Clinical Validation in Acute Respiratory Failure Case Study
Clinical validation plays a crucial role in ensuring accurate diagnosis and treatment for patients, particularly in cases like acute respiratory failure. This case study highlights the importance of thorough documentation review, collaboration with healthcare team members, and effective validation queries to clarify the accuracy of diagnoses. With detailed clinical data and criteria sets, healthcare professionals can make informed decisions to provide optimal care for patients.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Quick Study - Clinical Validation Presented to the WA and OR State ACDIS Chapters 4/6/2018 Cathy Farraher, RN, BSN, MBA, CCM, CCDS CDI specialist Newton-Wellesley Hospital Farraher has a broad experiential base, from defending RAC auditors, Legal Nurse Consulting, many years of Case Management Consulting, Off-Shift Nurse Management as well as hands on ICU, oncology/BMT and telemetry nursing at Brigham and Women s Hospital prior to embarking on her CDI career. She has presented to various groups over the years, including medical and surgical physicians, ACDIS and AHIMA members, and other practitioners. She is the former Co-Lead of the successfully renewed MA ACDIS Chapter, and is currently the Chair Elect of the ACDIS National Practice Guidelines Committee. She is also the author of CDI Mail: Ongoing Physician Training, available through HCPro. 1
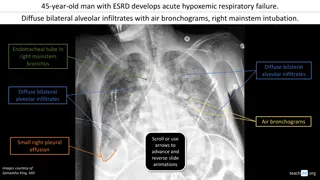
Respiratory Failure Case Study Acute Respiratory Failure is documented in a chart with the following clinical data . Patient presented to the ED with SOB, DOE and was noted to have PMH of CHF and 2+ Bil LEE. Sating 90 on RA but recovered quickly with 2L NC and 20 IV Lasix . Review of systems notes WNL under respiratory. Nursing notes are scant, no respiratory therapy notes and no other respiratory treatments are documented. Acute Respiratory Failure is noted in the ED Report. 2
What Do you Do? Consider the impact of the notes as if you were the nurse caring for the patient . If no hospital approved criteria set, go with your instincts considering your clinical experience, and if unsure, collaborate with a co-worker, manager, or PA. Consider a verbal query if the physician documenting is likely to misinterpret a written one. Make every attempt to query the actual provider who is responsible for having documented what you believe is an erroneous diagnosis. 3
Example of a Validation Query Please clarify the accuracy of the diagnosis acute respiratory failure as documented in the ED Report of this CHF patient with an SpO2 of 90% on admission. The patient received a maximum of 2L of oxygen during the admission, as well as some IV lasix. The Review of Systems includes documentation of the respiratory system WNL and he is noted to be resting comfortably . No other clinical indicators or treatment are noted by my review. The acute respiratory failure was: Confirmed (please include additional indicators and/or treatments) Ruled out Other diagnosis Unable to determine 4
Acute Respiratory Failure: Example of a Criteria Set Visible tachypnea or wheezing Inability to speak full sentences Use of accessory muscles Cyanosis Grunting Nasal flaring Pursed lip breathing Elevated respiratory rate Blood Gas Abnormality: PaO2 < 60 pH < 7.32 PaCo2 > 50 mm Hg Sats < 90% A change in PO2/PCO2 by 10-15 mm from baseline Treatments: Oxygen > 40% via face mask, non-rebreather, NC (5L= 40%) Significant increase in oxygen usage from baseline Respiratory treatments Mechanical Ventilation Mechanical Assist ie. CPAP, BiPAP 5
Post Operative Pulmonary Insufficiency Example of Developing a Criteria Set Patient remains on the vent, in the ICU, on high flow O2 etc. for longer than what would normally be expected due to a pre-existing underlying pulmonary issue ie; COPD, asthma, ILD Clearly defined time frames should be established to promote consistency with providers and CDI specialists 6
Post-op Pulmonary Insufficiency Case Study Mr. Jones was sent to the Thoracic ICU for further monitoring post operatively s/p his THA. He was extubated without incident at 6 am and will transfer to the floor. 1) POD 1 total hip arthroplasty 2) Post op Pulmonary insufficiency, Resolved 3) Chronic Respiratory Failure on home O2 4) COPD 7
