Understanding Gastrointestinal System Disorders and Endoscopy Procedures
Gastrointestinal (GI) tract disorders are common and can affect various parts of the digestive system. The GI system plays a vital role in ingestion, nutrient absorption, and waste elimination. Endoscopy is a non-surgical procedure used to diagnose and treat GI issues by visualizing the digestive tract with a flexible tube. Therapeutic endoscopy is also utilized for treatments like stone removal and stricture dilation. This article provides insights into GI disorders and the importance of endoscopy procedures.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Care of patients with Gastrointestinal system disorders
Outline ; Endoscopy. Proctoscopy . Nasogatric tube. medications; *Ranitidine * Metoclopramide * Dolcolax
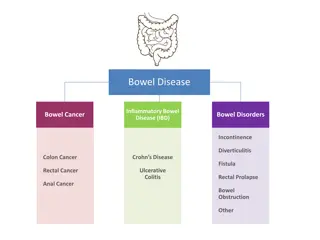
Gastrointestinal system disorders Gastrointestinal (GI) tract disorders are disorders of the digestive tract, which is sometimes called the Digestive diseases . The GI system comprises the alimentary canal and its accessory organs, beginning at the mouth; extending through the pharynx, esophagus, stomach, small intestine, colon, rectum, and anal canal; and ending at the anus.
The GI system is responsible for the following essential bodily functions: ingestion , absorption of nutrients into the bloodstream, and elimination of waste products from the body . Some common problems include ; Gastroesophageal reflux disease (GERD), peptic ulcer disease. Rectal problems, such as hemorrhoids. Liver problems, such as hepatitis B or hepatitis C, liver failure. Pancreatitis Tests for digestive problems can include Proctoscopy, upper GI endoscopy, cholangiopancreatography .
Endoscopy procedure Endoscopy is a nonsurgical procedure used to examine a person's digestive tract. Endoscopy is the use of a flexible tube with a light and camera attached to it, to visualize the GI tract and to perform certain diagnostic and therapeutic procedures. Images of digestive tract are produced through a video screen monitor. The endoscope can be inserted through the rectum or mouth, depending on which portion of the GI tract is to be viewed
During an upper endoscopy, an endoscope endoscope is lubricated with a water-soluble lubricant and passed smoothly and slowly along the back of the mouth and down into the esophagus allowing the doctor to view the esophagus, stomach, and upper part of the small intestine. Endoscopes contain multipurpose channels that allow for air insufflations, irrigation, fluid aspiration, and the passage of special instruments.
Therapeutic endoscopy can be used to remove common bile duct stones, dilate strictures, and treat gastric bleeding and esophageal varices. The patient wears a mouth guard to keep from biting the scope.
Capsule Endoscopy Capsule endoscopy utilizes an ingestible camera device rather than an endoscope. The procedure involves swallowing a capsule (camera device), which passes through the digestive system while taking pictures of the intestine. capsule (About the size of a large vitamin capsule) that takes multiple digital photos of the small bowel. The images are transmitted via small sensors attached to the abdomen with adhesive stickers or transmitted wirelessly from the capsule to recording device belted to the patient's waist.
Capsule Endoscopy The small bowel is about 6 meters long and the capsule takes about 8 hours to travel through it After approximately 8 hours, the recording device is removed, the physician downloads image data from the recorder to a PC and views the images to make a diagnosis. No sedation or anesthetic is required. The capsule will be excreted naturally through the digestive tract.
Indications Dysphagia. Esophageal reflux symptoms that persist or recur despite appropriate therapy. Persistent vomiting of unknown cause. For confirmation and specific histologic diagnosis of radiologically demonstrated lesions In patients with active GI bleeding or recent bleeding. When sampling of tissue or fluid is indicated. Treatment of bleeding lesions such as ulcers, tumors, Removal of foreign bodies. Placement of feeding or drainage tubes (eg, percutaneous endoscopic gastrostomy).
Contraindications Acute MI Peritonitis Acute perforation Patients who are taking anticoagulants
Complications Cardiopulmonary complications related to sedation and analgesia are the most common types of complications seen with diagnostic endoscopy . Aspiration pneumonia ( Aspiration of gastric contents into the lungs is common, pneumonia and may result in death). Infectious complications related to diagnostic endoscopy result either from the procedure itself or from the use of contaminated equipment. Perforation. Bleeding can result from injury to gastric or abdominal wall vessels.
