Pediatric Respiratory Conditions Management Overview
Tuberculosis is a contagious respiratory disease affecting children, with drug therapy involving a 6-month course and nursing management focusing on supportive care and treatment adherence. Prevention strategies include isolation, nutrition, and vaccination. Epistaxis, or nosebleeds, are common in children and can be managed by applying pressure, encouraging mouth breathing, and using cold compresses.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
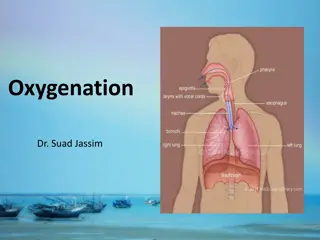
The child with Respiratory Alteration The child with Respiratory Alteration Lecture 4
TUBERCULOSIS Tuberculosis is a highly contagious disease caused by inhalation of droplets of Mycobacterium tuberculosis or Mycobacterium bovis. Annually about 1,000 U.S. children contract active tuberculosis disease. Non white children and children with chronic illness or malnutrition are more susceptible to infection. the incubation period is 2 to 10 weeks.
Drug Therapy the American Academy of Pediatrics recommends: a 6-month course of oral therapy. The first two months consist of isoniazid, rifampin, and pyrazinamide given daily. This is followed by twice-weekly isoniazid and rifampin. Ethambutol or streptomycin is given via intramuscular injection
Nursing Management Hospitalization of children with tuberculosis is necessary only for the most serious cases. Nursing management is aimed at providing supportive care and encouraging adherence to the treatment regimen. Supportive care includes ensuring adequate nutrition and adequate rest, providing comfort measures such as fever reduction, preventing exposure to other infectious diseases, and preventing reinfection.
Preventing Infection Tuberculosis infection is prevented by avoiding contact with the tubercle bacillus. hospitalized children with tuberculosis must be isolated according to hospital policy to prevent nosocomial spread of tuberculosis infection. Promotion of natural resistance through nutrition, rest, and avoidance of serious infections does not prevent infection. Pasteurization of milk has helped to decrease the transmission of Mycobacterium bovis. Administration of bacille Calmette-Gu rin (BCG) vaccine can provide incomplete protection against tuberculosis
EPISTAXIS Epistaxis (a nosebleed) occurs most frequently in children younger than adolescent age. Bleeding of the nasal mucosa occurs most often from the anterior portion of the septum. Epistaxis may be recurrent and idiopathic 6
Nursing Management The child should sit up and lean forward (lying down may allow aspiration of the blood). Apply continuous pressure to the anterior portion of the nose by pinching it closed. Encourage the child to breathe through the mouth during this portion of the treatment. Ice or a cold cloth applied to the bridge of the nose may also be helpful. The bleeding usually stops within 10 to 15 minutes. Apply petroleum jelly or water-soluble gel to the nasal mucosa with a cotton-tipped applicator to moisten the mucosa and prevent recurrence. 7
RESPIRATORY DISTRESS SYNDROME (RDS) It results from lung immaturity and a deficiency in surfactant, so it is seen most often in premature infants. Diabetic mothers, cesarean section deliveries without preceding labor, and those experiencing perinatal asphyxia. It is believed that each of these conditions has an impact on surfactant production 8
Other Names for Respiratory Distress Syndrome Hyaline membrane disease Neonatal respiratory distress syndrome Infant respiratory distress syndrome Surfactant deficiency 9
The administration of surfactant via endotracheal tube shortly after delivery helps to decrease the incidence and severity of RDS. Management of RDS focuses on intensive respiratory care, usually with mechanical ventilation. 10
Signs and Symptoms of Respiratory Distress Syndrome Rapid, shallow breathing Sharp pulling in of the chest below and between the ribs with each breath Grunting sounds Flaring of the nostrils 11
