Chronic Care Management (CCM) Overview and Eligibility
Chronic Care Management (CCM) offers benefits such as improved patient care and satisfaction through person-centered and coordinated care. Eligible individuals with multiple chronic conditions at significant risk can receive CCM services from qualified practitioners including physicians, nurse specialists, and midwives. While a face-to-face visit is required for new patients or those not seen in the past year, existing patients like Mrs. Jones may provide consent for CCM without an additional visit.
Uploaded on Sep 23, 2024 | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
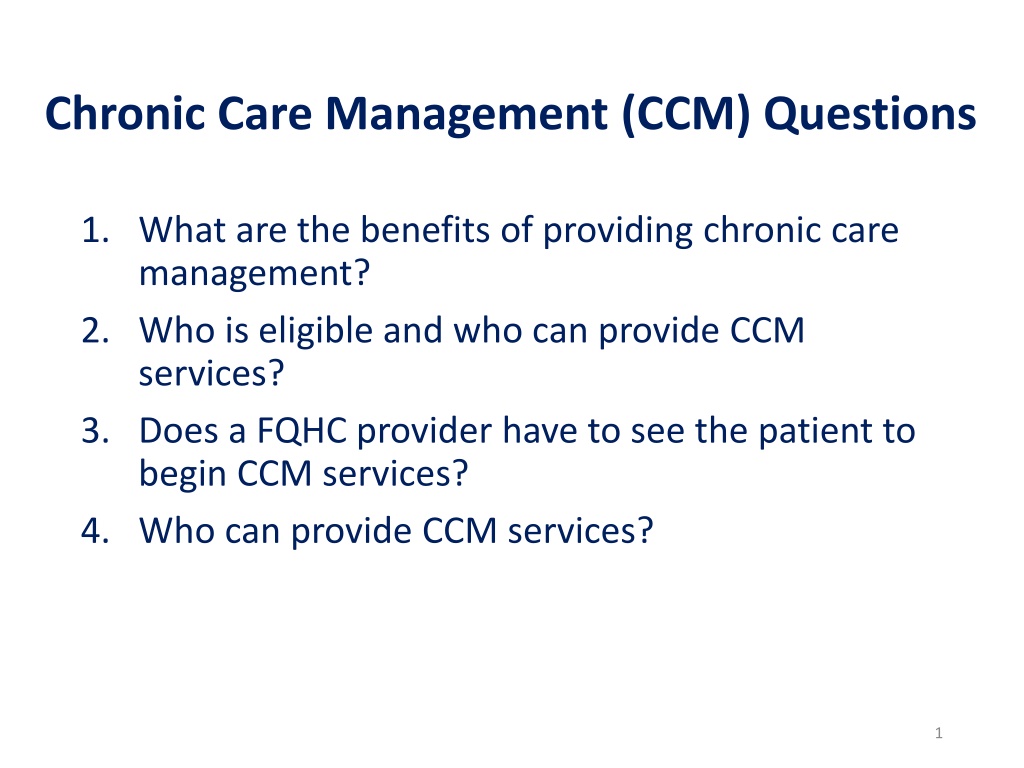
Chronic Care Management (CCM) Questions 1. What are the benefits of providing chronic care management? 2. Who is eligible and who can provide CCM services? 3. Does a FQHC provider have to see the patient to begin CCM services? 4. Who can provide CCM services? 1
1. What are the benefits of providing chronic care management? CCM is an opportunity to improve care and patient satisfaction CCM is person-centered CCM requires more centralized management of patient needs and extensive care coordination among practitioners and providers 2
2. Who is eligible and who can provide CCM services? Eligible beneficiaries have: Two or more chronic conditions expected to last at least 12 months or until death, that place them at significant risk of death, acute exacerbation, or functional decline Eligible reporting practitioners/providers: Physicians, Physician Assistants, Clinical Nurse Specialists, Nurse Practitioners, and Certified Nurse Midwives RHCs and FQHCs CCM Services Fact Sheet December 2016 https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network- MLN/MLNProducts/Downloads/ChronicCareManagement.pdf 3
3. Does a FQHC provider have to see the patient? For new patients or patients not seen within the last year: Prior to performing CCM services, the provider must furnish a face-to-face comprehensive E&M visit, Annual Wellness Visit, or Initial Preventive Physical Examination, the patient must be properly informed about the nature of CCM services (including how to revoke the service if desired) and consent must be obtained from the patient and documented in the EMR. For patients that have been seen within the last year: *Mrs. Jones, an existing patient, would be a good candidate for CCM services. Mrs. Jones has had an office visit with a FQHC practitioner within the last 365 days, but CCM services were not discussed during that visit. Would Mrs. Jones need to come in and have a face-to-face office visit with a FQHC practitioner to provide the informed consent process so that staff can begin CCM services? 1. In your scenario, Mrs. Jones would not need to come in for a face-to-face visit, but would still need to provide consent to receive CCM services. 2. Consent for CCM can be provided by clinical staff but must be documented in the medical record. * Summary of email conversation between Melanie and the CMS FQHC PPS Team from 8/1- 8/8 4
4. Who can provide CCM services? Can clinical staff explain CCM services to the patient and obtain informed consent or does that have to be done by a FQHC practitioner? Consent for CCM can be provided by clinical staff but must be documented in the medical record. (Email CMS FQHC PPS Team). Yes, qualified auxiliary staff (clinicians such as nurses, medical assistants, and others who furnish services incident to a RHC/FQHC visit) who are subject to general supervision complete the consent process. general supervision requirements can Consent for CCM can be provided by clinical staff and documentation of acceptance must exist and include: cost sharing ($8), that only one physician can bill for CCM, patient