaxis Aspirin Irreversible inhibitor of cyclooxygenase (COX) Inhibits platelet aggregation for 8-9 days Arthroplasty literature shows decreased VTE and fewer complications compared to other agents Not well studied in the trauma population Core Curriculum V5
Prevention Chemoprophylaxis Novel Oral Anticoagulants (NOACs) Dabigatran: selective inhibition of thrombin Rivaroxaban, Apixaban, Edoxaban: inhibit factor Xa Half life of 5-15 hours Efficacy not well studied in trauma population Concerns include bioavailability of oral agents in hospitalized patients, bleeding complications, limited reversibility Core Curriculum V5
24 Item questionnaire to members of OTA Found wide variability in surgeon practices Many practices not evidence based Expert panel constructed evidence-based guidelines Core Curriculum V5
Other Risk Factors 1. Older than 40 years 2. Obesity (body mass index > 30) 3. Previous history of VTE (personal or familial) 4. History of malignancy 5. History of smoking 6. Hormonal birth control 7. Nonambulatory status 8. Spinal cord injury 9. Proximity of injury to the axial skeleton 10. Tourniquet use 11. Immobilization 12. Other hypercoagulability conditions (protein C and S deficiency) Core Curriculum V5
265 patients with below-knee fractures Randomized to 14 days of LMWH vs placebo Doppler of bilateral proximal leg veins at 14 days and 3 months Overall incidence of clinically important VTE (CIVTE) was 1.9% no significant difference between groups Due to low incidence of CIVTE, trial recruitment was stopped early Core Curriculum V5
Metanalysis of 5 randomized trials describing chemoprophylaxis of VTE after operative management of fractures of the tibia and distal bones Assessed the incidence of any VTE vs clinically important VTE (CIVTE) Incidence of any VTE was significantly reduced with chemoprophylaxis No significant difference in CIVTE between LMWH and placebo Core Curriculum V5
Review of 11,313 trauma patients treated from 2010-2017 in a large multicenter health care system database Captured patients with ORIF of pelvis/acetabulum, femoral neck, and intertrochanteric fractures or intramedullary nailing (IMN) of the femur or tibia All patients in the study were on chemical and mechanical prophylaxis LMWH or Warfarin Overall rate of VTE was 0.82% (0.39% DVT, 0.43% PE) Pelvis/acetabulum 1.7% Femoral IMN 1.33% Core Curriculum V5
Diagnosis of DVT Symptoms Clinically silent in many cases Limb swelling Homan s sign (calf pain with passive dorsiflexion of the ankle) Tachycardia Fever of unknown origin Core Curriculum V5
Diagnosis of DVT Wells Score 3-8 points = High probability 1-2 points= moderate probability -2-0 points= low probability Ahsan ZS, Firoozibadi R. 2020. Venous Thromboembolic Disease in Patients with Skeletal Trauma. Tornetta, Paul, III, Rockwood and Green s Fractures in Adults 9e, Wolters Kluwer, 2020 Core Curriculum V5
Diagnosis of DVT Testing modalities D-Dimer Poor specificity Venography Historical Venous Doppler Exam Good sensitivity/specificity, but user dependent MRI Expensive, high false positive rate Core Curriculum V5
Diagnosis of PE Symptoms Tachycardia Shortness of breath Chest pain Hypoxia Hemoptysis Cyanosis Core Curriculum V5
Diagnosis of PE Wells Score > 6 points = High probability 2-6 points= moderate probability < 2 points= low probability Ahsan ZS, Firoozibadi R. 2020. Venous Thromboembolic Disease in Patients with Skeletal Trauma. Tornetta, Paul, III, Rockwood and Green s Fractures in Adults 9e, Wolters Kluwer, 2020 Core Curriculum V5
Diagnosis of PE Testing modalities Ventilation/Perfusion (V/Q) Scan Historical gold standard Remains useful for patients with contrast allergies or renal impairment CT Pulmonary Angiography (CTPA) Good sensitivity/specificity Current gold standard Core Curriculum V5
Treatment of DVT Based on anatomic location and individual risk factors Proximal to calf aggressive treatment Typically 3 months of anticoagulation (sometimes indefinite) Novel oral anticoagulants preferred to warfarin or LMWH Serial imaging of deep veins in patients at high risk of bleeding No anticoagulation for stable thrombus Core Curriculum V5
Treatment of PE Subsegmental (proximal pulmonary artery not involved) Rarely associated with cardiopulmonary complications Low incidence of concomitant DVT or recurrent thromboemboli Clinical surveillance recommended if no proximal DVT Clinically Relevant PE Respiratory and hemodynamic support as needed Thrombolytic therapy if low risk of bleeding If elevated bleeding risk thrombus removal Core Curriculum V5
Summary DVT/PE are common in patients with skeletal trauma Combined mechanical and chemical prophylaxis is recommended LMWH is commonly used in the trauma population IVC filters should be reserved for high risk patients with contraindications to an acceptable anticoagulant Core Curriculum V5
Key References Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315 352. Sagi HC, Ahn J, Ciesla D, et al. Venous Thromboembolism Prophylaxis in Orthopaedic Trauma Patients: A Survey of OTA Member Practice Patterns and OTA Expert Panel Recommendations [published correction appears in J Orthop Trauma. 2016 Jan;30(1):e35. Tornetta, Paul 3rd [added]]. J Orthop Trauma. 2015;29(10) Ahsan ZS, Firoozibadi R. 2020. Venous thromboembolic disease in patient s with skeletal trauma. Tornetta, Paul, III, Rockwood and Green s Fractures in Adults 9e, Wolters Kluwer, 2020 Core Curriculum V5