Understanding Eczema: Causes, Classifications, and Pathogenesis
Eczema, a common skin condition, is characterized by inflammation and disrupting skin homeostasis. It can be classified morphologically and etiologically, with major pathogenesis factors including reduced skin barrier function and abnormal immune response. Atopic dermatitis, a form of endogenous eczema, is chronic and often affects infants and young children. Psychological factors may also play a role in the development of eczema.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
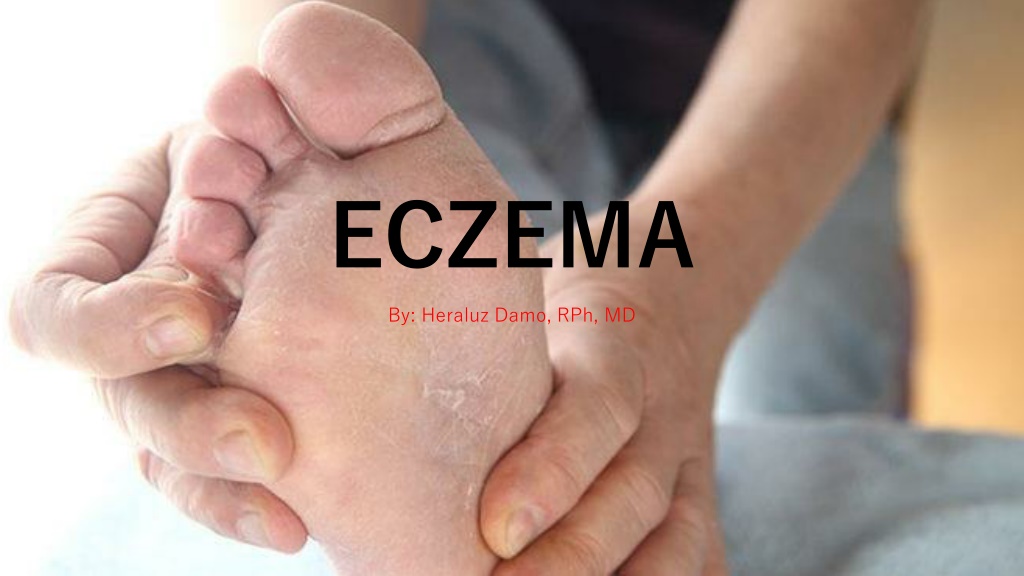
ECZEMA By: Heraluz Damo, RPh, MD
ECZEMA Greek word to boil out Incidence and Prevalence rate in the Philippines unknown
Eczema in Southeastern Asia (Extrapolated Statistics) 1,019,2522 East Timor 56,208 238,452,9522 Indonesia 13,149,978 6,068,1172 Laos 334,638 23,522,4822 Malaysia 1,297,195 86,241,6972 Philippines 4,755,975 4,353,8932 Singapore 240,104 64,865,5232 Thailand 3,577,142 Vietnam 4,558,610 82,662,800 Approximately 1:18 Filipinos
ECZEMA VS DERMATITIS ECZEMA VS DERMATITIS Synonymous A group of skin conditions Presence of inflammation (+) Reaction Pattern disrupting the normal homeostasis of the skin Irritant Allergen Disease Environmental Factors
3 MORPHOLOGICAL CLASSIFICATION 3 MORPHOLOGICAL CLASSIFICATION ACUTE SUBACUTE CHRONIC
ETIOLOGICAL CLASSIFICATION ETIOLOGICAL CLASSIFICATION EXOGENOUS Contact Dermatitis Phyto Dermatitis Photo Dermatitis ENDOGENOUS Atopic Dermatitis Pityriasis Alba Pompholyx Eczema Seborrheic Eczema Discoid Dermatitis LSC Noularis Prurigo Stasis Dermatitis
Major Pathogenesis of ECZEMA Major Pathogenesis of ECZEMA Reduced skin barrier function Abnormal immune response of the skin Abnormal response to bacterial infection Psychological factors
ATOPIC DERMATITIS ATOPIC DERMATITIS . The ITCH that RASHES
ENDOGENOUS ECZEMA ENDOGENOUS ECZEMA ATOPIC ECZEMA ATOPIC ECZEMA Chronic and relapsing inflammatory skin disease Found in infant , childhood and adult 6 to 9mos of age Peak incidence: 2-4yrs. of age improves by 10yrs. of age at 90% 5% to 10% continue throughout life
ENDOGENOUS ECZEMA ENDOGENOUS ECZEMA ATOPIC ECZEMA ATOPIC ECZEMA AD is a chronic relapsing inflammatory skin disease AD associated with local infiltration of Th 2 that secrete IL-4, IL-5, IL- 13, IL-31 More than 50% develop asthma 75% develop AR Complex interrelationship of genetic, environmental, immunologic, and epidermal factor Mark Boguniewicz, Donald Leung.Middleton s Allergy 7 th edition 1893-1999
ENDOGENOUS ECZEMA ENDOGENOUS ECZEMA ATOPIC ECZEMA EPIDEMIOLOGY ATOPIC ECZEMA EPIDEMIOLOGY Affects 15-30% of children, 2-10% of adult 60% begin during the first yr 45% begin within the first 6 mo 85% begin before 5 yrs Up to 70%: spontaneous remission before adolescence Predisposed to developing AR/asthma later in childhood .. Atopic march NJEM 2008;358:1483-94
