Primary Care DES: Additional Roles Future Supply Workforce and Intelligence
The Primary Care DES introduces a scheme to recruit additional staff to address workforce shortages in general practice. Various reimbursable roles are available under the scheme, aiming to enhance capacity and support recruitment across different healthcare roles. Considerations are made regarding supply and utilization of these roles, including factors such as attrition from training and data sources. The plan aligns with the Long Term Plan's goal of recruiting 26,000 additional staff in Primary Care Networks over the next four years.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
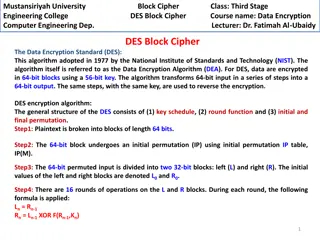
Primary Care DES: Additional Roles Future Supply Workforce and Intelligence, London
Introduction The Long Term Plan (LTP) sets out its support for the recruitment of 26,000 additional staff to work alongside doctors and nurses in Primary Care Networks (PCNs) over the next four years. Under a Network Contract Directed Enhanced Service (DES), funding is available to PCNs through a new Additional Roles Reimbursement Scheme across a number of specific roles. The intention of the scheme is to grow additional capacity through new roles, and by doing so, help to solve the workforce shortage in general practice. The scheme entitles PCNs to access funding to support recruitment across the following reimbursable roles: 1. Physician Associates 2. Physiotherapists. 3. Paramedics. 4. Clinical Pharmacists. 5. Social Prescribing Link Workers. 11. Care Coordinators 6. Occupational Therapists. 7. Podiatrists. 8. Pharmacy Technicians. 9. Dietitians. 10. Health and Well-being Coaches The following slides aim to summarise considerations relating to supply and effective utilization of these roles. Data availability varies between the roles largely because of different training course lengths and HEI reporting. As explained for each role, as applicable, new supply from HEIs does not represent the full picture, and there will be competition with private, secondary, and social care settings for some of the established roles.
Attrition from training Attrition from education and training can greatly impact student outturn. It is possible that now students are responsible for their own funding, students may leave their education because of affordability after starting. Alternatively, attrition may be reduced because individuals make a financially conscious decision before applying. Similarly, healthcare careers have seen a resurgence in interest since the COVID-19 pandemic and resultant recession, which may positively impact uptake and attrition. Attrition is a major unknown factor and won t be truly understood until the funding changes policies have bedded in. There are other personal reasons for attrition which mean it can be difficult to estimate the proportion of individuals that will leave training. Such as unexpected life events, a change in their relationship, health status or a desire to work abroad. They may find the reality of the course far from what they imagined and looking ahead they may feel that the job waiting for them is not something they want to do. Individuals can also step back on a course having had a break from training which makes calculating true attrition even more difficult.
About the data The future supply data used in this pack originates from HEE Contract Monitoring starters data. Using the count of starters and length of training of the different courses, the outturn is estimated. London HEI figures have been used, which assumes students will remain in the region in which they study; however it is acknowledged there is likely to be a degree of movement between regions post graduation. Attrition has not been applied to any of the outturn from 2020 onwards as it is difficult to estimate year on year, as previously explained. However, if it s known it s been highlighted in the text. Information about the profile of the existing workforce is taken from ESR. This only includes secondary care providers. As the majority of the reimbursement roles also require that staff have a number of years experience post graduation, student outturn is not solely representative of the workforce supply, and, as stated, existing workforce will also factor in. In respect of this, there will be a degree of competition across the wider NHS, and social care sectors; therefore there needs to be consideration of how candidates can be attracted to primary care, and of how primary and secondary care services may join forces to jointly tackle workforce and operational issues.
Physician Associates Physician Associate supply has seen a rise in course starters. Anticipated outturn for 2020 is 126, and for 2021 is 149. PA Predicted Outturn According to the first primary care workforce plan submissions, PCNs plan to increase their PA workforce by 210.9 FTE. This is the second largest planned growth in the established roles forming part of the ARRS (10.7%). It should be noted that this role is still in the process of becoming firmly established and embedded within the NHS, and is therefore subject to considerable variation across different specialty areas. 155 150 145 140 Factoring in that within the acute sector there are already a small number of vacancies and new supply will be required to replace leavers; competition from the acute sector for Physician Associates means it is unlikely that PCNs will be able to meet their projected recruitment to these roles within the stated timescales. 135 130 125 120 Exactly how many will be available to primary care will depend on the attractiveness and visibility of primary care roles compared with the acute sector. This will depend on individual motivations, but it should be noted that some roles within the acute sector offer rotational posts, and include opportunities to participate in surgical procedures, which may be seen as attractive. Consideration of joint posts, offering both primary and secondary care rotations could be beneficial across the NHS. 115 110 2020 2021 HEE Contract Monitoring starters data.
