Understanding Eating Disorders in Children by Dr. Soumi Kundu
Eating disorders in children, such as anorexia nervosa, bulimia nervosa, and binge eating disorder, are complex biopsychosocial disorders characterized by dysfunctional patterns of cognition and weight control behaviors. They result in significant physical, psychological, and social complications. These disorders have been on the rise in India over the last two decades, impacting older children and adolescents. The classification in DSM-5 includes specific diagnoses like ARFID and umbrella diagnoses like OSFED and UFED, highlighting the importance of early identification, intervention, and treatment to address these challenging issues.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
EATING DISORDERS IN EATING DISORDERS IN CHILDREN CHILDREN DR. SOUMI KUNDU Assistant Professor Department of Pediatrics KPCMCH, Kolkata
Common Eating Problems in Children Common Eating Problems in Children Food refusal Inappropriate food for age Poor appetite Picky eaters Faulty feeding practices These can be easily treated with parents education, few feeding modifications. But Eating Disorders on the other hand are much more difficult to treat.
EATING DISORDERs EATING DISORDERs
Eating disorders (EDs) are complex biopsychosocial disorders characterized by dysfunctional patterns of cognition and weight control behaviors that result in significant physical, psychological and social complications. Affects older children and adolescents. Incidence is increasing in India over the last two decades.
ED ED FED FED Eating Disorders (ED) this term has been replaced with Feeding and Eating Disorders (FED) in the 5th revision of the American Psychiatric Association s Diagnostic and Statistical Manual of Mental Disorders (DSM-5) published in 2013 and in the 11th revision of the World Health Organisation s International Statistical Classification of Diseases (ICD-11) and Related Health Problems published in 2019. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th edn) (DSM-5). Washington, DC: American Psychiatric Association; 2013. World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 11th Revision(ICD-11). Geneva: World Health Organization; 2019.
CLASSIFICATION CLASSIFICATION In DSM-5, FED comprises of eight diagnoses Six specific diagnoses : 1. Anorexia Nervosa (AN) 2. Bulimia Nervosa (BN) 3. Binge Eating Disorder (BED) 4. Avoidant/Restrictive Food Intake Disorder (ARFID) 5. Pica and 6. Rumination Disorder (RD) Two umbrella diagnoses : Other Specified Feeding or Eating Disorder (OSFED) and Unspecified Feeding or Eating Disorder (UFED) 1. 2.
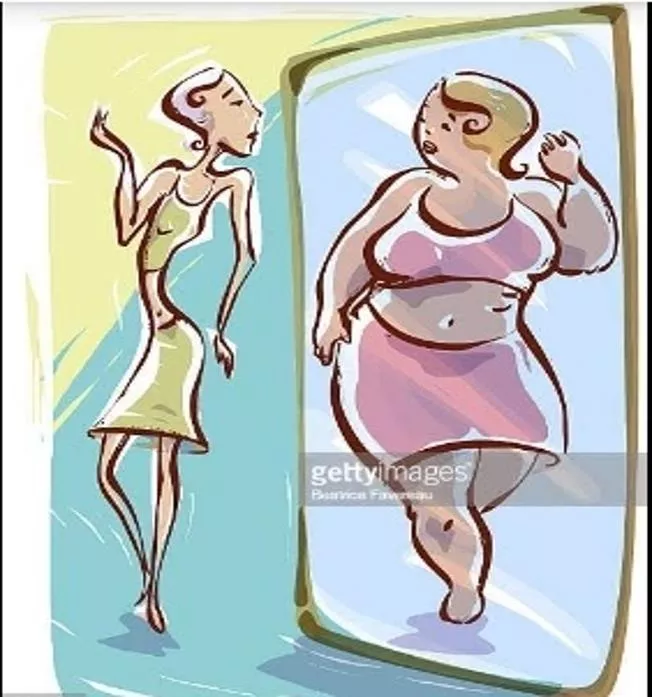
ANOREXIA NERVOSA ANOREXIA NERVOSA Restriction of energy intake relative to requirements, leading to a significantly low body weight in the context of age, sex, developmental trajectory, and physical health. Significantly low weight is defined as a weight that is less than minimally normal or, for children and adolescents, less than minimally expected. Intense fear of gaining weight or of becoming fat, or persistent behaviour that interferes with weight gain, even though at a significantly low weight.
