Understanding Skeletal Muscle Relaxants and Muscle Contraction Mechanisms
Skeletal muscle relaxants play a crucial role in relaxing muscles without affecting consciousness significantly. They are classified into neuromuscular blockers and spasmolytics, each targeting different mechanisms in the body. Muscle contraction occurs through the release of acetylcholine and the subsequent interaction of troponin and tropomyosin. Competitive non-depolarizing neuromuscular blockers act as antagonists at nicotinic receptors, inhibiting the wave of depolarization and muscle contraction. Understanding these processes is essential for the effective use of muscle relaxants in clinical settings.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Skeletal Muscle Relaxants Skeletal Muscle relaxants relax skeletal muscles without affecting the level of consciousness to a significant level. Two major types Neuromuscular blockers act on neuromuscular junction and are used to relax muscles during surgical procedures. Spasmolytics act on CNS or directly on muscles; used to reduce spasticity in neurological disorders.
Skeletal Muscle relaxants Neuromuscular blockers Spasmolytics D tubocurarine Pancuronium Vecuronium Atracurium Succinylcholine Centrally acting Baclofen Benzodiazepine Tizanidine Directly acting Botulinum toxin Dantrolene
Differences between Centrally Acting Spasmolytics and Neuromuscular blockers Centrally acting spasmolytics Neuromuscular blockers Action Reduces muscle tone; Voluntary power is not loss Muscle paralysis; Voluntary power is loss Mechanism Inhibit polysynatic reflexes in CNS Inhibit NM transmission at NM junction CNS depression Yes No Route of administration Therapeutic indications Oral or parenteral Parenteral Chronic spastic conditions Short term surgical procedures
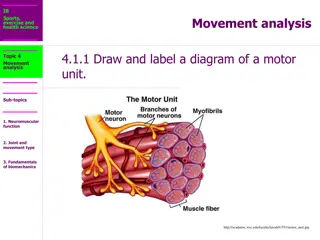
How the muscle contracts? With the arrival of impulse at the motor nerve terminal, acetylcholine is released, which activates NM receptor. It opens the gate of sodium ion channels that increases the entry of sodium leading to depolarization and spread to entire muscle fiber. It triggers the release of calcium from sarcoplasmic reticulum, which binds with troponin to break the troponin-tropomycin complex. The inhibition of the troponin-tropomycin complex on actin myosin interaction is inhibited so they get free to interact resulting into muscle contraction. Acetylcholine is rapidly destroyed by choline esterase and repolarization takes place. Repolarized muscle is now capable of responding to a fresh nerve stimulus.
Competitive or non-depolarizing neuromuscular blockers Mechanism of Action Non-depolarizing blockers are competitive antagonist at nicotinic NM receptor, therefore block the NM receptor and prevent acetylcholine to produce a wave of depolarization. They prevent postsynaptic membrane to depolarize hence also known as stabilizing agents. The block is surmountable type i.e. can be overcome by increasing the dose of agonist. Therefore anticholinesterase and electrical stimulation of nerve (that increases concentration of acetylcholine) inhibits the action.
Pharmacological actions On skeletal muscles: Paralysis; small muscles with rapid movements like those of fingers, toes, jaws, and eyes are affected first so there is difficulty in speech, ptosis, diplopia and dysphagia. Thereafter muscles of limbs, neck and trunk and lastly the intercostal muscles and diaphragm are affected. Reversal occurs in reverse order. Autonomic ganglion partial block leading to hypotension and tachycardia. Histamine release leads to bronchospasm, hypotension, and excessive bronchial and salivary secretions. CVS- hypotension due to vasodilatation because of release of histamine, sympathetic ganglion blockade and decrease venous return due to loss of skeletal muscle tone. CNS- they do not cross BBB hence no direct effect. However the breakdown product of atracurium, laudosine can cross blood brain barrier to produce seizures.
Adverse effects Non-depolarizing neuromuscular blockers can produce apnea, respiratory failure, cardiovascular collapse and effects of histamine release such as bronchospasm, hypotension, and excessive bronchial and salivary secretions. Treatment of respiratory failure is by positive pressure artificial respiration, oxygen, and neostigmine. NM blockers (except atracurium) need reversal by neostigmine with glycopyrollate. Suggamadex is a rapid reversal by chelating steroidal neuromuscular blocker and thereby inactivating them.
Drug interactions Drugs that enhance the neuromuscular blocking effect Inhalational anesthetics like ether, halothane, isoflurane and enflurane, stabilize the membrane so synergistic. Antimicrobials: Aminoglycosides by decreasing acetylcholine release, tetracyclines by chelating calcium; polymyxin B, clindamycin, vancomycin and colistin by NM blocking effect. Antiarrhythmics: Quinidine and procainamide owing to neuromuscular blockade. Local anesthetics: Lignocaine, procaine by stabilizing the membrane; procaine also competes with succinylcholine for the enzyme pseudocholinesterase. Calcium channel blockers enhance effect of competitive neuromuscular blocker. Magnesium- by reducing release and sensitivity of acetylcholine. Misc.- morphine, pethidine chloroquine, digitalis, propranolol
Drugs that inhibit the neuromuscular blocking effect Anticholinesterase, by reducing the metabolism of acetylcholine, antagonizes the effect. Calcium salts by increasing the release of acetylcholine. Corticosteroids, if patient is receiving for a long period, antagonize effect of certain NMB. Competitive NMB antagonizes depolarizing blockers.
