Implementing Strategic Areas for Non-Communicable Disease Prevention
Implementation of national prevention and control programs for non-communicable diseases is crucial for sustainable healthcare systems. Collaborating with multidisciplinary groups and shifting advocacy paradigms towards human rights and social determinants of health are essential. A transformation in healthcare paradigms is needed, focusing on comprehensive care and intersectoral actions. Effective interventions at various levels, from personal health services to global health frameworks, can enhance health system performance and address the challenges posed by NCDs.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Strategic areas for the implementation of national prevention and control programs for non communicable diseases Mauricio Hern ndez Avila National Institute of Public Health, Mexico Washington D.C., June 24, 2013
NCDs Strategic areas All diseases are important, but NCD s if not attended will collapse health systems and countries economies, with important externalities for development We have sufficient evidence that suggest that quantification of suffering is rarely sufficient, on its own to ensure action. Full exploitation of epidemiology & economy potentials will require collaboration of multidisciplinary groups
A shift in the advocacy paradigm is needed to include different perspectives Human rights Social determinants of health Development Universalization of health services Public health legislation Empowerment of the community information + participation
A shift in health care paradigm Prevalent model of care: single visit , medicalized, fragmentized, acute, episodic, curative In Mexico: Physician adjacent to pharmacies Non Communicable diseases Infectious Disease Etiology multifactorial Etiology Single agent Complexity of interventions Complex and in multiple levels Health sector + Intersectoral Complexity of interventions Less complex, vaccines, antibiotics Latency Mostly short Duration of intervention Mostly short Latency long Duration of intervention 20-60 yrars
Interventions for NCDs at different levels of action and influence E f f e c t i v e Personal health services C o v e r a g e Health Sector Improved Health Responsiveness Social and financial Protection Improved efficiency Non-Health Sector Non personal health services: Prevention Information Inter-sectorial Actions: Health in all Policies Healthy physical and social environments Reduce health externalities from public policies The Global Arena Health frameworks and multilateral agreements Transparency Accountability of Multinational Industries Modified from Murray, CL. and Evans, DB. (2003), Health systems performance assessment: Debates, Methods and Empiricism. Geneva:World Health Organization
Building blocks of and the boundaries health systems Inputs and Processes outputs Outcomes Impact Effective coverage Vaccines & Technologies Improved health Medical products, Responsiveness Access Lower Information Governance Workforce Financing prevalence of risk factors and behaviors Social and financial protection Coverage Quality Safety Better health policies & regulation Improved efficiency Leadership Health system performance overview Modified from: Inter-sectorial & inter-institutional healthy policy making Commitment with global agreements Resource allocation Murray, CL. and Evans, DB. (2003), Health systems performance assessment: Debates, Methods and Empiricism. Geneva: World Health Organization Promotion of healthy policies Access to quality preventive public health programs and Non-personal health services MONITORING THE BUILDING BLOCKS OF HEALTH SYSTEMS http://www.who.int/healthinfo/systems/WH O_MBHSS_2010_full_web.pdf Access to quality health care services Personal health services
Building blocks of and the boundaries health systems: addressing smoking Inputs and Processes outputs Outcomes Impact Vaccines & Technologies Fiscal Policy to increase price Anti- smuggling actions Laws for smoke free places and to enact Pictograms Anti-tobacco campaigns Training for the HWF in smoking prevention & nicotine addiction Anti-tobacco campaigns Information system to track process and impact indicators Local research to feed and evaluate policy Clinical guidelines for nicotine addiction NGO s empowered Medical products, Effective national stewardship against tobacco Laws enacted and enforced Cigarette price and tax revenues increase, sales drop Pictograms appear, and move to plain packaging Public places go smoke free Prevalence rates in young and adults drop Good Quality tobacco cessation programs Diseases related to tobacco are reduced (lung cancer, MI..) Medical cost from tobacco attributed diseases are reduced Policy communication: communicate success Land for tobacco-growing is reduced Information Governance Workforce Financing Leadership Inter-sectorial & inter-institutional healthy policy making Commitment with global agreements Resource allocation Non-personal health services Access to Replacement therapy and counseling Personal health services