Disturbance in the way in which one s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or persistent lack of recognition of the seriousness of the current low body weight. Two types Restricting type: During the last three months, the individual has not engaged in recurrent episodes of binge eating or purging behaviour (i.e. self-induced vomiting, or the misuse of laxatives, diuretics, or enemas). This subtype describes presentations in which weight loss is accomplished primarily through dieting, fasting and/or excessive exercise. Binge-eating/purging type: During the last three months the individual has engaged in recurrent episodes of binge eating or purging behaviour (i.e. self- induced vomiting, or the misuse of laxatives, diuretics, or enemas). Severity: Mild: BMI more than 17 Moderate: BMI 16- 16.99 Severe: BMI 15-15.99 Extreme: BMI less than 15
CLINICAL FINDINGs CLINICAL FINDINGs Weight loss; Loss of muscle, subcutaneous fat Weakness, fatigue Hypothermia; Acrocyanosis Pedal edema Dry skin, brittle nail Lanugo-type hairs, increased loss of scalp hair Dizziness, fainting, palpitations Bradycardia; Hypotension, orthostatic pulse difference >25 beats/min.; Increased risk of heart failure Early abdominal fullness, digestive problems, constipation Osteoporosis Severe dehydration, which may lead to renal failure Irregular menstruation, amenorrhea AN may be associated with other psychiatric disorders, like depression, OCD (Obsessive-Compulsive disorder), phobias, panic disorder, mood disorder, various personality disorder.
LABORATORY FINDINGs LABORATORY FINDINGs Hemoglobin, WBC, Platelet Hypoglycemia K, Na, Ca, Mg, Phosphorus (Refeeding syndrome) Metabolic alkalosis (in vomiting) or acidosis (laxative use) LFT, cholesterol Hypoproteinemia Normal or ESR Hypercarotenemia LH, FSH, estrogen Normal TSH, fT4, T3 (Sick Euthyroid syndrome) Bone density ECG Sinus bradycardia, low voltage graphs, prolonged QT interval, flat or inverted T wave, depressed ST segment
BULIMIA NERVOSA BULIMIA NERVOSA Recurrent episodes of binge eating. An episode of binge eating is characterized by both: 1. Eating in a discrete period of time (e.g. within any 2 hour period), an amount of food that is definitely larger than what most individuals would eat in a similar period of time under similar circumstances; 2. A sense of lack of control over eating during the episodes (e.g. a feeling that one cannot stop eating or control what or how much one is eating). Recurrent inappropriate compensatory behaviors to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise. The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for 3 months.
Self-evaluation is unduly influenced by body shape and weight. The disturbance does not occur exclusively during episodes of anorexia nervosa. Severity: Mild: An average of 1-3 episodes of inappropriate compensatory behaviours per week. Moderate: An average of 4-7 episodes of inappropriate compensatory behaviours per week. Severe: An average of 8-13 episodes of inappropriate compensatory behaviours per week. Extreme: An average of 14 or more episodes of inappropriate compensatory behaviours per week. Episodic binge eating usually occur in secret; may be triggered by stress, isolation or negative emotions. Tend to binge on foods high in sugar and refined flour. More likely to binge alone. Aware of fat and calories, but less regimented in avoidance than AN.
