Insights into Vertebral Fractures and Bone Health
Delve into the world of vertebral fractures and bone health with Dr. Frazer Anderson. Explore the impact of fractures, the importance of understanding the spine, and how to treat and prevent fractures effectively. Uncover fascinating bone factoids and learn about bone turnover and the factors that can affect bone health. Gain insights into why bone repair is crucial, how bone can deteriorate over time, and the vulnerability of vertebrae due to their bone composition.
Uploaded on Sep 12, 2024 | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
FractureFest May 2023 Treating Vertebral Fractures Dr Frazer Anderson FRCP FRACP Consultant in Geriatric Medicine Whangarei Hospital and Northland Region Te Whatu Ora Health New Zealand Te Tai Tokerau
Format of this session Impact of Vertebral Fracture Understanding the Spine Treating the Current Fracture Preventing the Next One
Frazers Fascinating Factoids If your bones were solid, you d be 8-12kg heavier We like crisps because we used to eat bones (mmm crunchy!) Cats are much, much more dangerous than sharks Bone drugs mostly come from washing powder
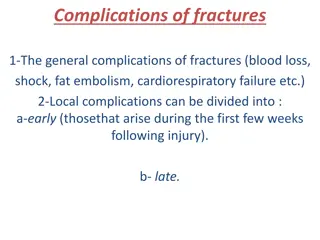
The impact of fractures Mrs C.W. Kyphosis from her late 60 s Pain, sleep Activities: cooking, sewing, shopping Social isolation, self-esteem Hip # aged 84: good recovery Hip # aged 91: passed away (pneumonia)
Get to Know your Spine The basic unit of all bony skeletons Dates back about 400m years Spines predate bones sharks use cartilage instead Shock absorption, core structure, flexibility, nerve protection Not designed to be used upright!
Bone Turnover Time
What is the point of all this? Unless bone is repaired, it gradually gets weaker Microfractures are normal after any vigorous activity The new bone is stronger and less brittle
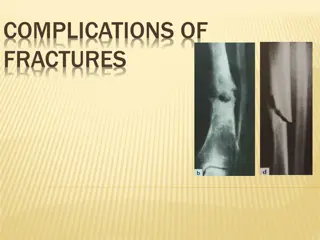
How does it all go wrong? Slightly less bone (~1%/year) added than removed - adds up over time Menopause (~3%/yr loss for ~10 years) Trabecular bone more affected Physical activity and bone loading change as we get older Co-dependency: muscle, ligaments, discs
Vertebrae have a high ratio of trabecular to cortical bone so are very vulnerable to bone loss Mild osteoporosis Severe osteoporosis
Loss of trabecular architecture of vertebrae in osteoporotic women Normal Woman * Osteoporotic Woman (with vertebral fracture) * Loss of bone mass and horizontal trabeculae * 3D Microcomputed tomography images Borah B et al. Anat. Rec. 2001; 265(2): 101-10
Cumulative risk of fracture Cumulative risk (%) 40 Fracture Site Hip (women) Vertebral (women) Wrist (women) Hip (men) Vertebral (men) Wrist (men) 30 20 10 0 50 55 60 65 70 75 80 85 90 Age (years)
Vertebral Fracture Treatment Pain relief Protection of spine function Physical rehabilitation Supporting social context
Pain Relief Analgesia Simple Opioids Neuropathic Heat or Cold, TENS Hydrotherapy warm water Spinal support? Vertebroplasty? Cognitive therapies
Pain Relief Acute pain typically lasts 4-12 weeks Risk of chronic pain rises steeply with increasing number of fractures Start with paracetamol + opioid Go in hard and back off quickly High risk of opioid dependency Avoid tramadol at all costs Muscle relaxant side effects limit use
Vertebral Fracture Prevention Osteoporosis medication Core strength and balance Falls interventions Managing frailty
What are bisphosphonates? Calcium binding agents Main use (~99%) is in detergents Clinical use discovered by accident during safety tests Interfere with bone resorption
How do bisphosphonates work? Absorbed poorly from gut - teaspoon of milk = zero absorption Short circulating half-life (~30 mins) Bind avidly to bone mineral then sit there doing nothing, often for years
How do bisphosphonates work? Ingested by osteoclasts Trigger detachment of osteoclasts from bone surface Detached osteoclasts automatically self- destruct (apoptosis) Summoned osteoblasts replace more bone mineral than has been removed Bone mineral content increases
Bisphosphonates Alendronate / Alendronic acid Reduces risk of all fractures in <80 y.o. Good long-term bone quality data Effective ( BMD) in, and licensed for, men Concordance not great Cheap as chips Risedronate Not inferior to alendronate First-line for CIOP in other countries, not NZ
Bisphosphonates Zoledronic Acid 5mg (Aclasta) Effective, high concordance (18-24 months) No data in older people Not suitable in chronic renal disease No longer needs Special Authority - hurray! Best choice for Fracture in alendronate-treated patients Concordance uncertain
Treatments for osteoporosis Teriparatide forces the body to build new bone very effective at reducing fractures has to be given by daily injection, expensive! Denosumab Very effective but nasty rebound if stopped Little used in NZ due to Pharmac restrictions Raloxifene reduces spine fractures but not others prevents common type of breast cancer
Drug Holidays More is not always better Atypical fracture risk How much is enough? 4-5 years of ALN 3 doses of ZOL BUT! Nobody knows how/when to restart!
Summary: Vertebral fractures Huge impact on quality of life Sentinel for non-spine fracture The spine is a complex organ Drugs are necessary but not sufficient Treat the person, not just the bone