Overview of Sexually Transmitted Diseases (STDs): Causes and Laboratory Diagnosis
Sexually transmitted diseases (STDs) encompass a variety of communicable infections transmitted mainly through sexual contact, caused by a diverse range of bacterial, viral, protozoal, and fungal agents. STDs can manifest as genital ulcers, discharge, or systemic symptoms. This article highlights different causative organisms of STDs and provides insights into laboratory diagnosis methods like culture and identification techniques. The content also touches on non-gonococcal urethritis, a condition with symptoms similar to gonorrhea but caused by organisms other than Neisseria gonorrhoeae.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
SEXUALLY TRANSMITTED DISEASES
INTRODUCTION The sexually transmitted diseases (STDs) are a group of communicable diseases which are transmitted predominantly or entirely by sexual contact. The causative organisms include a wide range of bacterial, viral, protozoal and fungal agents. STD may present as genital ulcers, genital discharge without any genital lesion or only as systemic manifestations.
CAUSATIVE ORGANISMS STDs ORGANISMS A. Painless genital ulcers Syphilis Lymphogranuloma venereum (LGV) Dorovanosis Treponema pallidum Chlamydia trachomatis Calymmatobacterium granulomatis B. Painful genital ulcers Chancroid Herpes genitalis Haemophilus ducreyi Herpes simplex viruses (HSV) type 2 and 1 C. Urethral discharge Gonorrhoea Non- gonococcal urethritis (NGU) Neisseria gonorrhoeae Chlamydia trachomatis (types D-K) Mycoplasma genitalium M. hominis
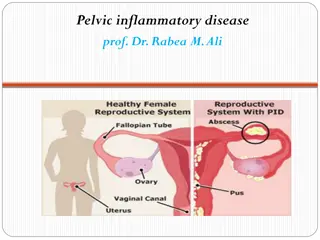
D. Vaginal discharge Gonorrhoea NGU N. Gonorrhoeae C. Trachomatis M. Hominis Trichomonas vaginalis Gardnerella vaginalis Mobiluncus spp. Candida albicans Trichomoniasis Vaginitis Vulvo vaginal candidiasis E. Genital warts Human papilloma viruses F. No genital lesions but only systemic manifestations HIV-1 and HIV-2 Hepatitis B Virus (HBV) Hepatitis C virus (HCV) G. Miscellaneous Group B streptococci Cytomegalovirus Sarcoptes scabei Shigella spp. Campylobacter spp. Giardia lamblia Entamoeba histolytica
LABORATORY DIAGNOSIS A. GONORRHOEA It is caused by Neisseria gonorrhoeae. 1. SPECIMENS 1. Urethral discharge 2. Cervical swab 3. In chronic cases : Discharge after prostatic massage in males 4. Rectal swab 2. Direct Gram staining Intracellular Gram-negative diplococci in smears is diagnostic in males (95% cases). It is sometimes difficult to diagnose gonorrhoea in females on direct Gram staining due to the presence of mixed normal flora.
3. CULTURE 1. Chocolate agar 2. Thayer-Martin medium The inoculated plates are incubated at 37 C for 24-48 hours in the presence of carbon di oxide. 4. IDENTIFICATION Identification of organisms is based on colony morphology, Gram staining from colonies and biochemical reactions. 1. Colony morphology : Translucent colonies are formed. 2. Gram staining : Gram negative diplococci. 3. Biochemical : They are oxidase positive and produce acid from glucose but not lactose, maltose or sucrose.
B. NON-GONOCOCCAL URETHRITIS (NGU) Symptoms of discharge and dysuria clinically indistinguishable from gonorrhoea caused by organisms other than N. gonorrhoeae is called non-gonococcal urethritis (NGU). LABORATORY DIAGNOSIS 1. SPECIMENS i. Swabs from exudate of urethra ii. Cervical discharge 2. DIRECT EXAMINATION (1). GIEMSA STAIN It shows intracytoplasmic inclusion bodies suggestive of C. trachomatis.
(2). DETECTION OF ANTIGEN Smears made from exudate are examined by immunofluorescence test with a monoclonal antibody or by ELISA for detection of elementary bodies of C. trachomatis. 3. CULTURE The exudate is inoculated on McCoy or HeLa cell cultures treated with cycloheximide. Intracytoplasmic glycogen- rich inclusions are detected by Giemsa stain or by immunofluorescence. These are suggestive of C. trachomatis. 4. SEROLOGY 1. Complement fixation test (CFT) 2. Micro-immunofluorescence or ELISA is useful for detection of serovar-specific antibody.