CLINICAL FINDINGs CLINICAL FINDINGs Thin to overweight Russell s sign Subconjunctival hemorrhage Dental enamel erosion, perimolysis Esophagitis; Mallory-Weiss tears Hematemesis Enlarged salivary glands (parotid > submandibular) Absent gag reflex Menstrual irregularities Laxative dependent : rectal prolapse, melena, cathartic colon May be associated with depression, substance abuse, h/o PTSD; more likely suicidal than AN LABORATORY FINDINGs LABORATORY FINDINGs Serum amylase Electrolyte abnormalities due to diarrhea from heavy laxative use K, Hypochloremic metabolic alkalosis from frequent purging ECG - Arrhythmia
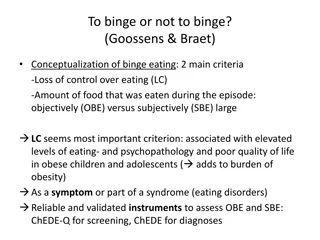
BINGE EATING DISORDER BINGE EATING DISORDER Recurrent episodes of binge eating. An episode of binge eating is characterized by both: 1. Eating in a discrete period of time (e.g. within any 2 hour period), an amount of food that is definitely larger than what most individuals would eat in a similar period of time under similar circumstances; 2. A sense of lack of control over eating during the episodes (e.g. a feeling that one cannot stop eating or control what or how much one is eating). Binge eating episodes are associated with three or more of the following: 1. Eating much more rapidly than normal. 2. Eating until feeling uncomfortably full. 3. Eating large amounts of food when not feeling physically hungry. 4. Eating alone because of feeling embarrassed by how much one is eating. 5. Feeling disgusted with oneself, depressed, or very guilty afterwards.
Marked distress regarding binge eating is present. The binge eating occurs, on average, at least once a week for 3 months. The binge eating is not associated with the recurrent use of inappropriate compensatory behavior as in bulimia nervosa and does not occur exclusively during the course of bulimia nervosa or anorexia nervosa. Severity: Mild: 1-3 binge eating episodes per week. Moderate: 4-7 binge eating episodes per week. Severe: 8-13 binge eating episodes per week. Extreme: 14 or more binge eating episodes per week.
AVOIDANT/ RESTRICTIVE FOOD INTAKE AVOIDANT/ RESTRICTIVE FOOD INTAKE DISORDER DISORDER A feeding or eating disturbance (e.g. lack of apparent interest in eating food; avoidance based on the sensory characteristics of food; concern about aversive consequences of eating) as manifested by persistent failure to meet appropriate nutritional and/or energy needs associated with one (or more) of the following: 1. Significant weight loss (or failure to achieve expected weight gain or faltering growth in children). 2. Significant nutritional deficiency. 3. Dependence on enteral feeding or oral nutritional supplements. 4. Marked interference with psychosocial functioning. The disturbance is not better explained by lack of available food or by an associated culturally sanctioned practice.
The eating disturbance does not occur exclusively during the course of anorexia nervosa or bulimia nervosa, and there is no evidence of a disturbance in the way in which one s body weight or shape is experienced. The eating disturbance is not attributable to a concurrent medical condition or not better explained by another mental disorder. When the eating disturbance occurs in the context of another condition or disorder, the severity of the eating disturbance exceeds that routinely associated with the condition or disorder and warrants additional clinical attention. Presents as 3 subtypes 1. Low interest or limited intake 3. Fear or aversive 2. Sensory or limited variety
PICA PICA Persistent eating of non-nutritive, non-food substances (e.g., paper, paint, plaster, soap, clay, wool, ashes, earth etc.) over the period of at least 1 month. The eating of non-nutritive, non-food substances is inappropriate to the developmental level of the individual. The eating behaviour is not part of a culturally supported or socially normative practice. If the eating behaviour occurs in the context of another mental disorder (e.g.,intellectual disability, autism spectrum disorder) or medical condition (e.g.,pregnancy), it is sufficiently severe to warrant additional clinical attention. Onset can occur in childhood. Pica can occur in otherwise normally developing children. It is the only FED which can be diagnosed simultaneously with other ED. Treatment Combined behavioral, social and medical approaches. Specific treatment for the ingested items, e.g., Lead toxicity, Iron-deficiency anemia, Parasitic infestation, Surgical intervention for gastric bezoar from ingestion of hair etc.
