Leadership and Rules
Formal leadership plays a crucial role in successful Restraint Reduction Projects by prioritizing the reduction, developing plans, removing barriers, allocating resources, and ensuring accountability. On the other hand, informal leadership influences peers and supervisors to model desired behaviors and practices in healthcare settings. The use of person-first language and awareness of unwritten and blanket rules further contribute to creating a respectful and person-centered environment in healthcare organizations.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
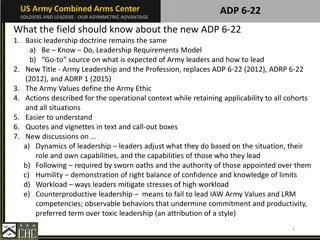
Formal leadership Is the most important component in successful Restraint Reduction Projects. Only formal leaders have the authority to make the changes that are necessary for success to: Make Restraint Reduction a high priority. Assure for Reduction Plan Development. Reduce/eliminate organisational barriers, including changing policy and procedures. Provide or re-allocate the necessary resources. Hold people accountable for their actions.
Informal leadership Experience doesn t necessarily mean you are right. Opinions are not fact, just opinions. The power of a leader to influence others can have a negative impact e.g. Attitude, language, overriding decisions, unwritten rules. We all have power and influence. Assumed authority Can be a member of the team you look up to or commands authority and it doesn t have to be the nurse in charge it could be any member of the team. Rules created from individuals, teams within teams, incidents. Incidents can happen in another part of the trust but a blanket rule is created so everyone then as to follows it. Habits can arise on a ward and suddenly a new rule is created ( no toast after 9am) and the years tick by and the rule is never challenged except usually by new staff. Who might be told when they don t follow the rule, oh, we don t do that on here .
Informal leadership All organisations have informal leaders who have their own power (influence with peers or supervisors). Informal leaders can use their influence in very important ways: To model consumer- directed care. To model compassion, respect and listening skills. To provide feedback to colleagues on good and not so good practices. To make suggestions to supervisors. Think about those in your career who you have looked up to, appreciated and wanted to model.
Person first language Chosen language to use for recovery-orientated systems of care. A major change/shift from usual language. Is culturally competent, respectful and person-centred. Based on linguistic philosophy, e.g. how we speak about something is indicative of how we value and treat it . (IAPSRS, 2003) What are some of the words you hear in nursing office, handovers and patient areas?
Unwritten rules Locked and unlocked doors Access to refreshments Access to phone Patients going into other patients rooms Visitors rules Delegation of tasks You are it. Dealing with other wards/teams/professionals Lock down
Blanket rules Smoking rules. Eating with patients. Patients not allowed in Nursing office. Patients not allowed in activity room. Removal of articles of clothing
Unwritten rules PDSA This exercise should throw up A number of potential PDSA s. Get your teams to think about what unwritten rules exist on your ward. The rules to be tweaked You will need to be clear On what the tweak/change is and Then test it. Put up a flip chart on office wall and ask staff over a 2 week period to put up the rules they see (including their own) The binned rules you might Want to monitor what happens When rule isn t in place. Use a community meeting to ask patient to list the rules they see and how they make them feel. What value do they see in the rule/s Collate all rules and in a team mtg discuss each rule and how staff feel/value it then allocate each rule to either a keeper, a tweaker or a binner. Once completed ask the patients to do the same exercise.
Note Some rules everyone hates but that doesn t mean they should be binned. When deciding on what to do with the rule have a set of criteria that they the rule must meet e.g. 1. That it ensures the safety and security of everyone. 2. That it has value. 3. That it aligns to policy and guidance (Trust and national). 4. It s least restrictive 5. Its fair and equitable