Understanding the Importance of Mortality Risk in Chart Review
The presentation by Kerry Seekircher highlights the significance of considering the risk of mortality in chart reviews. It covers the benefits of conducting a mortality review, emphasizes the need for accurate documentation and coding of diagnoses, and explains the concept of risk-adjusted mortality. The components of a mortality review process are also discussed, focusing on the critical role of clinical documentation and coding in assessing patient outcomes. By understanding and addressing mortality risk factors, healthcare providers can improve patient care and outcomes.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Importance of Considering Risk of Mortality in Chart Review Kerry Seekircher, RN, BSN, CCDS, CDIP January 18, 2018 1
Agenda Introduction Kerry Seekircher, RN, BS, CCDS, CDIP, Director of Clinical Documentation Improvement at Northern Westchester Hospital in Mount Kisco, NY Mortality Review I. Review benefits of conducting a Mortality Review II. Review components of a Mortality Review III. Conducting a Head to Toe Assessment-Key Diagnoses to Consider IV. Case Studies V. Coding Clinics-Cardiac Arrest and Palliative Care VI. Questions and Answers January 18, 2018 2
Benefits of Conducting a Mortality Review January 18, 2018 3
Benefits of Conducting a Mortality Review Mortality data is publicly reported-accuracy is key Ensure all clinically significant diagnoses are documented and coded to the highest level of specificity Critically ill & expired patients should have critical diagnosis codes, not symptoms Source: https://support.northwell.edu/view.image?Id=2314 For the reviewer Learn or further strengthen skills to better identify opportunity across the board in all types of reviews January 18, 2018 4
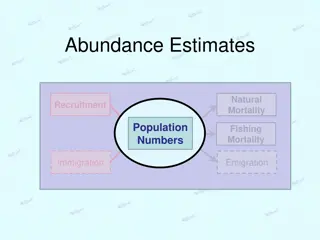
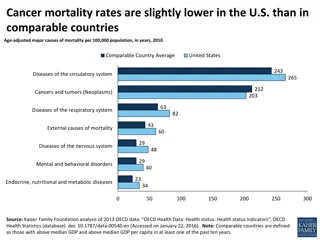
Risk-Adjusted Mortality Mortality Index Used to compare observed mortality rates with those of other hospitals around the nation. Risk-Adjusted Mortality Takes into consideration risk factors such as age, severity of illness and other medical problems that can put some patients at greater risk of death than others. = Observed rate/risk-adjusted expected rate Equal to 1= Average mortality rate Greater than 1= Higher than average mortality rate Less than 1= Better than average mortality rate January 18, 2018 5
Components of a Mortality Review January 18, 2018 6
Components of a Mortality Review Process varies from site to site. Presentation focuses on mortality reviews, however concepts apply to all roles involving inpatient chart reviews. The mortality review begins with concurrent Clinical Documentation chart review and routine queries as indicated. Consider second level review once the chart has been coded, but before bill drops to assess for opportunity. January 18, 2018 7
Components of a Mortality Review Consider the Principal Diagnosis (PDX); Does the current PDX match the acuity of the inpatient encounter? - Patients do not routinely get admitted and expire from Dehydration or Simple Pneumonia. Are there documented co-morbid conditions and major co-morbid conditions (CC s and MCC s)? - Patients do not routinely get admitted and expire without cc s and mcc s and/or a form of organ failure. Review procedure documentation and coding. What is the current Severity of Illness and Risk of Mortality (SOI/ROM)? - Optimal SOI/ROM is 4/4 Conduct head to toe assessment-see slides 10-24. Consider ICD-10 codes for Palliative Care and DNR. January 18, 2018 8
Head to Toe Assessment January 18, 2018 9
Nervous System Diagnoses When you see these Symptoms Consider these Diagnoses AMS Obtunded Mass Effect Unresponsive Midline Shift Coma/Unconsciousness Cerebral Edema Cerebral Compression Cerebral Herniation Encephalopathy (type?) Review Glasgow Coma Scale (GCS) Treatments may include: ICU, Surgery, IV/PO Steroids, Comfort Care, Head CT Key places to look for clinical indicators: Imaging, EMS and Nursing for GCS information January 18, 2018 10
Glasgow Coma Scale The Glasgow Coma Scale (GCS) is based on the patient s best response in three areas : Eye opening Verbal response Motor response Coma codes that are MCC s are: Coma GCS eye opening score - Never (R40211-) - To pain (R40212-) GCS verbal response score - None (R40221-) - Incomprehensible (R40222-) GCS motor response score - None (R40231-) - Extensor (R40232-) - Flexion (R40234-) Source: 2017 CDI Pocket Guide, Richard D. Pinson, MD, FACP, CCS and Cynthia L. Tang, RHIA, CCS January 18, 2018 11