RUMINATION DISORDER RUMINATION DISORDER Repeated regurgitation of food over the period of at least 1 month. Regurgitated food may be re-chewed, re-swallowed, or spit out. Not attributable to an associated gastrointestinal or other medical condition (e.g., reflux). Does not occur exclusively during the course of anorexia nervosa, bulimia nervosa, binge-eating disorder, or avoidant/restrictive food intake disorder. If symptoms occur in the context of another mental disorder (e.g., intellectual disability), they are sufficiently severe to warrant additional clinical attention. Rumination is poorly understood but believed to be self-stimulatory. Weight loss, failure to reach expected weight, malnutrition may occur. Behavioral treatment by reinforcing correct eating behavior while minimizing attention to rumination. Aversive conditioning techniques are more useful in adolescents.
OTHER SPECIFIED FEEDING OR EATING DISORDER Symptoms characteristic of a feeding or eating disorder that cause clinical distress or impairment in social, occupational, or other important areas of functioning predominate. However DO NOT meet the full criteria for any of the disorders in the feeding and eating disorders diagnostic class. This category can also be used in situations to communicate the specific reason the presentation does not meet the criteria for a specific eating disorder. This is done by recording other specified feeding or eating disorder followed by the specific reason e.g. bulimia nervosa- low frequency .
UNSPECIFIED FEEDING OR EATING DISORDER Symptoms characteristic of a feeding and eating disorder & cause clinical significant distress or impairment in social, occupational or other important areas of functioning predominate. However DO NOT meet the full criteria for any of the disorders in the feeding and eating disorders diagnostic class. Used when the clinician chooses not to specify the reason that criteria are not met for a specific feeding and eating disorder. This includes times when there is insufficient information to make a more specific diagnosis (e.g. in emergency room setting).
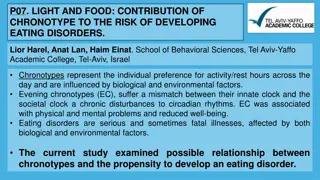
ETIOLOGY AND PATHOGENESIS ETIOLOGY AND PATHOGENESIS Multidimensional Genetic/ Biological Factors Both AN and BN tend to run in families. - Serotonin may play a role in BN - Dopamine in restrained eating Psychological Factors Low self-esteem/ Poor body image - Overvaluation of appearance - Inadequate coping machanisms - Feeling of failure/ feeling out of control - Response to change (puberty); stress (sports, dance) Social/ Cultural Factors Social norms for obtaining the perfect body - Peer pressure - Social media hype of thin body image Interpersonal Factors Unresolved family conflicts - Body relevant insult and teasing - History of physical or sexual abuse
RISK FACTORs FOR FED RISK FACTORs FOR FED A family history of FED, substance use or mood disorder Poor communication and conflict resolution at home Low self-esteem and self-confidence Personality traits such as perfectionism Family values or cultural norms about having a specific body size Participation in sports that focus on body shape and size such as ballet dancing, gymnastics, track events etc. Early puberty Abusive relations that cause emotional distress and feeling of loss of control such as physical or sexual abuse
EVALUATION EVALUATION Thorough history/ interview There are different questionnaire, like - Eating Disorder Inventory (EDI) - Eating Disorder Examination Interview (EDE) - Eating Attitudes Test (EAT) - SSHADES Specific signs and symptoms as discussed previously Specific laboratory investigations In another type of assessment, individuals with AN are shown line drawings of persons with varying body weight and asked to pick the closest one.
SAMPLE SCREENING QUESTIONs FOR SAMPLE SCREENING QUESTIONs FOR SUSPECTED FED SUSPECTED FED Why do you think that you are losing weight? How long has this been going on? What is your highest and lowest weight? What is your usual diet? Do you eat breakfast, lunch and dinner? Do you skip meals? Have you changed your intake? Is there anything that you do not eat or feel guilty eating? Have you ever tried to restrict your intake or consumed large quantities of food at one time? Have you tried to vomit, use laxatives or other diet pills? Do you exercise regularly? How much at one time? When was your last menstrual history and how often do you have your menses? Have you felt sad, depressed, suicidal or anxious? Are you on social media? If so, what do you use and how often? Are any of your peers dieting or concerned about their weight? When you look in the mirror what do you see? Are there certain parts of your body that you are unhappy with? How would you feel if you gained weight? Have you had any dizziness, weakness, fatigue or difficulty focusing? Have you noticed any cold intolerance or irregular menses? Do you have dry skin and/ or Lanugo (fine hair)? Have you had any bloating, heartburn, abdominal pain, constipation, diarrhea, chest pain, joint pains or muscle cramps? Abraham A. Eating Disorders in Adolescents. Indian J Adolescent Medicine. 2019;1(2):11-14.