Clinical Pharmacists Pharmacists must complete a four year masters course followed by a one year pre-registration training placement. The individual can then register to work as a pharmacist. Newly registered pharmacists traditionally choose to work in the community or secondary care, starting at a band 6 level. As the ARRS is recruiting band 7/8a pharmacists, candidates will also need a degree of post-graduate experience to be considered. There are roughly 200 Pre-reg Pharmacists each year in London; however acceptances in London decreased by 2.5% from 2017 to 2019. Alongside a fairly static workforce (compared to other professions), increased demand in primary care will face competition from across the NHS. The 18-month general practice pharmacy training pathway equips clinical pharmacists and senior clinical pharmacists with the necessary knowledge, skills and experience to work in general practice as part of a multidisciplinary team in a patient-facing role. There are as 4283 FTE community pharmacists as of Dec 18 (latest data) but no breakdown by banding is available. There are a further 220.2 FTE primary care pharmacists for the same period, again with no banding breakdown available. Pharmacy banding profile (FTE) band 8+ band 7 band 6 band 5 band 1-4 0 100 200 300 400 500 600 700
Pharmacy Technicians Trainee Pharmacy Technicians must work under a qualified pharmacist or Pharmacy technician, and their technical skills can be used to support the clinical pharmacist to carry out audits, issue prescriptions, and in discharge management. Training takes 24 months, provided they are working a minimum of 30 hours/week, and courses have rolling start dates throughout the year. In 2018, there were 27 graduates, and numbers in training are approximately 200 currently. On qualifying, Pharmacy Technicians are employed at band 5 level. There is no obvious direct career progression pathway; however individuals may consider further study to become a pharmacist. During the BBS campaign, this group proved difficult to source when staffing the Nightingale hospitals; however the entry requirements for training are modest, and this role may appeal to a broad catchment, particularly as it offers on-the-job training. In secondary care there were 599 FTE band 5 Pharmacy Technicians as of June 2020, and 265 FTE at bands 1-4, plus 140 trainees. There were a further 431 FTE at band 6 or above. Training capacity in primary care settings should be considered as this will impact not only on uptake of Pharmacy Technicians, but also on the clinical capacity of qualified pharmacists. Pharmacy Technician banding profile (FTE) band 8+ band 7 band 6 band 5 band 1-4 0 100 200 300 400 500 600 700
Physiotherapists Physiotherapy has historically been a popular course with students due to the flexible employment model and attractive private practice opportunities. During the period where the NHS funded training, places were limited but they were always filled. PT Predicted Outturn 374 Since the funding model has changed, HEIs have been able to recruit more students which they have found easier than other courses to the point where clinical placements are becoming increasingly difficult to find. Clinical placements are now being held in private practice and not NHS settings. 372 370 368 The primary care workforce planning submissions currently project an increase of 188.4 FTE; however with vacancy rates this number may be larger. As FCP posts require a minimum of 3 years post-graduate experience, new supply needs to be considered alongside current workforce across the NHS as a whole, with an inherent degree of competition between primary and secondary care services. Joint posts could present one potential solution in this regard. 366 364 362 360 Physiotherapists also have more opportunities to work in private practice than any other AHP group, introducing another competing sector. PCNs need to ensure the attractiveness of working in general practice outweighs that of private practice. Career progression and skills development will be key to this. 358 2020 2021 Physiotherapist secondary care banding profile (FTE) Approximately a third of physiotherapists in secondary care are band 7, with a further 16% band 8a and above. Band 8+ Using a Physiotherapist as a first contact practitioner within a PCN, would allow patients to book their first appointment with a musculoskeletal problem with this practitioner rather than being screened by a GP. The physiotherapist would need to be highly experienced to be able to make a quick and accurate diagnosis, create a management plan independently, manage complex patients who have many comorbidities and be able to know when pain is not a msk cause, or presents a potential emergency, and instead should be redirected to a GP. This means that a PCN will need to employ an experienced physiotherapist for this role rather than one straight out of training. Physiotherapists will require 3-5 years of experience in order to train to become a FCP in primary care. Band 7 Band 6 Band 5 Band 1-4 0 500 1000 1500 ESR June 2020
Paramedics In July 2018, following considerable improvements to vacancy, turnover and sickness rates and improvement in CQC rating, HEE s financial support for workforce development at London Ambulance Service (LAS) was brought in line with other London NHS employers after around ten years of considerable funding to support recruitment and retention activities. Paramedic trainee outturn from HEIs 400 Understandably LAS will be nervous about their future workforce, as the reimbursement scheme provides other avenues of employment for paramedics. Yet with the low volume of potential retirees in the existing workforce, there should be sufficient future supply to refill any paramedics that do retire at LAS while also providing a moderate supply to PCNs if required. 356 350 289 300 It is likely that a paramedic role in primary care will offer a different intensity to that compared with LAS which could suit some individuals more than others benefitting all organisations. There is consideration of a rotational programme to offer primary care experience to counter-balance some of the high stress of the traditional paramedic role. 267 250 200 Important to note that Paramedics remain on the shortage occupation list (this is UK wide). 150 100 50 0 2020 2021 2022 HEE Contract Monitoring starters data.
