Understanding the Role of Organ Donation Fellows in Intensive Care Units
Organ Donation Fellows (ODFs) are experienced doctors specializing in deceased organ donation, spending time on the ICU rota and supporting organ donation activities. They assist in donor optimization, communication with families, and organ retrieval, benefiting both ICU patients and the healthcare team. The role offers unique opportunities for research, education, and leadership in the field of organ donation.
- Organ Donation Fellows
- Intensive Care Units
- Deceased Organ Donation
- Healthcare Professionals
- Medical Education
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
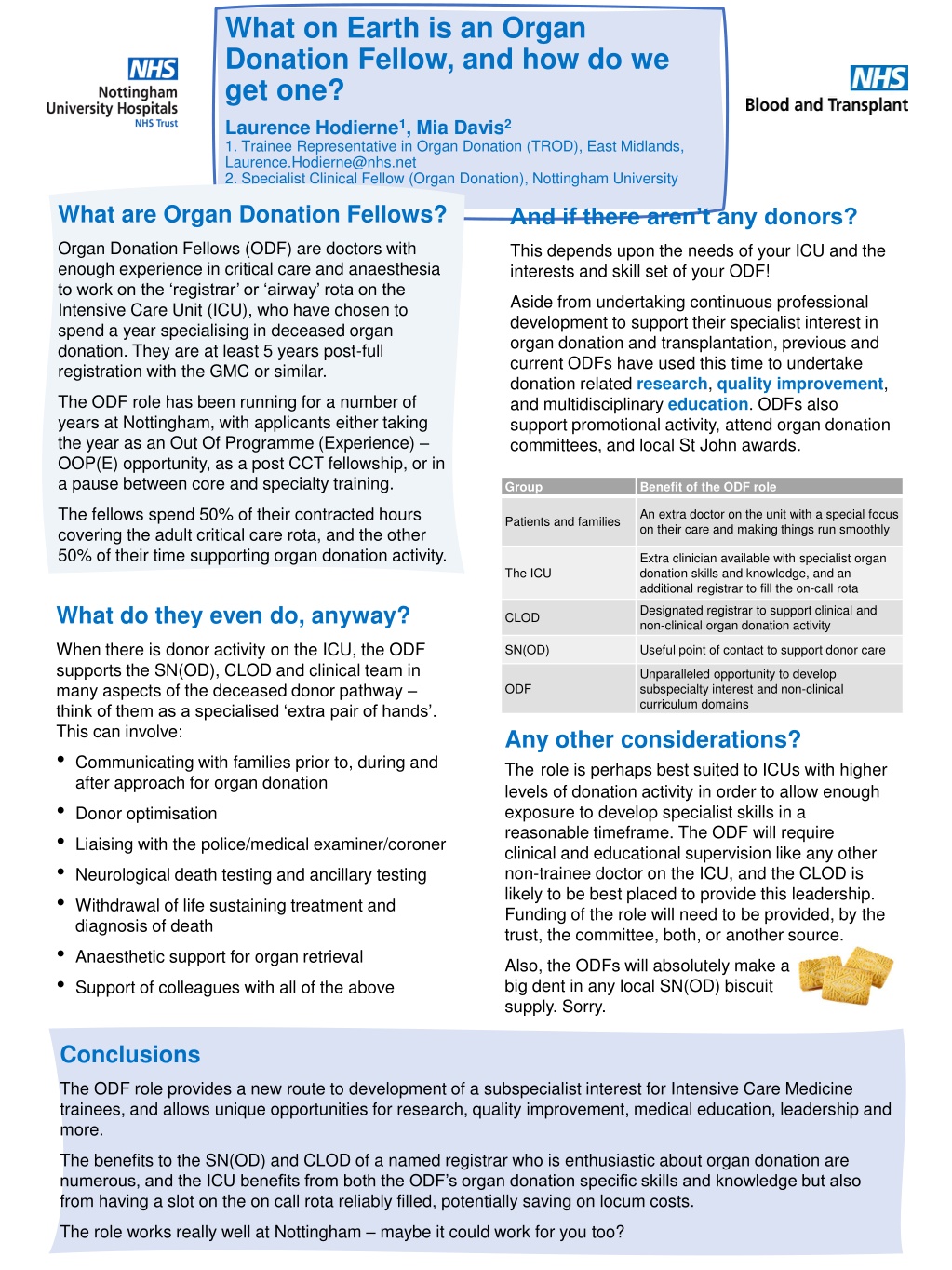
What on Earth is an Organ Donation Fellow, and how do we get one? Laurence Hodierne1, Mia Davis2 1. Trainee Representative in Organ Donation (TROD), East Midlands, Laurence.Hodierne@nhs.net 2. Specialist Clinical Fellow (Organ Donation), Nottingham University Hospitals, Mia.Davis@nhs.net What are Organ Donation Fellows? And if there aren t any donors? Organ Donation Fellows (ODF) are doctors with enough experience in critical care and anaesthesia to work on the registrar or airway rota on the Intensive Care Unit (ICU), who have chosen to spend a year specialising in deceased organ donation. They are at least 5 years post-full registration with the GMC or similar. This depends upon the needs of your ICU and the interests and skill set of your ODF! Aside from undertaking continuous professional development to support their specialist interest in organ donation and transplantation, previous and current ODFs have used this time to undertake donation related research, quality improvement, and multidisciplinary education. ODFs also support promotional activity, attend organ donation committees, and local St John awards. The ODF role has been running for a number of years at Nottingham, with applicants either taking the year as an Out Of Programme (Experience) OOP(E) opportunity, as a post CCT fellowship, or in a pause between core and specialty training. Group Benefit of the ODF role The fellows spend 50% of their contracted hours covering the adult critical care rota, and the other 50% of their time supporting organ donation activity. An extra doctor on the unit with a special focus on their care and making things run smoothly Patients and families Extra clinician available with specialist organ donation skills and knowledge, and an additional registrar to fill the on-call rota The ICU What do they even do, anyway? Designated registrar to support clinical and non-clinical organ donation activity CLOD When there is donor activity on the ICU, the ODF supports the SN(OD), CLOD and clinical team in many aspects of the deceased donor pathway think of them as a specialised extra pair of hands . This can involve: Communicating with families prior to, during and after approach for organ donation Donor optimisation Liaising with the police/medical examiner/coroner Neurological death testing and ancillary testing Withdrawal of life sustaining treatment and diagnosis of death Anaesthetic support for organ retrieval Support of colleagues with all of the above SN(OD) Useful point of contact to support donor care Unparalleled opportunity to develop subspecialty interest and non-clinical curriculum domains ODF Any other considerations? Therole is perhaps best suited to ICUs with higher levels of donation activity in order to allow enough exposure to develop specialist skills in a reasonable timeframe. The ODF will require clinical and educational supervision like any other non-trainee doctor on the ICU, and the CLOD is likely to be best placed to provide this leadership. Funding of the role will need to be provided, by the trust, the committee, both, or another source. Also, the ODFs will absolutely make a big dent in any local SN(OD) biscuit supply. Sorry. Conclusions The ODF role provides a new route to development of a subspecialist interest for Intensive Care Medicine trainees, and allows unique opportunities for research, quality improvement, medical education, leadership and more. The benefits to the SN(OD) and CLOD of a named registrar who is enthusiastic about organ donation are numerous, and the ICU benefits from both the ODF s organ donation specific skills and knowledge but also from having a slot on the on call rota reliably filled, potentially saving on locum costs. The role works really well at Nottingham maybe it could work for you too?
