Understanding Crystalarthropathies and Gout: A Comprehensive Overview
Crystalarthropathies encompass a group of diseases characterized by hyperuricemia and uric acid crystal formation, leading to conditions like gouty arthritis and nephrolithiasis. Primary gout, characterized by hyperuricemia without an identifiable underlying cause, primarily affects older men. Mechanisms of hyperuricemia in primary gout involve underexcretion or overproduction of uric acid. Deficiencies in HGP.T can also result in hyperuricemia, with complete deficiency leading to the Lesch-Nyhan syndrome. Diagnosis involves assessing HGP.T activity in erythrocytes.
Uploaded on Sep 17, 2024 | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Crystalarthropathies Gout
it is a group of diseases characterized by hyperuricaemia and uric acid crystal formation. These clinical syndromes include gouty arthritis, tophaceous gout, uric acid nephrolithiasis, and gouty nephropathy. In its more narrow and perhaps more commonly used definition, gout refers to arthritis caused by uric acid crystals. Risk factors for primary gout Male gender Age >40 years Obesity Family history Alcohol use Renal insufficiency Hypertension
Mechanisms of hyperuricaemia in primary gout Primary gout is simply defined by the absence of any identifiable underlying disease causing hyperuricaemia. This criterion defines the largest group of patients with gout. Most of these patients are older men and 80 85 per cent are hyperuricaemic on the basis of underexcretion of uric acid. There is no difference in rates of intestinal uricolysis in patients with primary gout compared with controls. Thus, the site of the abnormality in patients with primary gout who underexcrete is most likely to be at the kidney.
most patients with primary gout have low fractional uric acid excretion rates. The mechanism of underexcretion remains to be elucidated but is most likely a defect in secretion or reabsorption rather than in filtration. A minority of patients with primary gout have high urinary uric acid levels and excessive de novo purine synthesis. The best evidence to date supports a role for increased PRPP availability or decreased purine nucleotide concentrations (thus diminishing feedback inhibition of the synthetic enzymes) in patients with primary gout who overproduce uric acid
H G PT deficiency produces hyperuricaemia by increasing de novo synthesis of purine nucleotides through increased availability of the substrate PRPP, which stimulates synthesis . In its most complete form, HGP T deficiency results in the Lesch Nyhan syndrome. This syndrome presents in early childhood with severe mental retardation, self- mutilation, choreoathetosis, spasticity, hyperuricaemia, and premature gout. Although it is linked to the X chromosome, there are two reported cases in girls .
Partial defects of HGP T result in hyperuricaemia alone without the severe neurological consequences of complete HGP T deficiency. The diagnosis of HGP T deficiency can be made by documenting low HGP T activity in erythrocytes. Numerous different genetic mutations have been described in HGP T deficiency
Mechanism through wich MSU crystal cause inflamation
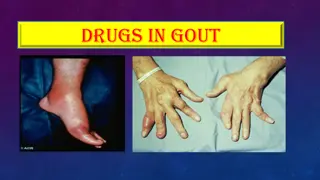
Clinical features Articular gout is often divided into four clinical stages. The first stage is defined by asymptomatic hyperuricaemia. This is followed by acute gouty arthritis and then by another asymptomatic phase termed intercritical gout. When allowed to proceed untreated, some patients will go on to develop chronic tophaceous gout. Acute gout The first clinical symptom of gout is usually an acute, self- limited, monoarticular inflammatory arthritis affecting the joints of the lower extremities. Gout has a predilection for the first metatarsophalangeal joint(Podagra). As many as 50 70 per cent of first gout attacks occur in the big toe. Other frequently involved joints include those of the foot, ankle, knee, wrist, elbow, and the small joints of the hands. The large axial joints and those of the spine are uncommon sites for early acute gout attacks.
The onset of an attack occurs suddenly and often late at night or early in the morning. Patients will describe very severe pain, associated with swelling, extreme tenderness, and redness overlying the joint. Without intervention, the attack will usually subside within 5 7 days. Low-grade fever, malaise, and anorexia may occur. The attack may be preceded by brief twinges of pain (petit attacks) in the affected joint. Common precipitants of acute attacks include excess alcohol intake, intercurrent illness, surgery, starvation, trauma, and the initiation of drugs that alter urate metabolism. All of these precipitants alter serum urate levels.
Physical examination shows signs of inflammation with erythema, warmth, and swelling over the joint, often extending to the overlying skin. There is exquisite tenderness over the affected joint. Not infrequently, an overlying cellulitis or accompanying tenosynovitis occurs. The skin may desquamate in the later days of an attack. Acute gout can also occur in bursas, and gout is a common cause of acute inflammatory olecranon bursitis. After the attack resolves, the patient will be completely asymptomatic. This phase is referred to as intercritical gout. Most patients will go on to have an additional attack within 2 years of the first attack.