Nursing interventions Before the procedure 1) Explain the following to the patient: 1) The type of procedure to be performed on the patient, And advise that someone must accompany the patient to drive home due to the patient being sedated. 2) NPO for 8 to 12 hours before the procedure to prevent aspiration and allow for complete visualization of the stomach. 3) Remove dentures and partial plates to facilitate passing the scope and preventing injury. 4) Inform the health care provider of any known allergies and current medications. Medications may be held until after the test is completed.
Describe what will occur during and after the procedure to the patient : 1) The throat will be anesthetized with a spray or gargle. 2) An I.V. sedative will be administered. 3) The patient will be positioned on the left side with a towel or basin at the mouth to catch secretions and to provide easy access for the endoscope. 4) A plastic mouthpiece will be used to help relax the jaw and protect the endoscope. Emphasize that this will not interfere with breathing.
5) The patient may be asked to swallow once while the endoscope is being advanced. Then the patient should not swallow, talk, or move tongue. Secretions should drain from the side of the mouth, and the mouth may be suctioned. 6) Air is inserted during the procedure to permit better visualization of the GI tract. Most of the air is removed at the end of the procedure. The patient may feel bloated, burp, or pass flatus from remaining air.
After the procedure 1) The nurse instructs the patient not to eat or drink until the gag reflex returns (in 1 to 2 hours), to prevent aspiration of food or fluids into the lungs. 2) The nurse assess or test gag reflex by placing a tongue blade onto the back of the throat to see whether gagging occurs. 3) After the patient s gag reflex has returned, the nurse can offer saline gargle, and oral analgesics to relieve minor throat discomfort. 4) The nurse places the patient in the Simms position until he or she is awake and then places the patient in the semi-Fowler s position until ready for discharge.
5) observing for signs of perforation, such as pain, bleeding, unusual difficulty swallowing, and an elevated temperature. 6) Patients who were sedated for the procedure must stay on bed rest until fully alert. 7) he nurse monitors the pulse and blood pressure for changes that can occur with sedation. 8) The nurse instructs the patient not to drive for 10 to 12 hours if sedation was used.
Proctoscopy The lower portion of the colon also can be viewed directly to evaluate rectal bleeding, acute or chronic diarrhea, or change in bowel patterns and to observe for ulceration, fissures, abscesses, tumors, polyps, or other pathologic processes. Proctoscopy is a diagnostic procedure used to examine anal cavity, rectum or sigmoid colon (pelvic colon) through an instrument called proctoscope. Proctoscope is a metal or plastic tube which is approximately 8 inch in diameter. The procedure is usually done to examine hameorrhoids or rectal polyps (overgrown tissues).
Procedure for proctoscopy During the procedure the instrument is lubricated and is inserted into the rectum and air is gently pumped in which allows a clearer view of the interior part of the rectum. The complete procedure takes around 5-10 minutes. This procedure is usually uncomfortable
Indications: 1) To confirm radiographic findings. 2) To obtain biopsy, cytology and culture specimens. 3) To locate and coagulate bleeding points. 4) To examine hameorrhoids Contraindications: 1) Patients with a large aortic aneurysm. 2) Patients with acute myocardial infarction. 3) Patients with abnormal coagulation studies.
Complications that may arise after proctoscopy Bleeding . Difficulty in urinating. Sever pain
Nursing interventions These examinations require only limited bowel preparation, including use an enema or laxative to empty the colon before the test is done. During the procedure, the nurse monitors vital signs, skin color and temperature, pain tolerance.
After the procedure, 1) the nurse monitors the patient for rectal bleeding and signs of intestinal perforation (ie, fever, rectal drainage, abdominal distention, and pain). 2) On completion of the examination, the patient can resume regular activities and dietary practices.
Nasogastric tube (NGT) (NGT )refers to the insertion of a tube through the nasopharynx into the stomach. Purposes of Nasogastric Intubation 1) Prevent or relieve nausea and vomiting after surgery or traumatic events by decompressing the stomach. 2) Irrigate the stomach (lavage) for active bleeding or poisoning. 3) Administer medications and feeding (gavage) directly into the GI tract. 4) Obtain a specimen of gastric contents
Procedure 1) Gather equipment. 2) Don non-sterile gloves 3) Explain the procedure to the patient and show equipment 4) If possible, sit patient upright for optimal neck/stomach alignment 5) Examine nostrils for deformity/obstructions to determine best side for insertion 6) Measure tubing from bridge of nose to earlobe, then to the point halfway between the end of the sternum and the navel 7) Lubricate 2-4 inches of tube with lubricant. Pass tube via nostrils, past the pharynx into the esophagus and then the stomach.
