Understanding Rabies: A Comprehensive Overview
Rabies is an acute fatal disease affecting humans and warm-blooded animals, characterized by abnormal behavior, nervous disturbances, excessive salivation, and respiratory paralysis. It claims around 55,000 human lives globally, with efforts in rabies control showing marginal success. The etiology of rabies involves the Lyssa virus, a highly fragile RNA virus belonging to the Rhabdoviridae family. Different serotypes and classifications of the virus exist, with primary reservoirs being foxes, bats, and other animals. Transmission occurs through fresh saliva from rabid animals via bites, scratches, or abrasions.
Uploaded on Jul 23, 2024 | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Veterinary Epidemiology & Zoonoses VPH-321 (Credit Hours-2+1)
Introduction It is an acute fatal disease in man & other warm blooded animals Characterized by: Abnormal behavior, Nervous disturbances such as motor nerve irritability, Mania, An attacking complex, Inability to swallow, Excessive salivation, Impairment of consciousness, Progressive ascending paralysis & Death due to respiratory paralysis
Introduction Rabies claims nearly 55000 human deaths, worldwide Mostly children Presently the efforts at rabies control have enabled a marginal reduction of rabies deaths from 30,000 to 20,000 in India annually
Etiology Lyssa virus Family: Rhabdoviridae RNA virus, Bullet shaped (180 nm X 75 nm in dia.) Highly fragile viruses susceptible to standard disinfectants Sunlight & moderate heat destroy the virus There are 25 viruses in this genus, of which closely related rabies viruses are called Classical rabies viruses
Etiology Serotypes of rabies viruses are: 1. Lagos bat virus, 2. Mokola virus, 3. Duvenhage virus, 4. European bat lyssa virus I (EBL I), 5. European bat lyssa virus II (EBL II) & 6. Australian bat lyssa virus
Etiology Based on antigenicity, the virus is classified as fixed or street rabies virus Sl. No. Fixed rabies virus Street rabies virus 1. The intradermal route in rabbits virus is passaged by serial It is from naturally occurring infection 2. Incubation period is fixed and shorter (6-7 days) Incubation period is variable (11-47 days) 3. It does not produce Negri bodies It (Intracytoplasmic inclusion bodies) produces Negri bodies 4. No shedding of virus in the saliva Shedding of virus in the saliva 5. The virus is not virulent and self- limiting. Used for vaccine production. The virus is virulent and not self- limiting. Pathogenic to warm blooded animals.
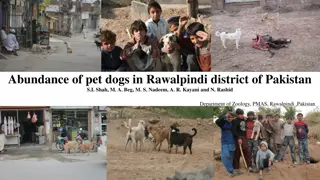
Source & Transmission Worldwide distribution Primary reservoirs: Foxes, bats, raccoons, skunks, dogs, cats & cattle Transmission: From fresh saliva via bite, scratch or abrasion by an rabid animal Rabid dogs shed virus in saliva 5-7 days before showing signs Cat does so for only 3 days before signs Contamination of skin wounds by fresh saliva from infected animals also a source of infection
Disease in animals Central nervous system disturbances The clinical course especially (in dogs) Can be divided into 3 phases: The prodromal form The excitative form The paralytic form Prodromal period: 1-3 days, animals either show signs of paralysis or become vicious
Disease in animals 1. Furious form (changes in behaviour & stage of excitement) Tendency to bite either inanimate/animate objects till death Travel to long distance Shows imaginary catching stance Attempt to lick water but unable to drink water due to the paralysis of pharyngeal& laryngeal muscles Drooling of saliva Photophobia Changes in barking due to paralysis of vocal chords Finally, dropped jaw & tongue will protrude & head will drop down In dogs
Disease in animals 1. In dogs Dump form or paralytic form: Isolated themselves in dark places Paralysis of lower jaw (dropped jaw ), tongue, larynx & hindquarters Not capable to bite 2. In cats Furious form is more common
Disease in animals 3. In cattle Furious form is more common: Violently attack other animals or Attack to inanimate objects, loud bellowing, Incoordination of gait, Excessive salivation, Behavioral changes, Muzzle tremor, Aggression, Sexual excitement, Hyper excitability & Pharyngeal paralysis Paralytic form: Knuckling of hind fetlock, Sagging & swaying of hind quarter while walking, Deviation of tail to one side, Drooling of saliva & yawing movement