In one study, 78 per cent had recurrent attacks within 2 years, and after 10 years, 93 per cent had had more than one attack . Untreated, the intercritical phases become shorter. Interestingly, they still present an opportunity for diagnosis, as many joints will still have urate crystals in the synovial fluid during the intercritical phase if they were involved in a previous attack, and urate-lowering therapy has not been initiated
Chronic tophaceous gout In the later stages of untreated disease, clinical manifestations characteristically change. Acute attacks are more often polyarticular. The intercritical stage shortens, and repeated joint damage results in permanent deformities, loss of motion, chronic pain, and tophi. Polyarticular gout occurs in late-stage disease, although some patients present earlier with polyarticular attacks. Intercritical stages are short or non-existent and involvement of atypical sites including the upper extremities, the spine, and axial joints may ensue. After repeated attacks in a single joint, deformity and loss of motion may occur.
Tophi are deposits of urate embedded in a matrix composed of amorphous urates, lipids, proteins, and calcific debris . Tophi are usually subcutaneous, but they rarely occur in bone and other organs including the heart valves and the eye. Classic sites include the pinna of the ear, bursas around elbows and knees, the dorsal surfaces of the metacarpophalangeal joints, and the Achilles tendon. Tophi are not distinguishable on physical examination from rheumatoid nodules or other subcutaneous nodules. There is no accompanying inflammation and they are usually painless. The overlying skin may be taut and shiny. A thick white or whitish-yellow exudate is seen if the skin integrity is compromised.
Tophi or chronic polyarthritis may occur as early as 3 years or as late as 42 years after the first acute attack. In the pre-treatment era, 50 per cent of patients with gout had tophi after 10 years of disease . Currently, about 5 per cent of patients with gout will have tophi . Their occurrence is directly correlated with serum urate levels, and they identify a group of patients with severe and prolonged hyperuricaemia. Another group at risk of developing tophi and polyarticular gout are elderly women with primary nodal osteoarthritis on diuretic therapy
Urate nephropathy The pathological changes that define urate nephropathy are common. MSU crystals in the renal medulla are associated with a giant-cell inflammatory reaction. The clinical significance of these pathological findings, however, remains unclear. Renal insufficiency is unequivocally common in patients with gout, but controversy exists as to the aetiology of this renal dysfunction. Current dogma states that urate crystals themselves produce only a minor amount of renal damage.
Most of the renal disease associated with gout is secondary to inadequately controlled hypertension, non-steroidal anti-inflammatory drug (NSAID) use, and other comorbidities Uric acid nephrolithiasis the risk factor is high serum urate &low urin PH.
Laboratory investigation Synovial fluid analysis remains the single most important diagnostic study in the patient with suspected gout. Synovial fluid is usually easily obtained from a large joint, while often only a drop of fluid or blood from the joint or adjacent tissues is necessary to provide a sample for definitive diagnosis of gout in a small joint. Synovial fluid is typically inflammatory with a mean white cell count of 20 000 cells/mm 3 . Most cells are polymorphonuclear leucocytes. Viscosity is often poor. A definite diagnosis can be made if typical, negatively birefringent, needle-shaped crystals are seen in the fluid with a polarizing light microscope . They may be extra- or intracellular. Rarely one may see spherules of uric acid in acute gout.
Few other laboratory studies are of significant clinical utility in diagnosing acute gout. Serum uric acid levels during the acute attack may not reflect pre-attack levels and cannot be used to make a diagnosis of gout in the absence of urate crystals in the synovial fluid. One may see a peripheral leucocytosis, an elevated erythrocyte sedimentation rate, and increased levels of other acute-phase reactants during an acute attack. Synovial fluid cultures and Gram stains may help rule out concurrent infection. Radiographs are often normal during early episodes of gout. They may be useful to differentiate other problems such as fracture or infection from acute gout. Often, soft tissue swelling is the sole radiographic finding in early gout.
Diagnosis definitive diagnosis of gout can only be made by the identification of urate crystals in the synovial fluid of an affected joint. Identification of urate crystals in tophi also allows a definitive diagnosis to be made. In the absence of these findings, other clinical criteria may be used to make a putative diagnosis of gout As crystals may be present in the intercritical phase, one may aspirate an asymptomatic but previously affected joint to establish a definite diagnosis. Many clinical conditions can mimic acute gout These include infectious arthritis, other crystal-associated arthropathies such as pseudogout or BCP-associated periarthritis, or trauma.