Glasgow Coma Scale The Glasgow Coma Scale is for use in any setting and non-provider documentation of the score can be coded (EMT, Nursing). A correlating diagnosis needs to be documented by the provider in order to be coded. Avoid coding the GCS score in the setting of a transient diagnosis such as the post-ictal period following a seizure or for brief loss of consciousness (LOC) following a syncopal event. The GCS score should be coded by its individual components versus the total score when documented (*E, V, & M). The 7th character of component codes identifies when the scale was recorded (in the field, arrival to ER, etc..) Documentation opportunity: Are the GCS scores built into the EMR at your facility? See below for a screenshot of NWH s nursing documentation. Source: 2017 CDI Pocket Guide, Richard D. Pinson, MD, FACP, CCS and Cynthia L. Tang, RHIA, CCS January 18, 2018 12
Coding Clinic for ICD-10 CM Q1. 2014, Pgs. 19-20 Glasgow Coma Score Question: ICD-10-CM provides codes to identify the Glasgow coma scale (GCS) score. When the patient presents with a traumatic brain injury (TBI), these codes are used in conjunction with the specific codes describing the TBI. If the emergency medical technician (EMT) documents the patient's initial GCS score in the field, can the EMT's documentation be used? Coders are concerned that there is no official advice or guideline that allows use of nonphysician documentation for the Glasgow coma scores. These scores are typically documented by personnel other than physicians. What documentation can be used for determining the ICD-10-CM Glasgow coma score code? AHA Coding Clinic Answer:It would be appropriate to use the pre-hospital report containing the EMT's documentation, and other nonphysician documentation to determine the Glasgow coma score. January 18, 2018 13
Coding Clinic for ICD-10 CM Q2. 2015, Pgs. 17-18 Glasgow Coma Scales Question: Can individual Glasgow coma score (GCS) codes be assigned based on documented numeric values rather than the description of the codes (e.g., eyes open to pain, best verbal response, etc.)? When reporting the GCS, can a total score be calculated if only individual scores are documented? AHA Coding Clinic Answer: Yes, if the provider's documentation clearly shows that the ratings are specific scores or numeric values for the Glasgow scale, it would be appropriate to report codes from categories R40.21-, R40.22- and R40.23-. These codes are used only when the individual score(s) or numeric values are documented within the health record. Do not assign code R40.24-, Glasgow coma scale, total score, if the individual scores are documented. Assign code R40.24-, Glasgow coma scale, total score, when only the total score is documented in the medical record and not the individual score(s). The 7th character indicates when the scale was recorded. The 7th character should match for all three codes. January 18, 2018 14
Coding Clinic for ICD-10 CM Q4. 2016, Pgs. 64-65 Glasgow Coma Scale Subcategory R40.24-, Glasgow coma scale, total score, will require a 7th character to indicate when the scale was recorded. The 7th characters are similar to those already in existence for the Glasgow coma scale individual scores (R40.21- to R40.23-): AHA Coding Clinic 0 1 2 3 4 - - - - - unspecified time in the field [EMT or ambulance] at arrival to emergency department at hospital admission 24 hours or more after hospital admission A code from subcategory R40.24 should be assigned when only the total coma score is documented. In addition, the ICD-10-CM Official Guidelines for Coding and Reporting have been revised so that the coma scale codes may also be used to assess the status of the central nervous system for other nontrauma conditions, for example monitoring patients in the intensive care unit regardless of the medical condition. Prior to this change, the Official Coding Guidelines specified that the coma scale codes (R40.2-) could only be used in conjunction with traumatic brain injury codes, acute cerebrovascular disease or sequelae of cerebrovascular disease codes. January 18, 2018 15
Coding Clinic for ICD-10 CM Q4. 2017, Pg. 95 Medically Induced Coma and Glasgow Coma Score Question: A critically ill patient had a medically induced coma. Should we assign a Glasgow coma score for a patient in a medically induced coma? AHA Coding Clinic Answer: Do not report individual or total GSC scores codes for a patient with a medically induced coma. This type of reversible coma is induced with drugs to help protect the brain from swelling by decreasing blood flow as well as the metabolic rate of brain tissue. January 18, 2018 16