Classification of Non-depolarizing neuromuscular blockers (a) According to duration of action- Long acting- d tubocurarine, pancuronium, metocurine, doxacurium, pipecuronium Intermediate vecuronium, atracurium, cis- atracurium, rocuronium Short acting mivacurium Ultra short acting gantacurium ( action last for 5-10 minutes only)
Some thing special Long acting ones are more potent so need low concentrations; hence the onset of action is delayed. Rocuronium is having intermediate duration but rapid onset therefore used as an alternative to succinylcholine for rapid sequence intubation in patients where succinylcholine is contraindicated. Rocuronium is painful on injection, which can be reduced by alkalizing the solution.
According to chemical characteristics Natural alkaloids and synthetic substitute: D tubocurarine, gallamine, and metocurine. They are potent histamine liberator. Ammonio steroid: Pancuronium; no histamine release but blocks muscarinic receptors so tachycardia. With newer agents like vecuronium and rocuronium there s no tachycardia. Benzylisoquinolines: Atracurium, mivacurium; no anticholinergic and no ganglionic blockade but a little tendency to release histamine. Safe in renal insufficiency since the elimination follows a different pattern. Mivacurium is hydrolyzed by plasma cholinesterase; Atracurium is having two routes of degradation, one is by plasma cholinesterase and other is by Hofmann degradation . Hofmann degradation breaks down the atracurium to laudosine, which has no parental activity but crosses BBB to produce seizures. Cisatracurium forms less laudosine, hence claimed to have less potential for seizures.
Depolarizing Blockers: Succinylcholine Succinylcholine is having two acetylcholine molecules linked end to end. It produces depolarization in a manner similar to acetylcholine but is not so rapidly metabolized hence the effect persists for a long period. Persistent depolarization occurs without repolarization so muscle is non responsive to a new impulse and paralysis occurs. Excitation contraction coupling requires repolarization and repeated firing to maintain muscle tension so flaccid paralysis results. This is depolarizing phase 1 block that is potentiated by anticholinesterase.
Depolarizing Blockers: Succinylcholine With continuation of the exposure or in higher doses, the initial depolarization decreases, membrane is repolarized but still refractory to acetylcholine as long as succinylcholine is present ( Non-depolarizing Phase II block). The mechanism is not clear; probably a non-excitable area develops surrounding the motor end plate, which prevents the centrifugal spread of impulses initiated by acetylcholine (desensitization) This is why excessive dose of succinylcholine can also lead to prolonged apnea even with normal status of pseudocholinesterase. This phase II block is similar to block produced by non-depolarizing blockers hence can be reversed by anticholinesterases.
Kinetics & Genetics After a single intravenous dose of 10-30 mg effect of succinylcholine starts with in a minute, reach to peak in 2 minutes and last for 5 minutes. This brief effect is due to its rapid hydrolysis by pseudocholinesterase present in plasma and liver. There is prolonged effect if the level of enzyme is low as observed in malnutrition, uremia, liver disease, occupational exposure to anticholinesterase and abnormal genetic variants. In the last case there are atypical pseudo cholinesterases, which are not able to metabolize succinylcholine leading to prolonged paralysis and apnea (succinyl apnea).
Adverse effects: P5 enhancement Potassium (Hyperkalemia) due to prolonged depolarization Pressures (Increase intra ocular pressure, gastric , vomiting , aspiration) Pain (muscle soreness, twitching)- due to damage produced by the twitching of muscles. Paralysis (Succinyl apnea) Pyrexia (Malignant hyperthermia ) if used with halothane or isoflurane, in patients with hereditary disorder and familiar tendency, there is a sudden release of calcium with massive contraction of muscles, lactic acid production, acidosis, and increase body temperature. It may be fatal. It is managed by rapid cooling, control of acidosis, 100% oxygen inhalation and dantrolene.
Contraindications to succinylcholine Patients with extensive soft tissue injury such as burn, trauma and peritoneal infections Rhabdomyolysis i.e. dissolution and disintegration of skeletal muscles. Ocular lacerations Spinal cord injury with paraplegia or quadriplegia or with muscle dystrophies Child below age of 8 years (NM junction is not fully developed) Renal failure (hyperkalemia becomes life threatening)
Therapeutic indications for neuromuscular blockers As a part of balance anesthesia to get muscle relaxation that facilitate operative manipulation and endotracheal intubation. Orthopedic procedures like correction of dislocation and alignment of fractures. To facilitate endotracheal intubations, laryngoscopy, bronchoscopy and esophagoscopy. To prevent trauma in ECT. To control convulsions in tetanus, status epilepticus, and drug toxicity. To facilitate artificial ventilation in patients of obstructive airway diseases by reducing chest wall resistance.