Occupational Therapists All AHP professions have faced similar issues since changes were introduced to the funding model; however there are fewer opportunities for OTs to launch directly into private practice than for physiotherapists. Due to their broad skillset and holistic perspective, OTs are well placed to work with the breadth of issues encountered in primary care. OTs require 3-5 years post-graduate experience in order to be eligible to train as a FCP; therefore supply will compete with secondary care services, as well as social care, and mental health services. As there is potential to bypass the GP referral process practitioners will require a high level of skill in assessment. Career progression may be limited; therefore there is a need to consider how to attract and retain practitioners to this setting. Roles in primary care are likely to appeal to clinicians seeking to work autonomously, with a broad general skillset. Flexible working patterns may further enhance appeal, particularly as this is a limitation in the acute sector. Consideration will also need to be given to access to supervision, and peer networks across PCNs may provide a solution. Approximately one third of OTs in secondary care are at band 7, with a further 11% at band 8. There is a need to consider practice patient demographics for best use, i.e. most OTs will have specialised in either physical or mental health, and have limited recent experience in other areas of practice; therefore how practices envision using them will likely depend on the needs of the local population. OT secondary care banding profile (FTE) Band 8+ Band 7 Band 6 Band 5 0 500 1000 1500
Dietitians All AHP professions have faced similar issues since changes were introduced to the funding model; however there are fewer private practice opportunities for most AHP groups, including dietitians, compared to physiotherapists due to the nature of the work. Dietitians will require 3-5 years post-graduate experience to be eligible to train as a FCP; therefore supply will compete with other services, including secondary care, as with FCPs from other AHP groups. Career progression may be limited therefore employers will need to consider how to attract and retain practitioners to this setting flexible working options may be attractive. 46% of dietitians in secondary care are at band 7, with a further 13% at band 8. There is the potential to bypass GP referrals for certain interventions, particularly weight management support, and follow up for nutritional support post hospital discharge; however this requires a high level of skill in assessment to ensure important diagnoses are not missed. Dietetics secondary care banding profile (FTE) Band 8+ Band 7 Band 6 Band 5 0 50 100 150 200
Podiatrists Similar to physiotherapy, podiatrists have greater opportunities to work in private practice than most AHP groups; however they will need 3-5 years experience to be eligible to train as a FCP; therefore supply will still compete with secondary care services. FCP roles may appeal to many podiatrists working in private practice; however supply in this area is unknown. Career progression may be limited therefore need to consider how to attract and retain practitioners to this setting flexible working options may be attractive. Numbers in secondary care are low, but band 7 s make up 37% of the workforce, with the bulk being comprised of band 6 staff. There is potential to bypass GP referral, freeing up GP appointment times; however this will require a high level of skill in assessment in order to make accurate diagnoses and ensure patients receive the highest standards of care. There is potential to support primary care practice with specific initiatives, e.g. diabetic foot health clinics. Podiatry secondary care banding profile (FTE) Band 8+ Band 7 Band 6 Band 5 0 50 100 150 200
Public Health Roles Social Prescribing Link Workers | Health & Well-being Coaches | Care Co-ordinators As these are new roles, it is not yet clear how they will work in practice, nor how easy they will be to staff; however, given the entry level requirements, there is a potentially broad appeal to individuals seeking secure employment and on-the-job development, particularly in a time of recession. There may be some overlap or interchangeability with some of these roles, depending on the needs of the population, and practices should consider carefully the needs of their populations. Due to shorter duration of training (up to 7 months) there is potential to staff these roles relatively quickly; however for face to face training this will be restricted by the number of colleges/training centres offering these courses. HEE does not have numbers for this training supply. These roles are also likely to have limited career progression pathways which may impact recruitment; however they may be seen as introductory roles to the health service in general, and therefore act as a springboard into other health and social care professions. Careful consideration should be given to promotion and recruitment of these roles to maximise uptake.