Life course approach to chronic disease prevention Area of intervention Type of Intervention Mother & Infants Younger people Older People /elders Adults Sectorial Life course area specific interventions Healthy Eating Inter-sectorial Sectorial Non Personal Health Services Active Living Life course area specific interventions Inter-sectorial Sectorial Tobacco Control Life course area specific interventions Inter-sectorial Sectorial Safe Alcohol Use Life course area specific interventions Inter-sectorial Sectorial Mental Health Promotion Life course area specific interventions Inter-sectorial Sectorial Environmental Health Life course area specific interventions Inter-sectorial Integrated sectorial and inter-sectorial approaches based on key settings Non Personal Health Services
Life course approach to chronic disease prevention Area of intervention Type of Intervention Mother & Infants Younger people Older People /elders Adults Sectorial Breast feed promotion Food Labeling Promotion Healthy Eating Inter- sectorial Food Policy (salt+ TFA) Taxation of SB + junk food Labor & Wenviron. Subsidies Sectorial Promotion of physical activity for all ages Active Living Inter- sectorial Urban design Urban design Incentives Security Sectorial Promotion Promotion cessation clinics cessation clinics Tobacco Control Inter- sectorial Legislation, Regulation and healthy fiscal policy Sectorial Health education and health promotion Safe Alcohol Use Inter- sectorial Legislation Drunk Driving prevention Price increase +Taxes
Building blocks of health systems Effective access to HQ personal health care services Effective access to HQ health promotion and risk protection Service delivery Competent work force to respond to personal and non-personal health-care needs Health Work Force Sound and reliable information to enable decision makers at all levels adequate decision making and monitoring and evaluation Information Medical Products, Vaccines and Technologies Essential medical products, vaccines and technologies of assured quality, safety, efficacy and cost-effectiveness, used with quality Personal (clinical and preventive) care services Public health Interventions (risk protection & health promotion) Financing strategic policy frameworks, effective stewardship, regulations, system design, evaluation and accountability Intesectoral influence Leadership Governance
Systemic approach to prevention and control of NTDs, the boundaries of the health system and its building blocks strategic policy frameworks, effective stewardship, regulations, system design, evaluation and accountability Intesectorial influence Leadership Governance Personal health services Human Right's and Social Determinants Public health Law and International multilateral agreements and frameworks Equity NCD policy for the health system Policy for workforce development & training Complicated case with comorbidities Policy for Palliative care Monitoring health system outcomes Established chronic patient control of health perspectives Inter-institutional referral systems Monitoring disease stage at diagnosis Newly Diagnosed Case Monitoring quality of screening process Early detection Health system design for effective health promotion Non personal health services Prevention programs Promotion of healthy life styles and enabling environments Health in all polices Modified from: Don de Savigny and Taghreed Adam (Eds). Systems thinking for health systems strengthening. Alliance for Health Policy and Systems Research, WHO, 2009. & Murray, CL. and Evans, DB. (2003), Health systems performance assessment: Debates, Methods and Empiricism. Geneva: WHO 2003