Spasmolytics Spasm is sustained involuntary muscle contraction accompanied by pain and stiffness or tightness of the muscles . There is increased muscle tone and reduced muscle power with overactive reflexes. There may be clonus i.e a series of fast involuntary contractions. Spasticity is the outcome of an imbalance of signals from the CNS to the muscles. This imbalance is often found in people with cerebral palsy, traumatic brain injury, stroke, multiple sclerosis, and spinal cord injury. A variety of conditions like trauma, inflammation, pain and anxiety may also associated with acute muscle spasm.
Spasticity can be reduced by Stretching exercises: Prolonged stretching makes the muscle longer, reduces the spasticity and prevents the contracture. Splinting, casting, and bracing: These methods are used to maintain range of motion and flexibility. Antispastic drugs helping by: Central effects leading to modification of the stretch reflex arc : Benzodiazepines, baclofen, Tizanidine, Mephensin. Peripheral , by interfering directly with skeletal muscles: Dantrolene, Botulinum toxin
CENTRALLY ACTING DRUGS Benzodiazepines like diazepam and clonazepam facilitate the effect of GABA Baclofen- GABAB agonist inhibits monosynaptic and polysynaptic transmission in spinal cord. It is less sedative. Tizanidine: Central 2 agonist inhibiting release of excitatory neurotransmitter from spinal neurons. The adverse effects are drowsiness, dizziness, asthenia and dry mouth. Mephensin depresses transmission through spinal and supraspinal polysynaptic pathways. It produces mild sedation. There may be hypotension and respiratory paralysis. Several other drugs are also used to manage the acute muscle spasm such as methocarbamal, chlorzoxazone, carisoprodol, orphenadrine, chlormezanone, chlorphenesin, cyclobenzaprine, tolperisone, Thiocolchicoside,etc.
Directly acting drugs Dantrolene in the skeletal muscles, it inhibits the release of Ca from sarcoplasmic reticulum and thereby produces muscle relaxation. During excitation-contraction coupling, there is direct coupling between the receptor of T-tubule with ryanodine receptor (RYR) of sarcoplasmic reticulum leading to release of calcium. Calcium sensitivity of RYR is increased by caffeine and reduced by dantrolene. Adverse effects are sedation, diarrhea, generalized muscle weakness and hepatitis. Indications: Malignant hyperthermia, neuroleptic malignant syndrome and spastic disorders.
Botulinum toxin It is a powerful neurotoxin protein obtained from Clostridium botulinum. It blocks acetylcholine release, by degrading synaptobrevin that is required for synaptic vesicle fusion with the axon terminal membrane, and thereby produces flaccid paralysis of skeletal muscles. The effect may loss for 3-4 months. It is being used in management of Blephrospasm i.e. Spasm of eyelids Strabismus (squint, abnormal alignment of the eyes). Achalasia cardia: failure of the lower oesophageal sphincter to relax Anal fissures Hyperhidrosis of palm and axilla: Excessive sweating due to excess of acetylcholine. Cosmetic surgery to get wrinkle free face Spastic disorders such as cerebral palsy, torticollis Prophylaxis of migraine Urinary incontinence due to over active bladder Sialorrhoea (Hypersalivation , if refractory to glycopyrollate.
Botulinum toxin Different botulium toxins used as therapeutics are: Incobotulinumtoxin A, Onabotulinumtoxina, Abobotulinumtoxina, Rimabotulinumtoxin b. Adverse effects may be pain at site of injection, dyspepsia, dysphagia, muscle weakness, ptosis, neck pain and fever. Occasionally there may be arrhythmia, syncope, hepatotoxicity and anaphylaxis.
One minute perception Shortest acting: Succinyl choline/Gentacurium, mivacurium Fastest acting: Succinyl choline/ Gentacurium , rocuronium Rocuronium is used as an alternative to succinylcholine for rapid sequence intubation Longest acting: Doxacurium pan, tube, metro all are long acting Miva- short Curonium-ammoniosteroid- no histamine release but anticholinergic Curium- benzyl isoquinolines- no anticholinergic, no ganglionic blocking but histamine release. Muscle relaxants with no/minimal CVS side effects are: Vecuronium(Safest), Doxacurium & rocuronium
Preferred Muscle Relaxant In Hepatic failure: Atracurium In Renal failure: Atracurium In arterial surgery (to maintain arterial pressure): Pancuronium For rapid sequence intubation (the emergency means for the fastest airway control) Succinyl choline or Rocuronium Tetanus toxin inhibits GABA release leads to spastic paralysis (unopposed excitatory influence) Botulinum toxin inhibits acetylcholine release, contractility is loss, so flaccid paralysis