Patients with palindromic rheumatism may give a similar history of self-limited monoarticular attacks associated with exquisite pain, tenderness, and erythema near the affected joint. Rarely, other causes of polyarticular inflammatory arthritis, particularly psoriatic arthritis or Reiter's syndrome, may present with monoarticular self-limited attacks of the lower extremities that may be confused with gout. Once tophi and deformities occur, gout can be misdiagnosed as rheumatoid arthritis. As many as 30 per cent of patients with gout will have positive serum rheumatoid factors .
Clinical conditions that mimic gouty arthritis CPPD disease (pseudogout) *Psoriatic arthritis BCP arthritis *Rheumatoid arthritis Cellulitis Erythema nodosum arthritis Trauma Palindromic rheumatism Reiter's syndrome
Management of gouty arthritis divided into three phases: treatment of acute gout, treatment of chronic or tophaceous gout, and preventive measures Management of acute gout Traditional therapies for acute gout include NSAIDs, colchicine, and steroids. Rest and splinting of the affected joint may be helpful adjuncts to any pharmacological therapy. Colchicine Colchicine tends to be much more effective in the early hours of an attack and loses efficacy with time. The mechanism of action of colchicine is unknown. It inhibits polymorphonuclear leucocyte function through its action on microtubules, but may also have very specific effects on crystal-induced inflammation .Colchicine can be given in intravenous and oral forms.
A dose of 13 mg diluted in 20 ml of normal saline can be slowly instilled into a large vein. Another 1-mg dose can be given 6 h later if the clinical response is incomplete. The maximum dose is 4 mg in 24 h. No additional doses should be given for 7 days after the initial dose. Intravenous colchicine is particularly useful for patients unable to take oral medications. Now that parenteral forms of NSAIDs are available, its use may decline further. Absolute contraindications to the use of intravenous colchicine include significant renal or hepatic compromise, bone marrow suppression, or sepsis. It should be used with great caution in patients with mild renal or hepatic disease, or those on daily oral colchicine prophylaxis.
Side-effects range from venous sclerosis or tissue damage from extravasation of colchicine, to fatal bone marrow failure. Other side-effects include renal or hepatic failure, disseminated intravascular coagulation, and neuromuscular toxicity. Deaths from misuse of intravenous colchicine have been reported Corticosteroids Regimens for acute gout include intramuscular ACTH, intramuscular triamcinolone, and oral steroids . These regimens are safe and well tolerated. Their efficacy remains to be proven. They may be particularly useful for patients in whom NSAIDs and colchicine are contraindicated. The use of intra-articular steroids is less controversial. Although no studies of the efficacy of intra-articular steroids have been published, they remain a mainstay of therapy in patients unable to tolerate more traditional therapies.
Allopurinol Allopurinol is the drug most commonly used for the prevention of acute gout and the treatment of chronic tophaceous gout .It is a xanthine oxidase inhibitor and thus decreases uric acid production. It may also have other actions . It is very effective in lowering serum uric acid levels and is the drug of choice for patients with renal insufficiency, a history of nephrolithiasis, or tophi. It is also indicated in patients who clearly overproduce uric acid such as those with tumour lysis syndrome or primary metabolic defects. Allopurinol is usually given as a once daily dose of 300 mg.
The most common side-effects include a hypersensitivity syndrome of rash and fever. Life- threatening reactions, including fulminant hepatitis, interstitial nephritis, and toxic epidermal necrolysis, are even more unusual. Patients with renal disease may have a greater incidence of drug allergy. Allopurinol can be given cautiously to an allergic patient using available desensitization regimens .
Uricosurics Probenecid and sulfinpyrazone are the most commonly used uricosuric drugs. They interfere with the renal handling of urate by altering organic anion transport, thus increasing urate excretion. Uricosurics are contraindicated in patients with nephrolithiasis and ineffective in patients with significant renal compromise, or those using acetylsalicylates. Side- effects include rare hypersensitivity reactions, rashes, gastrointestinal complaints, and nephrotic syndrome. Benzbromarone is a uricosuric drug available in Europe. Unlike other commonly used uricosuric drugs, it is effective in patients with renal insufficiency
Less potent uricosuric agents include the angiotensin 1 receptor antagonist losartan, and the lipid-lowering agents atorvastatin and fenofibrate. New urate lowering agent as Febuxostat, which inhibits xanthine oxidase through a different mechanism than allopurinol and oxypurinol, blocks substrate access to xanthine oxidase by occupying a channel in the enzyme leading to the active site.
Gout & food