Systemic approach to prevention and control of NTDs, the boundaries of the health system and its building blocks Effective access to HQ personal health care services Effective access to HQ health promotion and risk protection Service delivery Personal health services Monitoring the status of patients and case fatality Quality palliative care for terminal patients Access to specialized health care personnel and technologies Guidelines for clinical management Complicated case with comorbidities Quality care and control to avoid complications and treatment od comorbidities Research translation Established chronic patient control Newly Diagnosed Case Quality of care indicators Early detection Non personal health services Access to tobacco cessation programs and mutual help groups Physical activity enabling & smoke free environments Prevention programs Promotion of healthy life styles and enabling healthy environments Modified from: Don de Savigny and Taghreed Adam (Eds). Systems thinking for health systems strengthening. Alliance for Health Policy and Systems Research, WHO, 2009. & Murray, CL. and Evans, DB. (2003), Health systems performance assessment: Debates, Methods and Empiricism. Geneva: WHO 2003
Systemic approach to prevention and control of NTDs, the boundaries of the health system and its building blocks Sound and reliable information to enable decision makers at all levels adequate decision making and monitoring and evaluation Information Personal health services Data on health system financing Data on health quality indicators Data on essential medicine prices Complicated case with comorbidities Data on effective coverage Data on health work force Established chronic patient control Registries: cancer, diabetes, Incidence /prevalence reports Newly Diagnosed Case Report the status of population health Early detection Non personal health services Evaluate the success of prevention programs in the population Produce information on population life styles and risk factors Prevention programs Promotion of healthy life styles and enabling healthy environments Modified from: Don de Savigny and Taghreed Adam (Eds). Systems thinking for health systems strengthening. Alliance for Health Policy and Systems Research, WHO, 2009. & Murray, CL. and Evans, DB. (2003), Health systems performance assessment: Debates, Methods and Empiricism. Geneva: WHO 2003
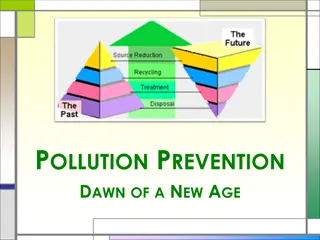
Systemic approach to prevention and control of NTDs, the boundaries of the health system and its building blocks Medical Products, Vaccines and Technologies Essential medical products, vaccines and technologies of assured quality, safety, efficacy and cost-effectiveness, used with quality Personal health services Essential drug list policy Access to new drugs and technologies to treat complication in patients Complicated case with comorbidities Good prescription practices and clinical guidelines Access to new drugs and technologies to prevent complication in patients Established chronic patient control Newly Diagnosed Case Access to better screening tests Systematic screening Non personal health services Medicines to facilitate tobacco use cessation Better food labeling; healthy food in the school environment Prevention programs Promotion of healthy life styles and enabling environments Modified from: Don de Savigny and Taghreed Adam (Eds). Systems thinking for health systems strengthening. Alliance for Health Policy and Systems Research, WHO, 2009. & Murray, CL. and Evans, DB. (2003), Health systems performance assessment: Debates, Methods and Empiricism. Geneva: WHO 2003
SOME EXAMPLES IN TOBACCO CONTROL
Tobacco control strategies: A comparison New York and Mexico City New York Mexico City Coverage (+) Quality (not evaluated) Service delivery Coverage and quality (+++) (e.g coverage and quality) Health Work Force (e.g Algorithms' in Tobacco cessation treatment) Available (+++) No consensous Information Under construction (+) Research (++) Available (+++) (e.g. smoking surveillance system and Research) Medical Products, Vaccines and Technologies (e.g Nicotine subtitutes) Non Available Available (+++) Financing Local and International Resources (+) Local Resources (++++) (e.g campaigns) Political will (++++) Political will (++) Leadership / Governance
Tobacco control policies (federal and local) in NYC, USA
Policy elements Understanding & creating awareness of the problem defining outcomes, stakeholders and role Developing solutions evidence, evaluating options, consultation & working with stakeholders, estimating & managing risks Putting solutions into effect communicating policy, securing budget for implementation & evaluation Testing success and making it stick evaluating & refining & communication
The policy process: Political context Motivate public interest for NCD control Include NCD s within government priorities Policy conflicts that may need to be resolved Stakeholders: involved or neutralized? Political wins in the short time. Who looses? The policy process: Wider Public Context Policy is addressing a national problem Evaluate what are the needs & views of those the policy seeks to influence/affect. Compare with experiences from other countries. Estimate risks and how can they be managed.