Complications 1. Air leak syndrome (pneumothorax) . 2. Bronchopulmonary dysplasia(atelectasis). 3. Patent ductus arteriosus. 4. congestive heart failure 5. Intraventricular hemorrhage, 6. Retinopathy of prematurity. 7. Necrotizing enterocolitis. 8. Complications resulting from intravenous catheter use (infection, thrombus formation), and developmental delay or disability 12
Diagnostic test Chest x ray. A chest x ray creates a picture of the structures inside the chest, such as the heart and lungs. Blood tests. Blood tests are used to see whether an infant has enough oxygen in his or her blood. Echocardiography (echo). This test uses sound waves to create a moving picture of the heart. 13
Treatments Surfactant replacement therapy. Breathing support from a ventilator or nasal continuous positive airway pressure (NCPAP) machine. Oxygen therapy. 14
Prevention Seeing your doctor regularly during your pregnancy Following a healthy diet Avoiding tobacco smoke, alcohol, and illegal drugs Managing any medical conditions you have Preventing infections 15
Nursing Management Nursing care of the child with RDS is mainly supportive and occurs in the intensive care unit. Closely monitor respiratory and cardiovascular status. Comfort measures such as hygiene and positioning as well as pain and anxiety management. Maintenance of nutrition, and prevention of infection are also key nursing interventions. Psychological support of the family as well as education 16
ASTHMA Asthma is a chronic inflammatory airway disorder characterized by airway hyper responsiveness, airway edema, and mucus production. Airway obstruction resulting from asthma might be partially or completely reversed 17
ASTHMA 18
Symptoms of Asthma 1. Wheezing 2. Coughing: Cough may be the only symptom of asthma, especially in cases of exercise-induced or nocturnal asthma. 3. Chest tightness: The child may feel like the chest is tight or won't expand when breathing in. 4. Other symptoms: Infants or young children may have a history of cough or lung infections (bronchitis) or pneumonia 19
Causes of Asthma 1. Respiratory infections: These are usually viral infections. In some patients, other infections with fungi, bacteria, or parasites might be responsible. 2. Allergens: An allergen is anything in a child's environment that causes an allergic reaction. Allergens can be foods, fungi, or dust mites. 3. Irritants: Tobacco smoke, cold air, chemicals, perfumes, paint odors. 4. Weather changes. 5. Emotional factors. 6. Gastroesophageal reflux disease (GERD). 20
The Five Parts to an Asthma Treatment Plan Step 1: Identifying and controlling asthma triggers Step 2: Anticipating and preventing asthma flares. Step 3: Taking medications as prescribed. Step 4: Controlling flares by following the doctor's written step-by-step plan. Step 5: Learning more about asthma, new medications, and treatments. 21
Laboratory and diagnostic studies Pulse oximetry: oxygen saturation may be significantly decreased or normal during a mild exacerbation Chest x-ray: usually reveals hyperinflation Blood gases: might show carbon dioxide retention and hypoxemia Pulmonary function tests (PFTs): can be very useful in determining the degree of disease. Allergy testing: skin test or RAST can determine allergic triggers for the asthmatic child 22
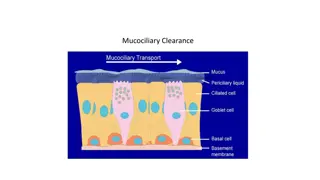
Tracheostomy A tracheostomy is an artificial opening in the airway, usually a plastic tracheostomy tube is in place to form a patent airway. Thetracheostomy facilitates secretion removal, reduces work of breathing, and increases patient comfort. In some cases the tracheostomy facilitates mechanical ventilation weaning. 23
It may be permanent or temporary depending on the condition that leads to the tracheostomy. 24
Complications Hemorrhage, air entry, pulmonary edema and respiratory arrest. tube occluded and ventilation compromised. Complications of chronic tracheostomy include infection, cellulitis, and formation of granulation tissue around the insertion site. 25
Nursing Management In the immediate postoperative period the infant or child may require restraints to avoid accidental dislodgment of the tracheostomy tube. Provide humidity to either room air or oxygen. Tracheostomies require frequent suctioning to maintain patency. Perform tracheostomy care every 8 hours or per institution protocol. 26