ENDOGENOUS ECZEMA ENDOGENOUS ECZEMA ATOPIC ECZEMA EPIDEMIOLOGY ATOPIC ECZEMA EPIDEMIOLOGY Emerges in 1st month of life, while its prevalence decreases by age. Girls more often suffer from AD than boys ... but until age of 6, both sexes are affected equally. Increase exposure to allergen & decline in BF were reason for increasing of AD. Williams H.C.: Is the prevalence of atopic dermatitis increasing?. Clin Exp Dermatol 1992; 17:385-391 Childhood eczema found correlation with increased socioeconomic class Williams H.C., Strachan D.P., Hay R.J.: Childhood eczema: disease of the advantaged?. Br Med J 1994; 308:1132-1135
ENDOGENOUS ECZEMA ENDOGENOUS ECZEMA ATOPIC ECZEMA RISK FACTOR ATOPIC ECZEMA RISK FACTOR Genetic host factors Gene encoding epidermal or other epithelial structural proteins Loss of function mutations of epidermal barrier protein filaggrin (FLG) Transepidermal water loss (hallmark) & penetration of environmental allergens N Engl J Med 2008;358:1483-94
ENDOGENOUS ECZEMA ENDOGENOUS ECZEMA ATOPIC ECZEMA RISK FACTOR ATOPIC ECZEMA RISK FACTOR Genetic host factors Gene encoding major elements of immune system:3q21, 1q21, 16q, 17q25, 20p, 3p26 regulation of IgE synthesis Exaggerated T cell responses: imbalance between Th1 & Th2 Reduced skin innate immune response: human B defensins, cathelicidin, dermcidin (antimicrobial peptide) N Engl J Med 2008;358:1483-94
ENDOGENOUS ECZEMA ENDOGENOUS ECZEMA ATOPIC ECZEMA RISK FACTOR ATOPIC ECZEMA RISK FACTOR Environmental factors Food allergens (egg, milk, wheat, soy) Associate to infantile AD Related to disease severity Aeroallergens (pets, mites, pollen) Exacerbation AD in older children N Engl J Med 2008;358:1483-94
ENDOGENOUS ECZEMA ENDOGENOUS ECZEMA ATOPIC ECZEMA RISK FACTOR ATOPIC ECZEMA RISK FACTOR Other factors Weather conditions or humidity Skin irritants : soap, detergent Infections : S. aureus, M. furfur, HSV Emotional stress Persistent or worsening disease N Engl J Med 2008;358:1483-94
ENDOGENOUS ECZEMA ENDOGENOUS ECZEMA ATOPIC ECZEMA RISK FACTOR ATOPIC ECZEMA RISK FACTOR Other factors ATOPIC MARCH describes the tendency for atopic eczema to precede the development of food allergies, asthma, and allergic rhinitis in a temporal sequence Barrier dysfunction and immune response ATOPIC TRIAD Atopic dermatitis Allergy Asthma Primary Symptom: Pruritus N Engl J Med 2008;358:1483-94
ATOPIC DERMATITIS ATOPIC DERMATITIS PATTERNS OF INFLAMMATION PATTERNS OF INFLAMMATION ACUTE ATOPIC DERMATITIS (Acute AD) Erythema, vesicles, pruritus CHRONIC ATOPIC DERMATITIS (Chronic AD) Dryness, scaling, lichenification, fissuring, pruritus
ATOPIC DERMATITIS ATOPIC DERMATITIS ACUTE AD ACUTE AD Intensely pruritic, erythematous papule associated with excoriations, vesiculation, and serous exudate Pathology: Spongiosis (intercellular epidermal edema), superficial epidermal hypertrophy, acantholysis Marked infiltration of Your CD4 activated memory T cells, APC s and degranulated mast cells N Engl J Med 2008;358:1483-94
