Overview of Chemical Mediators of Inflammation and Their Roles
Chemical mediators of inflammation act on blood vessels and cells to contribute to an inflammatory response. These mediators include vasoactive amines like histamine and serotonin, plasma proteases such as the complement, kinin, and clotting systems, and important inflammatory mediators like C3a and C5a. Activation pathways and systems like the kinin system play key roles in promoting vasodilation, increased vascular permeability, smooth muscle contraction, and pain. Understanding these mediators is crucial in managing inflammatory conditions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
CHEMICAL MEDIATORS OF INFLAMMATION Dr. SANJIV KUMAR ASSTT. PROFESSOR, DEPTT. OF PATHOLOGY, BVC, PATNA
Definition: Any messenger that acts on blood vessels, inflammatory cells, or other cells to contribute to an inflammatory response. May be in present in Cell or Plasma In Cell they are either preformed or newly synthesized In plasma present as precursor or inactive form.
VASOACTIVE AMINES Histamine and Serotonin (Histamine is formed from amino acid histidine by histidine decarboxylase ) Increase Vascular Permeability and Vascular Permeability Mediators in the immediate active phase of increased permeability Promotes contraction of smooth muscle *Serotonin found in rodent mast cells
PLASMA PROTEASES 1. COMPLEMENT SYSTEM 2. KININ SYSTEM 3. CLOTTING SYSTEM
Activation Pathway Classical pathway- By antibody, antigen complex Alternate pathway- By microbial surface polysaccharides Common pathway
Important inflammatory mediators C3a and C5a (anaphylatoxins) Cause release of histamine from mast cells Lysosomal enzyme release in inflammatory cells C5a Activates lipoxygenase pathway Chemotactic many inflammatory cells Increases adhesion of leukocytes C5b-9 membrane attack complex (MAC) Lyses cells Stimulates arachidonic acid metabolism Produces reactive oxygen metabolites C3b act as opsonin
KININ SYSTEM Activated by Hageman factor (XIIa) BRADYKININ (Vasoactive nanopeptide) I. Potent vasodilator II. Increased vascular permeability III.Contraction of smooth muscle IV.Produce pain V. Stimulates release of histamine VI.Activates the arachidonic acid cascade
COAGULATION SYSTEM Clotting system/fibrinolytic system Plasma proteins Can be activated by Hageman factor Thrombin converts fibrinogen to fibrin vascular permeability Chemotactic for leucocytes Plasmin is important in lysing fibrin clots, Activates Hageman factor (XII) bradykinin Cleaves C3 C3a "fibrin-split products" formed from fibrin breakdown vascular permeability
HAGEMAN FACTOR Factor XII of intrinsic coagulation cascade Causes Coagulation Activation of fibrinolytic system Produces bradykinin Activates complement Provides an amplification system
ARACHIDONIC ACID METABOLITES 20-carbon polyunsaturated fatty acid (4 double bonds) Derived directly from dietary sources or by conversion of essential fatty acid linoleic acid Undergo 2 major pathways Cyclooxygenase pathway (COX) Lipoxygenase pathway (LOX)
CYCLOOXYGENASE PATHWAY 3 important products Thromboxane A2 Aggregates platelets and causes vasoconstriction Prostacyclin (PGI2) Endothelial cells inhibits platelet aggregation and causes vasodilation Prostaglandins PGE2, PGF2-alpha and PGD2 Variety of actions on vascular tone and permeability Pain and fever
LIPOXYGENASE PATHWAY Leukotrienes and lipoxins Leukotriene B4 is a potent chemotactic agent Leukotrienes C4, D4, E4 Potent vasoconstrictors Potent mediators of increased vascular permeability on venules only Up to 1000 times as potent as histamine in producing increased vascular permeability Lipoxins cause vasodilation, inhibit neutrophil i.e. reverse of leukotrienes.
PLATELET ACTIVATING FACTOR from mast cells, neutrophils, macrophages, platelets, endothelium etc. as AA metabolites Aggregate platelets and cause release Bronchoconstriction and Vasoconstriction At low concentration Vasodilation and vascular permeability leukocyte adhesion Leukocyte chemotaxis
CYTOKINES Transmitters for cell-to-cell chatting Primarily from activated macrophages and lymphocytes
IL-I and TNF Master Cytokines
Other Cytokines IL-5 Eosinophils IL-6 B and T cells IL-8 Neutrophils Lesser degree monocytes and eosinophils
GROWTH FACTORS Platelet derived growth factor Transforming growth factor Chemokines Important in regeneration and repair
NITRIC OXIDE (NO) Formed from arginine along with citrulline 3 effects Physical mediator of vascular tone Host defense Reduces platelet aggregation and adhesion Inhibits several features of mast cell induced inflammation Uncontrolled NO production Can lead to massive peripheral Vasodilation and Shock
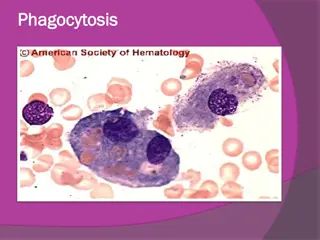
LYSOSOMAL CONSTITUENTS Neutrophils, Monocyte/Macrophages Smaller, specific or secondary granules like lysozyme, collagenase, histminase. Large, azurophil or primary granules like myeloperoxidase, acid hydrolases, elastase etc. Cationic proteins vascular permeability Chemotactic Neutral proteases degrade ECM while acid proteases degrade bacteria, neutral proteases cause anaphylotoxins.
OXYGEN-DERIVED FREE RADICALS Cause endothelial damage Protein destruction by inhibiting antiproteases Injury to variety of cells Don t forget the antioxidants Ceruloplasmin Transferrin Superoxide dismutase Catalase Glutathione peroxidase