C. SYPHILIS Syphilis is caused by Treponema pallidum. 1. SPECIMENS i. Fluid from chancre ii. Scrapings from ulcerated secondary lesions iii. Blood for serology 2. DIRECT MICROSCOPY T pallidum can be demonstrated in exudate by dark ground microscopy or phase contrast microscopy. Motile organisms may be seen. 3. SEROLOGICAL TESTS (1). NON SPECIFIC TESTS a) VDRL test b) Rapid plasma reagin (RPR) test
(2). SPECIFIC TESTS a) TPHA (Treponema pallidum haemagglutination assay) b) FTA-ABS (Fluorescent treponemal antibody absorption test) c) TPI (Treponema pallidum immobilisation test) VDRL and TPHA are two most commonly used tests. D. CHANCROID Chancroid or soft chancre is caused by H. ducreyi. 1. SPECIMEN Exudate 2. GRAM STAINING Smear shows Gram negative coccobacilli. 3. CULTURE Exudate is cultured onto chocolate agar enriched with isovitalex and foetal calf serum, and containing vancomycin as selective agent. Culture plates are incubated at 35 C under 10% carbon di oxide and high humidity.
4. IDENTIFICATION Colony morphology and Gram staining are useful in identification of the organisms. (1). COLONY MORPHOLOGY H. ducreyi forms small, grey translucent colonies. 2. GRAM STAINING It shows Gram negative coccobacilli. LYMPHOGRANULOMA VENEREUM (LGV) It is caused by C. trachomatis serotypes L1, L2 and L3. 1. SEROLOGICAL TESTS 1. Microimmunofluorescence 2. CFT 2. FREI TEST It is a skin test using LGV antigen and shows delayed type of hypersensitivity.
3. ISOLATION Chlamydiae can be cultivated in variety of cells from chick embryos and mammals. They also grow in yolk sac of eggs. The inclusions in the cell cultures may be stained with Giemsa stain. 4. DIRECT MICROSCOPY Smears of material aspirated from the bubos may show the elementary bodies. The sensitivity of microscopy is very low. F. DONOVANOSIS Donovanosis is caused by Calymmatobacterium granulomatis. 1. SPECIMEN Tissue smear from the ulcer.
2. STAINING Giemsa staining shows Donovan bodies. The Donovan bodies are rounded coccobacilli, 1-2 mm, which lie within cystic spaces in large mononuclear cells. They show bipolar condensation of chromatin, giving a closed safety pin appearance in stained smears. G. HERPES GENITALIS Aetiological agent is Herpes simplex virus (HSV), types 1 and 2 but type 2 strains are more commonly associated. 1. SPECIMENS i. Scrapings from base of the lesions ii. Blood for serology
2. DIRECT MICROSCOPY Giemsa or Wright staining shows characteristic intranuclear inclusions. 3. CULTURE Diagnosis is confirmed by tissue culture in human diploid fibroblast cells. Cytopathogenic effect (CPE) occurs within 24 hours. 4. SEROLOGY Antibody detection by complement fixation test (CFT) is useful in diagnosis of primary infection. H. TRICHOMONIASIS It is caused by Trichomonas vaginalis. 1. SPECIMEN Swab of vaginal discharge is examined freshly. If delay in transport is inevitable, specimen should be collected in stuart s transport medium.
2. DIRECT MICROSCOPY Direct wet film shows motile trichomonads. Direct microscopy is at least 80% as positive as culture. 3. CULTURE Specimen is cultured in Fineberg s medium and incubated for 5 days and examined for motile protozoa. VULVOVAGINAL CANDIDIASIS It is caused by various species of Candida but C. albicans accounts for 80% of cases. 1.SPECIMEN Swab from vaginal secretions. 2. DIRECT MICROSCOPY 1. KOH mount : It shows yeast cells. 2. Gram staining : Characteristic Gram positive budding yeast cells and pseudohyphae may be seen.
3. CULTURE The specimen is inoculated on Sabouraud s dextrose agar (SDA) and incubated at 37 C for 48 hours. 4. IDENTIFICATION i. Colony morphology : Colonies are creamy white and smooth. ii. Gram staining : Gram stained smear shows budding Gram positive yeast cells. iii. Germ tube formation : C. albicans forms germ tube within two hours when incubated in human serum at 37 C. iv. Chlamydospores formation : C. albicans forms chlamydospores on cornmeal agar.
J. GENITAL WARTS Genital warts, also known as condyloma acuminata are common in sexually active adults. These are usually due to human papillomavirus (HPV) types 6 and 11. Cytological or histological examination of cells in urine is used for detection of inclusion bodies of HPV.
Textbook of microbiology by Ananthanarayan and Paniker s. Textbook of microbiology by D. R. Arora and Brij Bala Arora. Textbook of microbiology by Dr. C. P. Baveja. REFERENCE BOOKS