ATOPIC DERMATITIS ATOPIC DERMATITIS CHRONIC AD CHRONIC AD Thickened plaques with increased lichenification Pathology: marked epidermal hyperplasia, acanthosis Macrophage dominated mononuclear cell infiltrate and perivascular accumulation of lymphocytes in smaller numbers than seen in acute AD N Engl J Med 2008;358:1483-94
ENDOGENOUS ECZEMA ENDOGENOUS ECZEMA STAGES OF ATOPIC ECZEMA STAGES OF ATOPIC ECZEMA INFANT ATOPIC ECZEMA CHILDHOOD ATOPIC ECZEMA ADULT ATOPIC ECZEMA
STAGES OF ATOPIC ECZEMA STAGES OF ATOPIC ECZEMA INFANT ATOPIC DERMATITIS INFANT ATOPIC DERMATITIS -face and trunk are extremely involved -appear as eczematous patches, papulovesicular and crusty exudative lesions
Signs and Symptoms A rash that appears suddenly and: makes the skin dry, scaly, and itchy. forms on the scalp and face, especially on the cheeks can bubble up, then ooze and weep fluid. Rubbing against bedding, carpeting, and other things in order to scratch the itch Trouble sleeping Skin infections
STAGES OF ATOPIC ECZEMA STAGES OF ATOPIC ECZEMA CHILDHOOD ATOPIC DERMATITIS CHILDHOOD ATOPIC DERMATITIS -2 to 12 yrs. of age - flexural in distribution -pronounced papular and lichenified plaques, painful, itchy dry fissure eczema -fingers, wrist, ankle and toes are also affected
STAGES OF ATOPIC ECZEMA STAGES OF ATOPIC ECZEMA ADULT ATOPIC DERMATITIS ADULT ATOPIC DERMATITIS -Similar in childhood -Face and hands are commonly affected
ATOPIC DERMATITIS ATOPIC DERMATITIS CRITERIA FOR DIAGNOSIS CRITERIA FOR DIAGNOSIS MAJOR FEATURES: Pruritus Morphology & distribution (absence of sharp margin) Personal or Fhx of atopy MINOR FEATURES: Cataracts Conjunctivitis Keratoconus Orbital darkening Cheilitis
CLINICAL DIAGNOSIS CLINICAL DIAGNOSIS American Academy of Dermatology (AAD) 2014 Guidelines American Academy of Dermatology (AAD) 2014 Guidelines Essential features (must be present) are as follows: Pruritus Eczema (1) Typical morphology and age-specific patterns (2) chronic or relapsing history Important features (supports the diagnosis) are as follows: Early age of onset Atopy: (1) Personal and/or family history; (2) IgE reactivity Xerosis
CLINICAL DIAGNOSIS CLINICAL DIAGNOSIS American Academy of Dermatology (AAD) 2014 Guidelines American Academy of Dermatology (AAD) 2014 Guidelines Associated features (nonspecific but suggest the diagnosis of AD) are as follows: Atypical vascular responses (eg, facial pallor, delayed blanch response) Keratosis pilaris/pityriasis alba/hyperlinear palms/ichthyosis Ocular/periorbital changes Other regional findings (eg, perioral changes/periauricular lesions) Perifollicular accentuation/lichenification/prurigo
CLINICAL DIAGNOSIS CLINICAL DIAGNOSIS American Academy of Dermatology (AAD) 2014 Guidelines American Academy of Dermatology (AAD) 2014 Guidelines Exclusionary conditions (conditions that should be excluded) are as follows: Scabies Seborrheic dermatitis Contact dermatitis Ichthyoses Cutaneous T-cell lymphoma Psoriasis Photosensitivity dermatoses Immune deficiency diseases Erythroderma of other causes
