The Importance of Glycogen in Providing a Constant Source of Blood Glucose
Glycogen serves as a crucial storage form of glucose in the body, ensuring a constant source of blood glucose crucial for brain function, RBC energy, and muscle fuel. This storage form is essential for providing glucose during times of fasting or increased energy demands, with glycogen synthesis and breakdown tightly regulated by hormones. Muscles and the liver are the main storage sites, each playing a unique role in maintaining blood glucose levels and energy reserves. Glycogen is composed of branched-chain molecules of glucose, with its synthesis and degradation crucial for meeting the body's energy needs.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
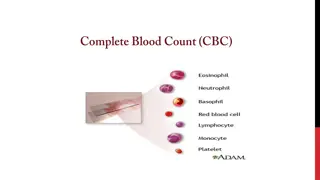
A constant source of blood glucose is an absolute requirement for human life. Glucose is the greatly preferred energy source for the brain, and the required energy source for RBC and muscle, since it s the substrate for anaerobic glycolysis. Blood glucose can be obtained from three primary sources: the diet, degradation of glycogen, and gluconeogenesis. Dietary intake of glucose and glucose precursors, is sporadic and, depending on the diet, is not always a reliable source of blood glucose. In contrast, gluconeogenesis can provide sustained synthesis of glucose, but it is somewhat slow in responding to a falling blood glucose level. Therefore, the body has developed mechanisms for storing a supply of glucose in a rapidly mobilizable form, namely, glycogen.
In the absence of a dietary source of glucose, this sugar is rapidly released from liver and kidney glycogen. Similarly, muscle glycogen is extensively degraded in exercising muscle to provide that tissue with an important energy source. When glycogen stores are depleted, specific tissues synthesize glucose de novo, using amino acids from the body s proteins as a primary source of carbons for the gluconeogenic pathway.
The main stores of glycogen in the body are found in skeletal muscle and liver. The function of muscle glycogen is to serve as a fuel reserve for the synthesis of ATP during muscle contraction. That of liver glycogen is to maintain the blood glucose concentration, particularly during the early stages of a fast. Amounts of liver and muscle glycogen Approximately 400 g of glycogen make up 1 2% of the fresh weight of resting muscle, and approximately 100 g of glycogen make up to 10% of the fresh weight of a well-fed adult liver. What limits the production of glycogen at these levels is not clear.
Glycogen polysaccharide from -D-glucose. The primary glycosidic bond is an (1 4) linkage. After an average of eight to ten glucosyl residues, there is a branch containing an (1 6) linkage. These molecules exist in discrete cytoplasmic granules contain most necessary for glycogen synthesis and degradation is a made branched-chain exclusively that enzymes also of the
Glycogen is the storage form of glucose. The synthesis and degradation of glycogen are carefully regulated so that sufficient glucose is available for the body s energy needs. Both glycogenesis primarily by three hormones: 1. Insulin 2. Glucagon 3. Epinephrine. and glycogenolysis are controlled
Glycogenesis Stores glucose by converting glucose to glycogen. Operates when high levels of glucose-6-phosphate are formed in the first reaction of glycolysis. Does not operate when energy stores (glycogen) are full, which means that additional glucose is converted to body fat. Glycogen is synthesized from molecules of -D-glucose. The process occurs in the cytosol, and requires energy supplied by ATP (for the phosphorylation of glucose) and uridine triphosphate (UTP). 9
The degradative pathway that mobilizes stored glycogen in liver and skeletal muscle is not a reversal of the synthetic reactions. Instead, a separate set of cytosolic enzymes is required. When glycogen is degraded, the primary product is glucose 1-phosphate, obtained by breaking (1 4) glycosidic bonds. In addition, free glucose is released from each (1 6)-linked glucosyl residue. Is activated by glucagon at low blood glucose levels
Glucose is the primary energy source for the brain, skeletal muscle, and red blood cells. Deficiency can impair the brain and nervous system. 15
Gluconeogenesis: Glucose Synthesis Gluconeogenesis is a metabolic pathway that results in the generation of glucose from non-carbohydrate carbon substrates such as lactate, glycerol, and glucogenic amino acids. The vast majority of gluconeogenesis takes place in the liver and, to a smaller extent, in the cortex of kidneys. This process occurs during periods of prolonged fasting, starvation, or intense exercise and is highly endergonic. Gluconeogenesis is often associated with ketosis.