Disease in animals In sheep: Hyperexcitability, salivation, vocalization, recumbency, vigorous wool plucking, excessive bleating does not occur but continuous bleating is common & starring of eyes & twitching of lips
Disease in animals In horse: Muscle tremors are frequent & common, pharyngeal paralysis, ataxia & lethargy, Sudden onset of lameness in one limb followed by recumbency & violent head tossing In pigs: Twitching of nose, excessive salivation, chronic convulsion, rapid chewing movement & may walk backward
Disease in human The incubation period: few months (usually 30 to 60 days), Depending on The distance of bite, Severity of bite, Amount of virus inoculated Aggressive status of the rabid animal Infection reaches to CNS symptoms begin to show The infection is effectively untreatable & usually fatal within days Death almost invariably results 2-10 days after first symptoms Drinking cause extremely painful laryngeal spasm Patient refuses to drink (hydrophobia-fear of water) Muscle spasm, laryngospasm & extreme excitability are present
Disease in human Convulsions occur Thick tenacious saliva Increased lacrimation, Frequent micturition Increased perspiration. The initial symptoms of rabies are often mild fever & pain or paresthesia at the wound site Furious rabies is rapidly fatal: hydrophobia or aerophobia, phobia towards sound, hyperactivity and fluctuating consciousness Flaccid paralysis ascending with pain in the affected muscles & mild sensory disturbances will precede death from respiratory paralysis
Classification of exposure based involvement of risk Class I- Slight or negligible risk Licks unbroken skin Scratches without oozing of blood on healthy/ Class II- Definite but moderate risk Consumption of unboiled milk from suspected animals Licks on fresh cuts Scratches with oozing of blood All bites except on head, neck, face, palm and fingers Minor wounds less than five in number Class III- Severe/ grave risk Licks on mucosa Bites on head, Neck, face, palm & fingers Lacerated wounds on any part of the body Bites from wild animals
Diagnosis 1. Sign & symptoms 2. Fluorescent antibody test (FAT) Corneal impression smear, as well as brain Highly specific & rapid test (99.9%) Detects different strains using monoclonal antibody The identifiable strains correlate well with species & geographic distributions observed 3. Identification of Negribodies (intracytoplasmic inclusion bodies) in the brain impression smear by Seller's staining technique 4. Virus isolation from body fluid or brain tissue Negri bodies 5. Molecular techniques
Treatment Post-exposure care to prevent rabies includes: Washing & scrubbing the wound with phenolic soap and/or plenty of running tape water Application of antiseptics Avoiding bandaging or suturing of wound, or point of contact Administering anti-rabies immunizations as soon as possible Anti-rabies vaccine should be given for category II & III exposures (follow post exposure schedule)
Treatment Post exposure schedule If the animal is not previously immunized, Post exposure vaccination on 0-day (the day starts within 24 hours after bite), 3rd, 7th, 14th, 28th & if necessary, on 90th day (Essen's schedule) If the animal is immunized annually 0 day, 3rd and 7th day, put the animal under observation for 10 days If the animal dies, should follow the full regimen (5 doses)
Vaccination Pre-exposure schedule Type of vaccine: Inactivated (from cell culture or embryonated egg vaccine) Number of doses: Three: 0, 7th & 21st or 28th day given by IM or ID route (vaccine should not be given in the gluteal region) Booster: After one year then every five years Contraindication: Severe reaction to previous dose Adverse reactions: Mild local or systemic reactions; rare neuroparalytic reactions reported Special precautions: Do not use animal-brain-derived vaccines
Prevention Postexposure immunization: Upto 50% of human rabies immune globulin is infiltrated around the wound; the rest is administered IM (ERIG or HRIG: anti-rabies antibody) Human Diploid Cell Vaccine (HDCV): 5 injections IM at days 0, 3, 7, 14, & 28 Vaccination of domestic animals Enforced animal control measures (Animal Birth Control and Anti- rabies vaccination programme: ABC-AR) Controlling stray dog population Proper immunization of household dogs (ABC-AR programme) Vaccination of high risk personnel Awareness programme among public

















 undefined
undefined