may stop the service at any time and whether they accepted or declined services. Consent may be verbal or written but must be documented in the medical record, and includes informing them about: (CCM Services Dec 2016) - availability of CCM services and applicable cost-sharing ($8) - only one practitioner can furnish and be paid for CCM services during a calendar month - right to stop CCM services at any time (effective at the end of the calendar month) Once the patient has consented to receive CCM services, can other staff furnish CCM services? Yes Yes once the patient has consented to receive this service, any RHC/FQHC practitioner (physician, nurse practitioner (NP), physician assistant (PA), certified nurse midwife (CNM), clinical psychologist (CP), or clinical social worker (CSW)), or qualified auxiliary staff (in accordance with the direct supervision requirements) can furnish the CCM services. (CCM Services in FQHCs FAQs 2/19/16) (CCM Services in FQHCs FAQs 2/19/16) CCM Services in FQHCs FAQs 2/19/16 https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/FQHCPPS/Downloads/FQHC-RHC-FAQs.pdf CCM Services December 2016 https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network- MLN/MLNProducts/Downloads/ChronicCareManagement.pdf 5
Additional Note: CCM Services Additional Note: CCM Services Q14. Can CCM costs such as software or management oversight be included on the cost report? Yes. Any cost incurred as a result of the provision of RHC and FQHC services, including CCM, is a reportable cost and must be included in the Medicare cost report. CMS will be adding a line to both the RHC (CMS-222-92) and FQHC (CMS-224-14) cost report on Worksheet A to specifically report costs associated with the provision of CCM. CCM Services in FQHCs FAQs February 19, 2016 https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/FQHCPPS/Downloads/FQHC-RHC-FAQs.pdf CHAPTER 29 INDEPENDENT RURAL HEALTH CLINIC AND FREESTANDING FEDERALLY QUALIFIED HEALTH CENTER COST REPORT FORM CMS-222-92 Line 55.50.--This cost center includes the cost related to the structured recording of patient health information, an electronic health care plan addressing all health issues, access to chronic care management (CCM) services, managing care transitions, and coordinating and sharing patient information with practitioners and providers outside the practice. CCM services are reimbursed as an add-on payment based on the Medicare Physician Fee Schedule (MPFS). See 80 FR 71080 (November 16, 2015). 7
Provider reviews the summary and bills/signs the encounter Pt is educated about CCM services by Care Mgr during MWV Pt is identified as qualified for CCM services during MWV Once billable time is achieved, a summary is sent to the provider Provider reiterates CCM services during CCM Gaston Family Health Services CCM Process Pt messages are sent to the provider for FYI and action (as needed) Pt is identified as CCM patient in the EMR The time spent with the pt, and a pt note is documented in the EMR Pt is follow up is based on goals set during the CCM High Risk pt engagement is attempted each month 8
Caswell Family Medical Center We use eCW and have a timer built into our system. We have one nurse who is designated to work on CCM. This nurse is responsible for enrolling patients in the program, completing care plans and following up with these patients monthly. All licensed clinical staff can use the timer when completing non face to face care such as medication refills, reviewing labs, reviewing reports from specialists, referral tracking, answering telephone messages, etc. If someone forgets to use the timer the time can be manually added as well. The care plans are completed at either an office visit or something over the phone. 9