Gluconeogenesis and Glycolysis In gluconeogenesis, which occurs when blood sugar levels are low and liver glycogen is depleted, 7 of the 10 reactions of glycolysis are reversed. Three irreversible glycolytic reactions are bypassed by alternative reactions. The major substrates for gluconeogenesis are certain amino acids (derived from muscle), lactate (formed in muscle and red blood cells), and glycerol (produced from the degradation of triacylglycerols). In contrast to the reactions of glycolysis, which occur only in cytoplasm, the gluconeogenesis reactions catalyzed by pyruvate carboxylase and, in some species, PEP carboxykinase occur within the mitochondria. The reaction catalyzed by glucose-6-phosphatase takes place in the endoplasmic reticulum. Note that gluconeogenesis and glycolysis do not occur simultaneously. In glycolysis, pyruvate is converted either to acetyl-CoA (not shown) or to lactate.
Gluconeogenic precursors are molecules that can be used to produce a net synthesis of glucose. They include intermediates of glycolysis and the tricarboxylic acid (TCA) cycle. Glycerol, lactate, and the -keto acids obtained from the transamination of glucogenic amino acids are the most important gluconeogenic precursors.
Glycerol is released during the hydrolysis of triacylglycerols in adipose tissue , and is delivered by the blood to the liver. Glycerol is phosphorylated by glycerol kinase to glycerol phosphate, which is oxidized by glycerol phosphate dehydrogenase to dihydroxy acetone phosphate an intermediate of glycolysis. Note: Adipocytes cannot phosphorylate glycerol because they essentially lack glycerol kinase.
Lactate is released into the blood by exercising skeletal muscle, and by cells that lack mitochondria, such as red blood cells. In the Cori cycle, bloodborne converted by exercising muscle to lactate, which diffuses into the blood. This lactate is taken up by the liver and reconverted to glucose, which is released back into the circulation . glucose is
C. Amino acids Amino acids derived from hydrolysis of tissue proteins are the major sources of glucose during a fast. -Ketoacids, such as -ketoglutarate, are derived from the metabolism of glucogenic amino acids. These -ketoacids can enter the TCA cycle and form oxaloacetate (OAA), a direct precursor of phosphoenolpyruvate (PEP). Note: Acetyl coenzyme A (CoA) and compounds that give rise only to acetyl CoA (for example, acetoacetate and amino acids such as lysine and leucine) cannot give rise to a net synthesis of glucose. This is due to the irreversible nature of the pyruvate dehydrogenase reaction, which converts pyruvate to acetyl CoA. These compounds give rise instead to ketone bodies and are therefore termed ketogenic.
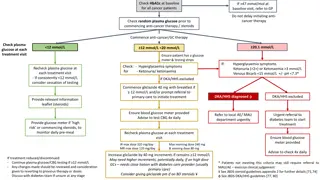
Regulation of Glycolysis and Gluconeogenesis Regulation occurs as: High glucose levels and insulin production promote glycolysis. Low glucose levels and glucagon production promote gluconeogenesis. 24
The pentose phosphate pathway is an alternative metabolic pathway for glucose oxidation in which no ATP is generated. Its principal products are NADPH, a reducing agent required in several anabolic processes, and ribose-5-phosphate, a structural component of nucleotides and nucleic acids. The pentose phosphate pathway occurs in the cytoplasm in two phases: oxidative and nonoxidative. In the oxidative phase of the pathway, the conversion of glucose-6-phosphate to ribulose-5-phosphate is accompanied by the production of two molecules of NADPH. The nonoxidative phase involves the isomerization and condensation of a number of different sugar molecules. Three intermediates in this process that are useful in other pathways are ribose-5-phosphate, fructose-6-phosphate, and glyceraldehyde-3- phosphate
The pentose phosphate pathway (hexose monophosphate shunt) is a more complex pathway than glycolysis . Three molecules of glucose 6-phosphate give rise to three molecules of CO2 and three 5-carbon sugars. These are rearranged to regenerate two molecules of glucose 6- phosphate and one molecule of the glycolytic intermediate, glyceraldehyde 3-phosphate. Since two molecules of glyceraldehyde 3-phosphate can regenerate glucose 6-phosphate, the pathway can account for the complete oxidation of glucose.