Remote SNOD IT access: A giant leap in safe donor potential screening and characterising. Lynsey Elliss - Specialist Nurse in Organ Donation. Royal Devon University NHS Foundation Trust. Remote IT Access Enhancing our ability to provide safe care. Unexpected Results Once SNODs had remote access it made characterisation safer and easier, as well as reducing inconvenience to the bedside Nurse, improving relationships. By gaining individual remote access to the Trust IT system (MyCare) for all regional SNODs in order to support the safe facilitation of the Donor Characterisation process, a positive unintended consequence has been how this access has allowed SNODs to access key patient data to allow effective potential donor screening remotely. However it also allowed SNODs to log in remotely at the point of referral allowing them to review the patients notes to make accurate mobilisation decisions, with a full clinical picture, allowing the SNOD to screen remotely. Why did we need remote IT access? Within the trust patients are often sent to the local Level 1 for neurosurgical intervention, having remote access to the Trusts system, allows us to review the patients records when they are a patient in another trust, as the Royal Devon University NHS Foundation Trust no longer has any paper notes to request. This also applies to out of Region enquiries from SNODs in other areas, for patients that have moved or are on holiday, allowing us swift and secure access to clinical information. Generic log in access was not available; Clinical Governance within the Trust were not supportive of this model of access due to data breach concerns. SNODs were therefore reliant on using the Bed Side Nurses computer to entirely characterise, this was not always convenient, and caused issues with GDPR compliance, as well as causing concerns with safe characterisation. All medical records are electronic within the Trust and having extremely limited access caused concern during the process. It also allows us to PDA remotely when donor activity is high and embedded time is limited. Recommendations The embedded SNOD liaised with Governance to find a way that they would allow SNODs access, having ruled out generic log ins, individual remote access was suggested. Having remote access has improved safety in screening and characterisation, and also allows SNODs to make informed decisions for mobilisation. Therefore we would recommend other Trusts to enquire if remote access is possible for their SNODs. The Governance Team requested the name of each SNOD, their NMC number and the Trust that they hold their honorary contract with, once the embedded SNOD provided this for each SNOD within the team, a log in and password to MyCare Remote was provided for each SNOD. Allowing them access from their Ipad for both the Royal Devon and Exeter and North Devon District Hospital.
When Two Become One Tate J*, Pearson M*, Gurung S , Hersey P *Specialist Nurse (Organ Donation) Clinical Lead (Organ Donation) South Tyneside and Sunderland NHSFT Opportunities Background Combined, the Trust is now level 2. This recognition of activity has opened opportunities including increased SN-OD resource, and greater research eligibility. In 2019, City Hospitals Sunderland NHSFT merged with South Tyneside NHSFT to form South Tyneside and Sunderland NHSFT. Acute services including emergency medicine and level 3 critical care have been maintained on both sites. The pool of potential group members has increased, allowing vacant positions to be more easily filled. In terms of donation activity, Sunderland was a level 3 trust, and South Tyneside level 4. The merger was opportunity to start again , considering the strengths of the legacy groups. Merging Trust Organ Donation Activity Top Tips Chase the money each group will have it s own historical budget, potentially with different flows aligning these early is important. Each legacy Trust had their own organ donation group, SN-OD and CL-OD. We have merged to a single organ donation group and produced trust-level policies and standard operating procedures. Identify the issues that a single site has found historically difficult the merger may provide a quick win . Keep your enthusiastic members but look critically at existing arrangements and practices. Challenges Utilise any economies of scale but also identify any opportunities that size can bring. Cultural norms needed a new normal as the group formed, with a willingness to adapt. In the early stages of the merger there was role duplication (site specific roles), risking an unwieldy group and maintenance of single site solutions. The needs of each site need to be remembered donation potential, staffing, geography etc differs between sites so solutions must be applicable to both.