Respiratory System Diagnoses When you see these Symptoms Consider these Diagnoses Shortness of breath (SOB) Respiratory Distress Arterial Blood Gas (ABG) results (no diagnosis) Hospital Acquired Pneumonia Atypical Pneumonia Aspiration Fluid Overload Acute Respiratory Failure (hypoxic, hypercapneic) Respiratory Acidosis/Alkalosis Pneumonia Specificity (Gram Negative, Aspiration, MRSA Pneumonia, etc..) Acute Pulmonary Edema (non- cardiogenic) Treatments may include: High-flow O2, ICU, IV Vancomycin & Zosyn, IV Lasix Key places to look for clinical indicators: O2 flow rate, ABG findings, & antibiotic selection January 18, 2018 17
Circulatory System Diagnoses When you see these Symptoms Consider these Diagnoses Chest pain Acute Coronary Syndrome (ACS) Fluid Overload Code called Hypotensive on vasopressor medications Hypertensive urgency Acute MI (specify type) Unstable angina Acute Systolic/Diastolic CHF Cardiac Arrest Shock (specify type) Hypertensive emergency Hypertensive crisis Treatments may include: Cardiac consult, Percutaneous Coronary Intervention (PCI), anti-thrombotic, anticoagulant, anti-platelet therapy, ICU, vasopressors & anti-hypertensives January 18, 2018 18
Digestive System Diagnoses When you see these Symptoms Consider these Diagnoses Rigid Abdomen Acute Abdomen Ischemic Colitis Abdominal pain Elevated Liver Function Tests (LFT s ) Peritonitis Bowel Perforation Common Bile Duct Obstruction Acute Ischemic Colitis Acute Liver Failure Shock Liver Treatments may include: Antibiotics, Comfort Care, IV fluids January 18, 2018 19
Kidney and Urinary System Diagnoses When you see these Symptoms Consider these Diagnoses Urosepsis CKD Stage unspecified Renal Insufficiency AKI due to contrast, hypotension and/or Sepsis Sepsis secondary to UTI (assess for link to indwelling catheter or device) CKD with Stage specified AKI Acute Tubular Necrosis (ATN) Treatments may include: IV antibiotics, IV fluids, Renal Consult January 18, 2018 20
Blood Disorders When you see these Symptoms Consider these Diagnoses Unspecified Anemia Drop in hemoglobin and hematocrit (h&h) Pancytopenia Thrombocytopenia Acute Blood Loss Anemia Pancytopenia secondary to Chemotherapy Disseminated Intravascular Coagulation (DIC) Heparin Induced Thrombocytopenia (HIT) Treatments may include: Transfusions, IV fluids, ICU January 18, 2018 21
Infectious Diseases When you see these Symptoms Consider these Diagnoses Urosepsis Fever Unknown Origin (FUO) on antibiotics Infection Bacteremia Sepsis Sepsis severity-Severe? Septic Shock? FUO-suspected bacterial infection (on antibiotics) (A49)-MS-DRG 867-869 Neutropenic Fever Bacteremia on long term antibiotics-Acute Endocarditis? Treatments may include: IV antibiotics, ID Consult, PICC January 18, 2018 22
Nutrition Diagnoses When you see these Symptoms Consider these Diagnoses Failure to thrive Poor appetite, weight loss, muscle wasting BMI <19 or >40 without associated diagnosis NPO for extended period Protein Calorie Malnutrition-include severity Obesity-morbid? Cachexia Treatments may include: Registered Dietician consult, supplements, TPN/PPN, tube feeds, calorie counts, Pro-stat, diet changes January 18, 2018 23
Nursing Diagnoses When you see these Symptoms Consider these Diagnoses RN documentation of pressure ulcers Complete immobility Total care Generalized deconditioning following prolonged ICU stay MD documentation of pressure ulcers-document POA status Functional Quadriplegia Critical Illness Myopathy/Polyneuropathy Treatments may include: Total nursing care, wound care consult, dressing changes, PT/OT Key places to look for documentation: Nursing, PT/OT notes *Functional Quadriplegia should be avoided in the setting of acute symptoms due to a current illness and hospitalization. This is a chronic issue. January 18, 2018 24
Functional Quadriplegia Defined The lack of ability to use one s limbs or to ambulate due to extreme debility. It is not associated with neurologic deficit or injury, and code R53.2 should not be used for cases of neurologic quadriplegia. It should only be assigned if functional quadriplegia is specifically documented in the medical record. A few common causes include: Severe, end-stage dementia Advanced progressive neuro-degenerative disorders (e.g., Multiple Sclerosis and ALS) Severe brain injury/brain damage Sources: ICD-10-CM Official Coding Guidelines Section I.C .18.f. 2017 CDI Pocket Guide, Richard D. Pinson, MD, FACP, CCS and Cynthia L. Tang, RHIA, CCS January 18, 2018 25
Functional Quadriplegia Clinical Indicators Nursing notes describe a total care patient Documentation of immobility requiring turning and positioning every 2 hours or more, bedridden, and the inability to independently perform activities of daily living (ADL s) May have contractures Braden scores Most often found in nursing assessments Mobility score of 1 (completely immobile) or 2 (very limited) Activity score of 1 (bedridden) Source: 2017 CDI Pocket Guide, Richard D. Pinson, MD, FACP, CCS and Cynthia L. Tang, RHIA, CCS January 18, 2018 26
Mortality Review Case Studies January 18, 2018 27
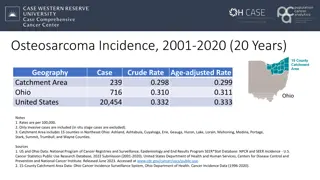
Mortality Case Study #1-Neurovascular Case summary: Patient presents with massive right sided hemispheric intracerebral hemorrhage with interventricular extension. She now has extensor posturing on examination. She is comatose and vent dependent. Neurosurgery documents Given massive hemorrhage with herniation, I see no role for surgical intervention. Second level review findings: Provider documentation of comatose, cerebral edema, herniation and individual GCS scores had been documented but were not coded. Pre-Mortality Review Post-Mortality Review MS-DRG 065 Intracranial Hemorrhage or Cerebral Infarction with CC or tPA in 24 hours MS-DRG 064 Intracranial Hemorrhage or Cerebral Infarction with MCC or tPA in 24 hours SOI/ROM 3/4 Relative Weight 1.0313 Average Length of Stay 4 days SOI/ROM 4/4 Relative Weight 1.7691 Average Length of Stay 6 days January 18, 2018 28
Mortality Case Study #2-Respiratory Case summary: Patient presents after a recent discharge with acute respiratory distress and hypoxia. She is diagnosed with Hospital Acquired Pneumonia, COPD exacerbation and Acute Hypoxic Respiratory Failure. The doctor ordered Vancomycin, Fortaz, IV steroids, and the patient was placed on BIPAP. She initially improved, but her hospital course was complicated by Septic Shock. She expired after being placed on comfort care. Second level review findings: Upon review, CDI nurse found clinical indicators to support a provider query for pneumonia specificity. The provider documented Given recent discharge from the hospital and clinical presentation, the patient was treated with IV Fortaz and Vancomycin for the treatment of suspected Gram Negative and MRSA pneumonia. Pre-Mortality Review Post-Mortality Review MS-DRG 190 MS-DRG 177 Chronic Obstructive Pulmonary Disease with MCC SOI/ROM 3/4 Relative Weight 1.1528 Average Length of Stay 5 days Respiratory Infections and Inflammations with MCC SOI/ROM 4/4 Relative Weight 1.8509 Average Length of Stay 7 days January 18, 2018 29
Coding Clinic for ICD-10 CM Q3. 2016, Pgs. 15-16 Chronic Obstructive Pulmonary Disease with Lobar Pneumonia Question: The patient has chronic obstructive pulmonary disease (COPD), and is admitted to the hospital for treatment of lobar pneumonia. Under code J44.10, Chronic obstructive pulmonary disease with acute lower respiratory infection, there is a note instructing: "Use additional code to identify the infection." Based on this note is the COPD required to be sequenced first? AHA Coding Clinic Answer: Yes, based on the instructional note, the COPD must be sequenced first. Assign code J44.0, Chronic obstructive pulmonary disease with acute lower respiratory infection, as the principal diagnosis. Code J18.1, Lobar pneumonia, unspecified organism, should be assigned as an additional diagnosis. January 18, 2018 30
Coding Clinic for ICD-10 CM Q4. 2017, Pg. 96 Bacterial Pneumonia, Influenza A, & Acute Exacerbation of COPD Question: The patient was admitted with wheezing and shortness of breath. The provider's diagnostic statement listed, "Bacterial pneumonia on top of influenza A, exacerbation of chronic obstructive pulmonary disease (COPD)." Would a combination code be assigned for the influenza with pneumonia and COPD and pneumonia; or should each condition be coded separately? Does the fact that a combination code is assigned for COPD with acute lower respiratory infection affect assigning an additional code for influenza with pneumonia? How would this case be coded? AHA Coding Clinic January 18, 2018 31
Coding Clinic for ICD-10 CM Q4. 2017, Pg. 96 Bacterial Pneumonia, Influenza A, & Acute Exacerbation of COPD Answer: Assign code J10.08, Influenza due to other identified influenza virus with other specified pneumonia; code J44.0, Chronic obstructive pulmonary disease with acute lower respiratory infection; code J15.9, Unspecified bacterial pneumonia; and code J44.1, Chronic obstructive pulmonary disease with (acute) exacerbation. All four codes are needed to capture the diagnostic statement. The circumstances of the admission would determine the principal diagnosis. Please note that effective October 1, 2017, the "use additional code to identify the infection" note at code J44.0, Chronic obstructive pulmonary disease with acute lower respiratory infection, has been revised to "Code also to identify infection." AHA Coding Clinic January 18, 2018 32
Cardiac Arrest I46.9 January 18, 2018 33
Cardiac Arrest as the Principal Diagnosis Cardiac Arrest should be selected as the PDX only when the underlying cause cannot be determined. Query the provider in the circumstance where there is evidence of an undocumented underlying etiology. Image source: https://www.northwell.edu/sites/northwell/files/styles/news_la rge/public/behavioral%20health/news/heartrhythm_1_6.JPG?it ok=cqh3h1i- January 18, 2018 34
Coding Clinic for ICD-10 CM Q3. 1995, Pgs. 8-9 Cardiac Arrest with Bradycardia and Hypotension Question: When a patient suffers a cardiac arrest is it appropriate to code the accompanying symptoms such as bradycardia and hypotension? AHA Coding Clinic Answer: No, symptoms that are integral to the cardiac arrest such as bradycardia and hypotension are not coded or reported. Cardiac arrest can result from cardiac causes (e.g., ventricular fibrillation, ventricular tachycardia, bradyarrhythmia, asystole, supraventricular tachyarrhythmia), or from abnormalities in respiration that lead to acute respiratory acidosis (cardiopulmonary arrest). Clinical findings may consist of significant arterial hypotension, nonpalpable pulse, absent heart sounds, apnea, and loss of consciousness. January 18, 2018 35
Coding Clinic for ICD-10 CM Q1. 2013, Pg. 9 Pulseless Electrical Activity Question: Physicians are documenting pulseless electrical activity (PEA) rather than cardiac arrest, when patients are being resuscitated during a code blue situation. Is it appropriate to assign code 427.5, Cardiac arrest, when PEA is documented within the health record? AHA Coding Clinic Answer:Assign code 427.5, Cardiac arrest, for pulseless electrical activity. PEA refers to electrical activity on a monitor without a detectable pulse. It is one of the rhythms that cause a pulseless cardiac arrest. PEA usually has some underlying cause that can be treated, with the most common cause in emergency situations being hypovolemia. PEA can be caused by respiratory failure with hypoxia, as in this case the cardiac muscle is unable to generate a sufficient force despite an electrical depolarization. True PEA is the absence of myocardial contraction despite coordinated electrical activity. *Cardiac Arrest code updated in ICD-10 to I46.9 January 18, 2018 36
Coding Clinic for ICD-10 CM Q1. 2013, Pg. 10 Cardiac Arrest without Underlying Condition Question: The patient is a 65-year-old male, who presents to the emergency department (ED), with complaints of severe chest pain and suffers a full cardiac arrest. Cardiopulmonary resuscitation is initiated, and the patient is defibrillated, intubated and placed on mechanical ventilation. He is admitted to the hospital's intensive care unit (ICU). Shortly after admission to the ICU, the patient's family decides to withdraw life support and the patient expires. The underlying cause of the cardiac arrest is unknown. How should this case be coded? AHA Coding Clinic *Cardiac Arrest code updated in ICD-10 to I46.9 January 18, 2018 37
Coding Clinic for ICD-10 CM Q1. 2013, Pg. 10 Cardiac Arrest without Underlying Condition Continued Answer:Assign code 427.5, Cardiac arrest, as the principal diagnosis. Assign codes 99.62, Other electric countershock of the heart, 96.71, Continuous mechanical ventilation for less than 96 consecutive hours, and code 96.04, Insertion of endotracheal tube, for the procedures performed. Cardiac arrest can be the principal or first-listed diagnosis if the underlying condition is not known. It does not matter whether the patient is resuscitated or not. The assignment and sequencing of code 427.5, Cardiac arrest, is dependent upon the circumstances of the hospitalization. If the patient is admitted due to cardiac arrest and an underlying cause is not established before the patient is discharged or expires, it is appropriate to assign code 427.5 as the principal or first-listed diagnosis. Code 427.5 should not be sequenced as the principal or first-listed diagnosis if the underlying condition is known. It may be assigned as a secondary diagnosis code when it meets the definition of a reportable additional diagnosis, regardless of whether the patient is resuscitated or not. AHA Coding Clinic *Cardiac Arrest code updated in ICD-10 to I46.9 January 18, 2018 38
Coding Clinic for ICD-10 CM Q1. 2013, Pg. 11 Cardiac Arrest Occurs During or Following Surgery Question: When cardiac arrest occurs during or following surgery, and the patient cannot be resuscitated, is cardiac arrest assigned as an additional diagnosis? AHA Coding Clinic Answer: Assign both codes 997.1, Complications affecting specified body systems, not elsewhere classified, Cardiac complications, and 427.5, Cardiac arrest, as additional diagnoses, when cardiac arrest is documented as occurring during or following surgery, regardless of outcome (successfully resuscitated or not resuscitated). *Cardiac Arrest code updated in ICD-10 to I46.9 January 18, 2018 39
Coding Clinic for ICD-10 CM Q1. 2013, Pgs. 11-12 Cardiac Arrest with Underlying Condition Question: The patient is a 75-year-old female with no significant past medical history. She was found unresponsive at home and emergency medical services (EMS) were called. EMS initiated cardiopulmonary resuscitation (CPR). Upon arrival in the Emergency Department (ED), the patient was unresponsive and was found to have lethal paroxysmal ventricular tachycardia, which was successfully defibrillated. She was admitted to the hospital and underwent placement of an implantable cardioverter defibrillator (ICD) to prevent recurrence of the arrhythmia. The provider documented that the lethal paroxysmal ventricular tachycardia was the underlying cause of the cardiac arrest. Is it appropriate to code the cardiac arrest since the underlying cause is known? AHA Coding Clinic *Cardiac Arrest code updated in ICD-10 to I46.9 January 18, 2018 40
Coding Clinic for ICD-10 CM Q1. 2013, Pgs. 11-12 Cardiac Arrest with Underlying Condition Answer:Assign code 427.1, Paroxysmal ventricular tachycardia, as the principal diagnosis. Code 427.5, Cardiac arrest, should be assigned as a secondary diagnosis. When the condition prompting the cardiac arrest is known, the condition causing the arrest is sequenced first, followed by code 427.5 when it meets the definition of a reportable additional diagnosis, regardless of whether the patient is resuscitated or not. Assign code 37.94, Implantation or replacement of automatic cardioverter/ defibrillator, total system [AICD], and code 99.62, Other electric countershock of the heart, for the procedures performed. AHA Coding Clinic *Cardiac Arrest code updated in ICD-10 to I46.9 January 18, 2018 41
Palliative Care Z51.5 January 18, 2018 42
Dos and Don'ts of Querying While on Comfort Care DO Query Question: A patient is placed on comfort care. During morning rounds, the patient complains of a sore throat and is found to have white patches in her mouth. The MD orders Nystatin swish and swallow but no diagnosis is documented. Is it appropriate to query for a diagnosis even though the patient is on comfort care? Answer-Yes. The patient has symptoms of a diagnosis and is receiving active treatment. DON T Query Avoid a query for acute respiratory failure when a patient experiences hypoxia after initiation of a morphine drip for comfort care as this is an expected outcome. January 18, 2018 43
Coding Clinic for ICD-10 CM Q1. 1998, Pgs. 11-12 Clarification, Palliative Care A new code for palliative care, V66.7, became effective October 1, 1996. A brief explanation of how it should be used was published in Coding Clinic, Fourth Quarter 1996. A further explanation is now being provided to clarify the proper use of the code. Code V66.7 can be used for any terminally ill patient receiving palliative care. It is always a secondary code. The terminal condition should be the principal diagnosis. It may be used when a patient is brought in for aggressive treatment for a terminal condition and during the encounter it is determined that further aggressive treatment is no longer appropriate and palliative care is initiated. The physician documentation in the medical record must substantiate that palliative care is being given. Terms such as comfort care, end-of-life care, and hospice care are all synonymous with palliative care. These, or similar terms, need to be written in the record to support the use of code V66.7. The physician should be queried if the treatment record seems to indicate that palliative care is being given but the documentation is unclear. The care provided must be aimed only at relieving pain and discomfort for the palliative care code to be applicable. AHA Coding Clinic *Palliative Care code updated in ICD-10 to Z51.5 January 18, 2018 44
Coding Clinic for ICD-10 CM Q3. 2008, Pgs. 13-14 Palliative Care Question: An elderly patient with metastatic lung carcinoma is admitted with fever and chills and is diagnosed with pneumonia and urinary tract infection. The principal diagnosis is pneumonia. During the hospitalization, the patient develops severe sepsis and respiratory failure requiring a ventilator. On the day before the patient expires, she is extubated and taken off of Levophed. On the day she expired, the physician documented, "extubated yesterday with goals of comfort/ palliative care." In addition, the physician's plan states, "Continue palliative approach to respiratory failure--increase Morphine to limit work of breathing, stop intensive monitoring, consult palliative care service, continue scopolamine." The patient expired an hour after this note was written. Is it appropriate to assign code V66.7, Encounter for palliative care, as a secondary diagnosis in this situation? AHA Coding Clinic *Palliative Care code updated in ICD-10 to Z51.5 January 18, 2018 45
Coding Clinic for ICD-10 CM Q3. 2008, Pgs. 13-14 Palliative Care Continued Answer:Yes, it would be appropriate to assign code V66.7, Encounter for palliative care, as a secondary diagnosis in this case. This code may be reported for any terminally ill patient who receives palliative care, regardless as to when the decision is made. There is no time limit or minimum for the use of this code assignment. As stated in Coding Clinic, First Quarter 1998, pages 11-12, "Code V66.7 can be used for any terminally ill patient receiving palliative care. It is always a secondary code. The terminal condition should be the principal diagnosis. It may be used when a patient is brought in for aggressive treatment for a terminal condition and during the encounter it is determined that further aggressive treatment is no longer appropriate and palliative care is initiated. AHA Coding Clinic *Palliative Care code updated in ICD-10 to Z51.5 January 18, 2018 46
Coding Clinic for ICD-10 CM Q3. 2010, Pgs. 18-19 Comfort Care Question: The patient, an 88-year-old male, was admitted to the intensive care unit (ICU) following a massive intracerebral hemorrhage. Because of patient age, the size of the hemorrhage, and poor prognosis, a conference was held with the family and they agreed to discontinue life support and declined placement of a feeding tube. The provider documented comfort care and pain control. What clinical protocol is required in order to assign code V66.7, Encounter for palliative care? Is it appropriate to assign code V66.7 as a secondary diagnosis? AHA Coding Clinic Answer:Yes, assign code V66.7, Encounter for palliative care, as an additional diagnosis. Code V66.7 is for use to describe comfort care, palliative care and/or end of life care for terminally ill patients. If, however, the documentation is not clear regarding palliative care versus nonpalliative, query the provider for clarification. It is beyond the scope of the Editorial Advisory Board for Coding Clinic to provide clinical protocol for palliative care. *Palliative Care code updated in ICD-10 to Z51.5 January 18, 2018 47
Summary Mortality data is publicly reported information. - US News, Healthgrades, Press Ganey Conduct a second level review to ensure the PDX, CC s & MCC s are both documented and coded to the appropriate level of specificity. Perform a head to toe assessment when reviewing the medical record to assess for documentation and/or coding opportunities to support the resources utilized during the inpatient encounter. When appropriate, query the provider to obtain documentation to support the conditions being treated. Use caution in querying for conditions which arise during the palliative care period unless they are being treated and/or monitored or are otherwise in accordance with coding guidelines. January 18, 2018 48
Thank You Kerry Seekircher, RN, BSN, CCDS, CDIP Director, Clinical Documentation Improvement Northern Westchester Hospital 400 East Main Street Mount Kisco, NY 10549 Phone: 914-666-1243 kseekircher@nwhc.net January 18, 2018 50