DIFFERENTIAL DIAGNOSIS DIFFERENTIAL DIAGNOSIS Malignancy, CNS tumors Endocrinopathies, e.g. Hyperthyroidism Occult chronic infection Malabsorption, e.g. Inflammatory bowel disease, celiac disease Stimulant abuse Type 1 diabetes mellitus Addison disease Depression Obsessive-compulsive disorder
COMPLICATIONs COMPLICATIONs Cardiac complications Ventricular dysrhythmias, reduced myocardial contractility Nutritional deficiencies Refeeding syndrome Suicidal tendency, depression, anxiety Hypothalamic dysfunction Reduced gonadal function Osteoporosis Hypertension, Diabetes mellitus, gall-bladder disease (associated with BED )
TREATMENT TREATMENT Multidisciplinary care Inpatient or outpatient treatment Nutrition Physical activity Cognitive Behavioral Therapy(CBT) Family Based Therapy(FBT) Dialectical Behavioral Therapy(DBT) Interpersonal Psychotherapy(ITP) Drug therapy Selective Serotonin Reuptake Inhibitors(SSRI), Tricyclic antidepressants(TCA), Serotonin Norepinephrine Reuptake Inhibitor(SNRI), Anticonvulsants Alternate therapies Yoga, mindfulness
TREATMENT OF AN TREATMENT OF AN Treatment of AN comprises of a specific program involving three main phases Weight restoration Treatment of psychological disturbances Long term remission. Outpatient care In mild to moderate cases. CBT and FBT (Maudsley approach) DBT Used in binge-purge subtype Individual psychodynamic (not effective) Inpatient care Prognosis depends on duration of illness, age and type of treatment. Antidepressants, Antipsychotics not much effective Use of zinc, cyproheptadine Hormone therapy - controversial However, patients are five times more likely to die prematurely and at much higher risk for suicide than non-eating disorder patients which underscores the need for early screening and treatment. Fichter M, Quadflieg N. Mortality in eating disorders results of a large prospective clinical longitudinal study. International J of Eating Disorders. 2016.https://doi.org/10.1186/s40337-016-0130-2.
TREATMENT OF BN TREATMENT OF BN Outpatient care Break the binge-purge cycle intensive counseling and regular follow-up. CBT most effective. FBT also useful. SSRIs TCA - binge, improve mood. Antiepileptic drug (topiramate) Inpatient care - Nutritional rehabilitation, replenishing electrolytes, preventing further medical or psychiatric complications. If untreated, BN may lead to long-term complications, e.g. Arrhythmia, dental problems, bleeding from esophagus. Mortality less common than AN. Poor prognosis if associated with sexual abuse, depression or substance abuse.
TREATMENT OF BED TREATMENT OF BED CBT (CBT+Orlistat > CBT) DBT and group therapy SSRI binge freqency TCA binge frequency, weight and depression Antieileptics (topiramate and zonisamide), SNRI, Atomoxetine - binge frequency, weight TREATMENT OF ARFID TREATMENT OF ARFID CBT Structure meal time Exposure therapy Helps to tolerate anxiety-provoking foods or the physical process of consuming the feared food or neophobia. FBT Nutritional rehabilitation Volume before variety . Supplementation of specific vitamins or minerals Cyproheptadine in low-weight patients Lorazepam, Olanzapine more trials needed.
PREVENTION PREVENTION Prevention is difficult Target older adolescents and college-age- women Psychoeducational approaches De-emphasizing socio-cultural influences Risk factor identification and intervention to alter these factors
TAKE HOME MESSAGE FEDs are potentially life threatening Cause considerable psychological distress apart from the physical complications Early diagnosis and treatment are of paramount importance More awareness is needed in our society Social media can play a vital role