CLINICAL DIAGNOSIS CLINICAL DIAGNOSIS American Academy of Dermatology (AAD) 2014 Guidelines American Academy of Dermatology (AAD) 2014 Guidelines Additional considerations in the diagnosis of AD are as follows: No reliable biomarker exists for the diagnosis of AD Laboratory testing is seldom necessary but a complete blood cell count can be useful to exclude immune deficiency; an IgE level can be helpful to confirm an atopic pattern; a swab of skin can be helpful to identify S aureus superinfection Allergy and radioallergosorbent testing is of little value Biopsy shows an acute, subacute, or chronic spongiotic dermatitis pattern that is nonspecific but can be helpful to rule out other conditions (eg, cutaneous T-cell lymphoma)
ATOPIC DERMATITIS ATOPIC DERMATITIS LABORATORY WORKUP LABORATORY WORKUP No biomarker for AD diagnosis Laboratory test is seldom necessary A swab of infected skin to isolate mo eithet Staph or Strep A swab for viral polymerase chain reaction (PCR) to identify superinfection with herpes simplex virus and identify a diagnosis of eczema herpeticum A complete blood cell count for thrombocytopenia helps exclude Wiskott-Aldrich syndrome, and testing to rule out other immunodeficiencies may be helpful. This also helps identify peripheral eosinophilia, which may help to support the diagnosis. A serum IgE level can be helpful to support the diagnosis. Scraping to exclude tinea corporis is occasionally helpful.
ATOPIC DERMATITIS ATOPIC DERMATITIS MANAGEMENT Agents typically used to treat AD include the following: Moisturizers: Petrolatum, Aquaphor, or newer agents such as Atopiclair and Mimyx Topical steroids (current mainstay of treatment; commonly used in conjunction with moisturizers): Hydrocortisone, triamcinolone, or betamethasone; ointment bases are generally preferred, particularly in dry environments Immunomodulators: Tacrolimus and pimecrolimus (calcineurin inhibitors; generally considered second-line therapy) Interleukin inhibitors: Dupilumab
ATOPIC DERMATITIS ATOPIC DERMATITIS OTHER TREATMENTS Ultraviolet (UV)-A, UV-B, a combination of both, psoralen plus UV-A (PUVA), or UV-B1 (narrow-band UV-B) therapy In severe disease, methotrexate, azathioprine, cyclosporine, and mycophenolate mofetil Everolimus Probiotics Antibiotics for clinical infection caused by S aureus or flares of disease Intranasal mupirocin ointment and diluted bleach (sodium hypochlorite) baths
ATOPIC DERMATITIS ATOPIC DERMATITIS NONMEDICAL MEASURES NONMEDICAL MEASURES Using soft clothing (eg, cotton) next to the skin; wool products should be avoided Maintaining mild temperatures, particularly at night Using a humidifier (cool mist) in both winter and summer Washing clothes in a mild detergent, with no bleach or fabric softener Avoiding specific foods as appropriate if there is concomitant food allergy
THANK YOU THANK YOU