Procedure 8) Instruct the patient to swallowing or sips small of water to enhance passage of tube into esophagus. If resistance is met, rotate tube slowly with downward advancement toward closes ear. Do not force. 9) Check for placement by attaching syringe to free end of the tube, aspirate sample of gastric contents. Do not inject an air bolus, as the best practice is to test the pH of the aspirated contents to ensure that the contents are acidic. The pH should be below 6. Obtain an x-ray to verify placement before instilling any feedings/medications or if you have concerns about the placement of the tube. 10) Secure tube with tape or commercially prepared tube holder. 11) Document the reason for the tube insertion, type & size of tube, the nature and amount of aspirate, the type of suction and pressure setting if for suction, the nature and amount of drainage, and the effectiveness of the intervention.
Nursing interventions 1) Assure the patient that most discomfort he feels will lessen as he gets used to the tube. 2) Irrigate the tube at regular intervals (every 2 hours unless otherwise indicated) with small volumes of prescribed fluid (To ensure the tube patency) . 3) Ensure that NGT in correct position through , inject air or aspirate stomach secretion. 4) Cleanse nares and provide mouth care every shift.
Nursing interventions 5) Apply petroleum jelly to nostrils as needed, and assess for skin irritation or breakdown. 6) Keep head of bed elevated at least 30 degrees. 7) Record the time, type, and size of tube inserted. Document placement checks after each assessment, along with amount, color, consistency of drainage.
Ranitidine Classification: Action: Histamine inhibiting basal gastric acid secretion and gastric acid secretion that is stimulated by food, insulin, histamine, cholinergic agonists, gastrin, duodenal ulcer gastric ulcer Short-term treatment of gastroesophageal reflux disease (GERD) esophagitis Treatment of heartburn. allergy to ranitidine, lactation. impaired renal or hepatic function, pregnancy. Indications contraindication Side Effects: CNS: Headache, malaise, dizziness. CV: Tachycardia, bradycardia. Dermatologic: Rash, alopecia GI: Constipation, diarrhea, nausea, vomiting. Local: Pain at IM site, local burning or itching at IV site
Ranitidine Nursing Considerations: Administer oral drug with meals and at bedtime. Decrease doses in renal and liver failure. Administer IM dose undiluted, deep into large muscle group. Arrange for regular follow-up, including blood tests, to evaluate effect . Patient teaching Take drug with meals and at bedtime. Have regular medical follow-up care to evaluate your response. These side effects may occur: Constipation or diarrhea (request aid from your health care provider) nausea, vomiting (take drug with meals) headache (adjust lights and temperature and avoid noise). Report fever, unusual bruising or bleeding, severe headache, muscle or joint pain.
Metoclopramide Classification: Antiemetic increases lower esophageal sphincter pressure; , accelerates gastric emptying and intestinal transit. Action: Prevention of nausea and vomiting associated with emetogenic cancer chemotherapy Prophylaxis of postoperative nausea and vomiting when nasogastric suction is undesirable Indications Contraindicated with allergy to metoclopramide GI hemorrhage contraindications Side Effects: CNS: Restlessness, drowsiness, fatigue, anxiety CV: Transient hypertension GI: Nausea, diarrhea Nursing Considerations: Monitor BP carefully during IV administration. Monitor diabetic patients, arrange for alteration in insulin dose or Have phentolamine readily available in case of hypertensive crisis.
Dulcolax Classification: laxative It acts directly on the bowels, stimulating the bowel muscles (Perstalsis) to cause a bowel movement and evacuate the colon . Action: to treat constipation Indications allergic to any ingredient in Dulcolax. severe stomach pain; appendicitis. stomach, intestinal, or rectal bleeding. contraindications abdominal cramping, diarrhea, nausea, vomiting fluid and electrolyte imbalance. Side Effects: Assess for allergy to the drug, stomach pain, N/V, sudden change in bowel habits lasting >2 weeks. Monitor for rectal bleeding, for no bowel movement, stomach discomfort. Monitor fluid and electrolyte regularly . Nursing Considerations: