Understanding and Managing Chronic Conditions
Chronic conditions affect millions of people, requiring long-term management and lifestyle changes. Patients must adapt physically, socially, and emotionally, facing different phases throughout their lives. Prevention is crucial, but once a chronic disease occurs, focus shifts to symptom management, avoiding complications, and promoting health. Nurses play a key role in supporting patients through the various phases, providing care, teaching self-care, and addressing challenges unique to each stage of the illness trajectory.
Uploaded on Sep 23, 2024 | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
C A N C E R OBJECTIVE 8 This Photo by Unknown Author is licensed under CC BY
Chronic Conditions Occur in people of every age, socioeconomic level, and culture ~ 16 million Canadians live with at least one chronic condition Medical conditions or health problems with associated symptoms that require long-term (3 months or longer) management Conditions that do not resolve or for which complete cures are rare Management means that people must learn to live with the symptoms or disabilities and carry out lifestyle changes or treatment regimens Chronicity = diseases with prolonged trajectory and are incurable, therefore difficult to manage
The patient must adapt and change physically, socially, psychologically, and emotionally Usually involve different phases during the person s lifetime to which the person must adapt (i.e. acute, stable, remission, flare ups) Require adherence to therapeutic regimen Characteristics of Chronic Conditions One chronic disease or problem can lead to another Chronic disorders contribute to higher risk of mortality and morbidity from other illnesses Affect the entire family Management is unique to everyone and includes trial and error Course of illness cannot be accurately predicted
Managing Chronic Conditions Importance of prevention health promotion/prevention Lifestyle changes or interventions to prevent chronic disease Once the disease occurs, focus shifts to: Managing symptoms Avoiding complications Avoiding acute illness Promoting health Maintaining functional status
Chronic Illness Trajectory Model 3. Stable phase symptoms are being managed 1. Pretrajectory phase being at risk 2. Trajectory phase onset of symptoms 4. Unstable phase exacerbation of symptoms 5. Acute phase sudden onset of severe symptoms 6. Crisis phase a life-threatening situation 7. Comeback phase after recovery from acute phase 8. Downward phase worsening despite management 9. Dying phase decline
Nursing Care of Chronic Illness Often supportive patient is normally in the community Challenging owing to the difficulty of predicting the trajectory of the illness Teaching Self Care Each phase brings unique challenges to the nurse Not every person goes through every stage Challenges include Alleviating and managing symptoms Psychologically adjusting to physical disabilities Adhering to treatment regiment Family functioning Managing exacerbations
Oncology Nursing Chapter 17 Oncology is a branch of medicine dealing with tumors/cancers Concerns/needs of clients with cancer Prevent infection Skin protection/integrity Mucous membranes Hair loss/wt. gain /loss Nutrition Fatigue Pain Anticipatory grieving Body image, low self esteem, loss of control
Cancer Epidemiology A group of more than 200 diseases Progress made with modifying risk factors Leading cause of death in every Canadian province Heart disease a close second Incidence higher in men, and higher in industrialized nations Estimated 187 600 new cases of and 75 000 deaths from cancer in 2013 Lung, colorectal and prostate Ca leading cause of death in men GI, Lung, breast and colorectal are leading cause of death in women Estimated Canadians expected to die from cancer Risk Factors Smoking, Diet, Sedentary lifestyle, Obesity, Sun exposure, Alcohol
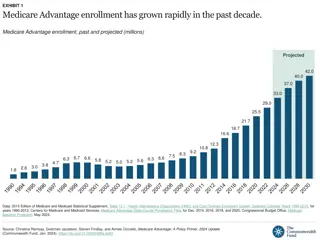
Statistics (2017) Nearly 1 in 2 Canadians is expected to be diagnosed with cancer at some point during their lifetime. Although an increasing number of Canadians are surviving at least five years past their cancer diagnosis, cancer continues to be the leading cause of death in Canada. About 1 in 4 Canadians is expected to die from cancer It is projected that the number of cancers diagnosed in 2030 will be almost 80% greater than the number diagnosed in 2005.(2) Although this increase is due to the growing and aging Canadian population rather than an increase in risk, these numbers have important implications for Canadians and Canadian healthcare resources. Immense progress has been made in cancer control in Canada as a result of advances in prevention, screening, early detection, and treatment.
Males: 1. Prostate 2. Colorectal 3. Lung and Bronchus Females: 1. Breast 2. Lung and Bronchus 3. Colorectal All Canadians/ 5 year survival rate: 1. Lung/ 17% 2. Colorectal/ 64% 3. Breast/ 87% 4. Prostate/ 95%
Healthy Cells Have specialized function depending on their location (differentiated). Cells grow, replicate, and repair tissues and organs. Your immune system and your genetic material (DNA/RNA) regulate these processes. Healthy cells are programmed what to do and when to do it. Blood cells Muscle (smooth, striated, cardiac) cells Nerve cells Bone cells Cartilage cells Liver cells
Cancer Cells Mutated cells Cannot regulate their replication and pass on the genetic mutations. Bear little resemblance to the normal cells of tissue from which they arose. Don t do their original job. Cell membranes contain tumor-specific antigens which develop overtime as cell become less differentiated. Have invasive characteristics to infiltrate other tissues. Common Terms Differentiation: The process of cells developing into mature healthy cells with explicit characteristics and capabilities to do a certain function. Fetal cells are less differentiated but become more differentiated as the cells mature. When a cell develops mutations, it becomes less differentiated, meaning it looks less and doesn t function like the cell it once was or was meant to be. Metastasis: process of infiltrating tissue, spreading from the original development site. Angiogenesis: growth of new capillaries from the host tissue to nourish the cancer cells. Carcinogenesis: transformation of a healthy cell into a cancer cell.
Pathophysiology: Cancer Abnormal, unrelated cell proliferation that competes with healthy cells/tissue for oxygen, nutrients, and space. Abnormal cell replicate faster than normal cells, passing on their defective DNA that do not have regulatory mechanisms to prevent overgrowth. Neoplasms: new growths of abnormal tissue Result: steal oxygen and nutrition, alter function of health tissue and organs
Cancer Cancer cells are described as malignant Uncontrolled growth/proliferation Classified according to cell origin and whether benign or malignant Benign: Non invasive, does not spread, noncancerous, may cause minor tissue damage, does not cause major injury unless cause pressure/obstruction to organs Malignant: Invasive, spreads/metastasizes, recurrence is common, death if uncontrolled First part of name refers to specific cell involved, and suffix oma indicates it is a tumour Lymphoma Glioblastoma
Cells that remain in one area are considered localized or in situ Spread of Cancer: Metastasis Metastasis describes spread of cancer from primary site through: 1. invasion of blood or lymph 2. Mechanical movement 3. Lodging and growing in a new location (lymphatics/angiogenesis)
Carcinogens Physical Agents Sunlight, radiation (ex: x-ray), chronic irritation/inflammation, tobacco use Chemical agents Tobacco smoke, chewing tobacco, workplace substances Diet Fat, smoked meats and high calorie diet, alcohol, red & processed meats Viruses HPV, AIDS Kaposki s sarcoma Bacteria H-pylori Genetics/familial Genes, shared environments, cultural or lifestyle factors Defective genes (BRCA-1, 2; HNPCC) Hormones Endogenous or exogenous hormones Medical interventions HRT, immunosuppressive drugs
Avoid second hand smoke; be a non smoker 5-10 servings of fruit and veggies a day Limit alcohol to 1-2 drinks per day Reduction of Risk Factors Regular physical activity Sun protection Follow cancer screening guidelines Visit MD if you notice any changes in your health Follow health and safety instructions at home and when using and storing or disposing of hazardous materials Avoidance of known carcinogens
Change in bowel or bladder habits A sore that does not heal Unusual bleeding or discharge Thickening or lump in breast or elsewhere Indigestion or difficulty swallowing Obvious change in wart or mole Nagging cough or hoarseness Warning Signs of Cancer: C.A.U.T.I.O.N
Lab tests: Tumor markers that cancer cells release PSA, CA-125 CBC, stool for FOB, bone marrow aspirate Diagnostic Tests Radiologic: X-ray, mammography, fluoroscopy, barium studies CT scan Nuclear medicine imaging (PET Scan) MRI Biopsy, cytology, Frozen sections Endoscopy
Classification of Tumors: Anatomical Carcinomas Leukemias Lymphomas 4. Sarcomas Cancer that originates from epithelial tissue Adenocarcinoma glandular epithelium Cancer that originates from organs that form blood Cancers that originate from organs that fight infection (lymphoid tissue Hodgkin's disease and non- Hodgkin's lymphoma; plasma cells multiple myeloma) Cancers that originate from connective tissue such as muscle and bone Osteosarcoma
In histological grading of tumors, the appearance of cells and the degree of differentiation are evaluated Graded from I IV, the higher the grade the more undifferentiated the cells and the poorer the prognosis Histological Classification: Grading Grade I: Cells differ slightly from normal cells (mild dysplasia) and are well differentiated. Grade II: Cells are more abnormal (moderate dysplasia) and moderately differentiated. Grade III: Cells are very abnormal (severe dysplasia) and poorly differentiated. Grade IV: Cells are immature and primitive (anaplasia) and undifferentiated; cell of origin is difficult to determine.
Clinical Staging Classifying the extent and spread of disease is termed staging. This classification system is based on a description of the extent of the disease rather than on cell appearance. Stage 0: cancer in situ Stage I: tumour limited to the tissue of origin; localized tumour growth Stage II: limited local spread Stage III: extensive local and regional spread Stage IV: metastasis
TNM Classification System Table 18-6 Most common international system for staging tumors: T = Primary Tumor Size, N = Involvement of Lymph Nodes, M = Metastasis Primary Tumor (T) T0 = No evidence of primary tumor Tis = Carcinoma in situ T1 T4 = Ascending degrees of increase in tumor size and involvement TX = Primary tumor cannot be assessed Involvement of Lymph Nodes (N) N0 = No evidence of disease in lymph nodes N1 N3 = Ascending degrees of nodal involvement Nx = Regional lymph nodes cannot be assessed Metastasis (M) M0 = No distant metastases M1 = Distant metastases MX = Distant metastases cannot be assessed
Collaborative Care: Goals The goal of cancer treatment is cure, control, or palliation These goals are achieved through four treatment modalities: chemotherapy, radiation, surgery, and biological therapy
Primary and oldest method of diagnosing, staging, and treating cancers Cure = removal of tumor with margins of surrounding tissue as well Control = debulking removal of as much as possible Palliative = pain/symptoms relief (colostomy, feeding tube, etc) Potential effects of clients: postsurgical complications, disfigurement, rehabilitation Treatment Modalities: Surgery
Treatment Modalities: Chemotherapy Antineoplastic agents interfere with cellular function, reproduction Administration Oral, IM, IV, intraperitoneally, intraarterially, intrapleural, topically Careful handling and administration, may be occupational hazard Dosage and agent(s) unique to client Special courses required in order to be able to administer chemotherapy
Hypersensitivity (type1): 5% chance Extravasation: leak into tissues directly (tissue necrosis) Nausea (first and most common); Stomatitis: mucosal lining of mouth Mucositis: inflammation GI lining Bone marrow suppression (7-14 days post) Sterility Alopecia (temporary or permanent) Renal damage; Heart Failure Peripheral neuropathy, muscle weakness, imbalance Chemotherapy: Potential Effects
Cause tissue disruption by alteration of DNA of molecule leading to cell death Cells that undergo frequent cell division (cancer cells) are more sensitive to radiation Treatment Modalities: Radiation Therapy External Radiation Therapy (Teletherapy) High energy x-rays aimed at specific locations Internal Radiation Therapy (Brachytherapy) Short distance therapy: Less radiation, used alone or in combination
Cumulative Skin reactions: erythema to dry desquamation(flaking), moist desquamation (dermis exposed, skin oozing), ulceration Oral: Stomatitis, xerostomia, change and loss of taste, dysphagia Anorexia, nausea, vomiting, diarrhea (if colon in irradiated field) Leukopenia and thrombocytopenia( if bone marrow in irradiated field) Radiation: Potential Effects Long term effects - irreversible Fibrosis : small intestine, lungs, & bladder, Cataracts, Sterility, Blood cell formation disturbances, & New cancers
Biological Therapy Treatment involving the use of biological agents such as interferons, interleukins, monoclonal antibodies, and growth factors to modify the relationship between the host and the tumor They have direct antitumor effects They restore, augment, or modulate host immune system They have other biological effects, such as interfering with the Result in inflammatory, and immune responses flulike symptoms are common. Many receive premedication with acetaminophen mechanisms cancer cells ability to metastasize or differentiate Neurological deficits are also commonly observed
Bone marrow transplantation: Self Review Page 343 Hyperthermia: Malignant cells may be more sensitive to the harmful effects of high heat as they cannot repair themselves. Used in combination with other treatments. External or internal. Medical Management: Other Clinical trials: Certain biological modifiers, antibodies, vaccines, gene therapy that may help Biological modifier methods that alter the immunologic r/s between host and cancer cells: monoclonal antibodies, cytokines, retinoids, cancer vaccines Complementary and alternative therapies mind-body relaxation, herbs, acupressure, etc
Common Nursing Interventions: Chemotherapy/Radiation Therapy Monitor side effects of effects of chemotherapy & radiation - BITES B - Bleeding suggests low platelet count (monitor labs, safety, injury prevention) I - Infection PPE, infection control strategies (Hematology PPT), boost immunity strategies monitoring labs, IV sites, and skin T - Tiredness suggests anemia (Activity based on conserving energy and physical status, foods with iron, B12, folic acid) E - Emesis (risk for altered nutrition, F&E balance- oral nutrition preferred first, see tips) S - Skin changes (radiation reaction or breakdown: maintain pH, moisture, prevent shear forces, prolonged pressure oral MM : routine and good oral hygiene)
Nursing Diagnosis: Patient with Cancer Impaired tissue integrity: malignant skin lesions Impaired oral mucous membrane Impaired tissue integrity Impaired tissue integrity: alopecia Imbalanced nutrition, less than body requirements Anorexia Malabsorption Cachexia Disturbed body image Anticipatory grieving Chronic pain Fatigue
Psychological support Pain management Fatigue Impaired skin integrity Nutrition Infection Nursing Care: Client with Cancer
As important as the medical treatments and physical care Promotes hope, self esteem and spiritual needs Clients and families/significant others have varied responses. Assess coping skills Support to the client and family Refer to pastoral care, counselling Important to consider: Disfigurement, Disability, Culture, Age, Sexuality, Mental status, Grieving as a normal process Nursing Care: Psychological Support
Nursing Care: Pain Management Moderate to severe pain occurs in approximately 50% of patients receiving active treatment for cancer and in 80% of those with advanced cancer Pain may be due to the cancer process and/or treatments Frequently undertreated for a variety of reasons Inadequate assessment need to ask if having pain, VS not a good indicator Fear of addiction/being loopy Pharmacological and non pharmacological approaches Opioids taken regularly with breakthrough if needed Imagery, massage, heat/cold, etc.
Nursing Care: Fatigue Most significant and frequent symptom for those receiving cancer therapy and the stress of coping Factors such as weight loss, anemia, depression, nausea, and other symptoms exacerbate the sensation of fatigue Maintaining good nutrition and adequate hydration, alternating periods of rest and activity, relying on family members for assistance with responsibilities, and managing pain and anxiety may help reduce fatigue Prepare patients for fatigue so they do not feel it is a sign of progressing disease/treatment failure
Impaired Skin Integrity Stomatitis: inflammation of oral tissues; 5- 14 days after certain chemo/ or radiation to head/neck Radiation- associated skin impairment: pain, irritation, pruritus, burning Malignant skin lesions erythema, nodules, edema, exudate, necrosis Important to adhere to proper cleansing, reducing bacteria, controlling bleeding, relieving pain Table 18-15
Anorexia, malabsorption, cachexia (weakening/wasting of body) Can have physical and psychosocial consequences Malnutrition Advanced stages may need nutritional support via enteral route
Malnutrition: Tips for Poor Appetite Eat your biggest meal when your appetite is best. This may be at breakfast time rather than at the evening meal, depends on the client Eat often through the day Try to eat something every 1 2 hours Have small snacks between meals everyday. Snacks can give extra energy. Include a high protein food at each meal and snack. Carry snacks if planning to be away from home Try a few mouthfuls even if not hungry Eat high energy and high protein foods most of the time. Limit low fat, calorie reduced or diet foods Drink liquids that give energy through the day such as milk, smoothies, commercial nutritional supplement drinks or juice.Limit low calorie fluids such as water, coffee and tea as they will fill clients up and not allow them to eat much at mealtimes Eat foods that taste good to you. It is okay to eat the same foods often if only a few foods appeal to you Source: http://www.bccancer.bc.ca/
Infection remains a major cause of morbidity and mortality in cancer patients Typical signs of infection may not occur immunosuppressed patients Nursing Care: Infection Fever may be only sign in immunosuppressed patient Prevent septicemia and septic shock life threatening; those with neutropenic & hematologic malignancies are at greatest risk Control bleeding and hemorrhage Prompt assessment and treatment is crucial
Oncological Emergencies Life threatening events that occur as a result of cancer or treatments. Can be obstructive, metabolic, or infiltrative Obstructive Tumor obstruction of organ/vessels Superior Vena Cava Syndrome, Intestinal obstruction, spinal cord compression, third space syndrome Metabolic Production of ectopic hormones SIADH, hypercalcemia, tumor lysis syndrome, septic shock & DIC Infiltrative Tumors infiltrate organs secondary to therapy Cardiac tamponade, carotid artery rupture
To provide care for people who are dying, while enabling them to live as normally as possible with dignity and with as much freedom from pain as possible Active, compassionate care of the terminally ill at a time when goals of a cure or prolongation of life are no longer paramount Palliative Care Emphasis of care is on comfort and quality of life until death Goals of palliative care Provide relief from symptoms, including pain Regard dying as a normal process. Affirm life and neither hasten nor postpone death. Support holistic patient care and enhance quality of life. Offer support to patients to live as actively as possible until death. Offer support to the family during the patient's illness and in their own bereavement.
Prioritizing Nursing Care for Palliative Clients A Good Death Meaning-Making Know what this means for your client: ensuring last rights if desired, ensuring family presence, or if wants to be alone, absence from pain, looks good! Family Recognition/Care Transitioning the meaning of hope, foster reminiscence of good memories, pastoral care- voicing regrets/forgiveness etc Pain/Comfort Relational, spiritual, emotional (therapeutic touch, visiting, pastoral care, being relational, using therapeutic communication techniques- validating, listening, rephrasing, silence, presence etc.) Ongoing communication, updates, family meetings, rest periods, establishing trust Pain/Comfort Physical sources (medication, position, skin care, warmth, cooling, mucous membranes) CNA_2020 45
Transition from Active Treatment to Palliative Care Initiate discussion Establish supportive relationship Ensure plan of care is consistent with family/patient view Find out how best to support family/patient Address questions/concerns Discuss: how have major decisions have been made in past How treatment decisions have been made during the illness How does patient/family want decisions made from now on? Setting for palliative care; family involvement in care Clarify understanding of the medical treatment plan and prognosis Identify what pt/family understand Identify gaps, need for consultation Use simple everyday language Identify end-of-life priorities Facilitate open discussions about priorities What is most important to you now? How can we best help you to meet your goals ? Allow time for emotional response Contribute to interprofessional care plan Provide guidance/referrals to understand medical options Make recommendations to other disciplines Identify need for more teaching Develop a plan for follow-up care: Schedule (frequency, time, place) Participants Tasks/assignments Communication that needs to occur before the next meeting Family member responsible for co-ordination
Death The minimum acceptable clinical standards to test for the cessation of circulatory function are: (1) absence of palpable pulse, (2) absence of breath sounds, (3) absence of heart sounds, (4) absence of respiratory effort or chest wall motion, (5) loss of pulsatile arterial blood pressure according to noninvasive measurement, and (6) coma and fixed pupils, observed continuously and confirmed after 2 to 5 minutes
Signs of Approaching Death: Table 13-3 As cells deteriorate, body receives insufficient oxygen and multisystem organ failure occurs Sensory: decreased sight, taste, smell. Hearing usually last to go Cardiovascular: Low BP/HR, irregular rhythm, weak pulse Respiratory: Cheyne-Stokes breathing, agonal breaths, death rattle inability to clear secretions Urinary: Decreased urine output, incontinence GI: Loss of appetite, slowed GI movement, Nausea, BM at time of death M/S: Increasing weakness, loss of gag reflex, dysphagia, dysarthria Skin: Mottling, Cold/clammy skin, Cyanosis nose, ears, nail beds, Skin becomes wax- like near time of death Neurological: Confusion, restlessness due to low oxygen, inability to control body temperature (hot/cold flashes)
Psychosocial care Table 13-10 Acknowledge fear, anger, feelings of grief/powerlessness Nursing Care: End of Life Pain management* Physical care Table 13-11 Post-mortem care
Review Videos/Quizzes Cancer cells : https://www.youtube.com/watch?v=UopUxkeC4Ls https://quizlet.com/13825862/med-surg-nursing-cancer-flash- cards/ https://quizlet.com/136060997/med-surg-ch25-patient-with- cancer-study-guide-and-nclex-questions-flash-cards/ (1199) Cancer: Pathophysiology, Risk Factors, Signs/Symptoms and more - Medical Surgical | @LevelUpRN YouTube (1199) Cancer: Nursing Care and Patient Teaching - Medical-Surgical | @LevelUpRN - YouTube