Understanding Coma, Brain Death, and the Examination Process
Exploring the definitions of coma and altered consciousness, understanding brain death examinations, criteria for determining brain death, who can perform the exam, Texas law on the definition of death, and components of a brain death exam. Learn about different states of altered consciousness, the importance of irreversible causes, and the detailed procedures involved in examining brain death.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Coma and Brain Death
Objectives O Define Coma and altered consciousness O Understand the brain death exam
Altered Level of Consciousness O Coma: unconscious state O Does not respond to stimuli appropriately O Eyes closed, no purposeful motor response, no language comprehension or expression O Vegetative State: Must meet all 3 criteria O No purposeful voluntary responses O No evidence of language comprehension O Sleep/wake cycles are apparent eyes open, unable to interact with environment O Minimally conscious state: 1 or more O Can follow simple commands O Yes/no gestures even if not accurate O Verbalizes O Appropriate response to external stimuli: tracking, smiling, reaching for things
When can you determine brain death? O Irreversible cause of coma O Rule out other reasons for unresponsiveness O Ensure patient is: O Normothermic O Normotensive (even if on pressors) O Has normal electrolytes O Not on any drugs that could cause coma
Who can perform a brain death exam? O Any 2 physicians, not from the same team O Different laws for different states O Texas requires 2 exams 6 hours apart
Texas Law: Definition of Death O (a) A person is dead when, according to ordinary standards of medical practice, there is irreversible cessation of the person's spontaneous respiratory and circulatory functions. (b) If artificial means of support preclude a determination that a person's spontaneous respiratory and circulatory functions have ceased, the person is dead when, in the announced opinion of a physician, according to ordinary standards of medical practice, there is irreversible cessation of all spontaneous brain function. Death occurs when the relevant functions cease. (c) Death must be pronounced before artificial means of supporting a person's respiratory and circulatory functions are terminated.
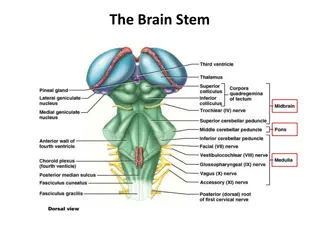
Components of Brain Death Exam O Assessment of cranial nerve brain stem function O Assessment of any level of responsiveness O Response to noxious stimulation O Apnea OR (if patient too unstable for apnea test) confirmatory test O Nuclear flow study O TCD s O EEG O Cerebral angiography
Steps of the brain death exam O Pupils not reactive to light (CNII and III) O Pupils usually between 4-9mm; pinpoint pupils not associated with brain death O No corneal reflex (CNV and VII) O Oculocephalic and oculovestibular reflex absent (CN III, VI, VIII) O Oculocephalic = doll s eyes. Cannot do if c-spine not cleared O Oculovestibular = no eye deviation. Use 50 ml cold water/saline and watch on each side for 1 minute
Steps of brain death exam O No facial movement to noxious stim (CN V, VII) O Noxious stim should be central pain (stim above nipples, TMJ, supraorbital) O No cough or gag (CN IX and X)
What can confound your exam? O Pupillary response can be altered by: eye trauma, scopolamine, atropine O Oculovestibular response can altered by: TM disruption, disease of inner ear, anticholinergic drugs O Cases of viper envenomations causing brain dead like state d/t coma and ophthalmoplegia
Apnea Test O Pre-oxygenate patient O Get baseline ABG try to normalize PCO2as much as possible prior to apnea test O Place cut nasal cannula down ETT during test O One person needs to time the test not the physicians performing test O Pressors can be titrated during test O Stop test if: SBP cannot be maintained >90 or sats <90% O Goal: PCO2>60mmHg or 20mmHg rise over pretest PCO2
Neurologic Exam O Apnea test: O Prerequisites: normotensive, normothermia, eucapnia, normoxia O Patient should be preoxygenated for at least 10 minutes O Check PCO2 prior to test O Remove patient from ventilator, supply O2 and watch for breathing for 8-10 minutes O Stop test if sats <85% or SBP <90 O Can use a t-piece with CPAP O PCO2 >60 or 20mmHg above starting point O Inconclusive tests can be repeated
Brain Death O Ancillary Tests: EEG, CTA, MRA O Not necessary O Used if apnea test unable to be done O In lieu of repeat exam O Documentation: time of death O Time when POC2 reached target level O Time when ancillary test results reported O TOSA required to be contacted once brain death confirmed EEG, angio angio, nuclear scan, TCD , nuclear scan, TCD,
Can patients move when thy are brain dead? O One study showed up to 55% of patients have movements when brain dead O Movements such as: O Spinal reflexes causing movement of limbs other then posturing O Sweating, flushing O DTR s O Breathing-like movements