Example of a Validation Query Post Operative Pulmonary Insufficiency was documented in your 2/17 PN. He was noted to be extubated approximately 5 hours s/p transfer from the OR directly to the ICU and weaned quickly to his baseline O2 rate of 2L NC. Please provide your clinical opinion of the following options: Post Operative Pulmonary Insufficiency is a valid diagnosis. (Please provide additional clinical indicators to support this) Post Operative Pulmonary Insufficiency was Ruled Out Other 8
Malnutrition Case Study Patient with a BMI of 19.3 that according to nursing notes has been skinny all my life and just can t seem to gain weight no matter what I eat . No documentation in the chart supports the moderate malnutrition diagnosis in the H+P. No treatments or consults are ordered, and the patient is on a Regular Diet. ___________________________________________ Her roommate has a BMI of 29, but has had a 15% weight loss over the last 4 months 2/2 dysphasia. She is being worked up for malignancy and is NPO for g-tube placement in the AM. 9
Malnutrition: Example of a Criteria Set Moderate Protein Calorie Malnutrition Acute or Chronic Illness/ Injury or Social Condition with <75% of recommended intake for at least 1 week combined with : mild wasting of muscle, subcutaneous fat and/or fluid accumulation AND unintentional wt loss of 1-2%-week, 5%-month, 7.5 %-3 months, 10%-6 months or 20%- year. Unspecified Severe Protein Calorie Malnutrition Acute or Chronic Illness/ Injury or Social Condition with <50% of recommended intake for at least 5 days combined with : Moderate/severe wasting of muscle, subcutaneous fat and/or fluid accumulation AND unintentional wt loss of >2%-week, >5%-month, >7.5 %-3 months, >10%-6 months or> 20%- year. Treatment: Nutritional Supplements Strict I+O Diet changes TPN/Tube Feeds Calorie Counts Medications 10
Example of a Validation Query Moderate malnutrition is documented in your H+P for this inpatient stay. No additional clinical indicators or treatment can be found by my review to support this as a billable code. Please clarify if: Moderate malnutrition was documented in error Moderate malnutrition was ruled out/resolved prior to this admission Moderate malnutrition is a valid diagnosis and can be further supported by ___________ Other 11
Encephalopathy Case Study 12/3 RN note Mrs. Smith is a 79 year old patient with Alzheimer s from Newbridge Nursing Home (long term patient) here after an unwitnessed fall. VSS. A+Ox1. Her daughter says her MS is the same it always is and she is only concerned about some grimacing she noticed when her mother tried to move her left arm. Pt to X-ray and awaiting results. Tylenol given. 12
Example of a Validation Query Mrs. Smith was noted have Alzheimer s dementia at baseline and her daughter informed the ED RN that her mental status was the same it always is per the 12/3 RN note. Encephalopathy was documented by your resident, Dr. Cool in the H+P. Do you Agree with the diagnosis of Encephalopathy? Disagree with the diagnosis of Encephalopathy? Other comments for the coding department? 13
Encephalopathy Example of a Criteria Set Alteration in all brain functioning (communication, memory, speech, orientation, behavior) due to a systemic underlying cause that is typically reversible. Acute (or subacute) and will resolve when the underlying cause is corrected Toxic encephalopathy- effects of drugs, toxins, poisons and medications. Metabolic- due to fever, dehydration, electrolyte imbalance, acidosis, infection and organ failure. Toxic-metabolic -a combination of toxic and metabolic effects. Septic encephalopathy due to severe sepsis. Uremic and hepatic encephalopathies- due to renal and hepatic failure Treatments: 1:1 observation Medications Physical/chemical restraint 14
Acute Kidney Injury (AKI) Case Study Bob Ratchet here with complaints of feeling weak, poor PO and was noted to have hyponatremia, dehydration and Acute Kidney Injury (AKI) in the ED note. Creatinine 2.3, GFR 36 H+P later noted CKD stage 3B with a baseline creatinine of 2.0. 15
Example of a Validation Query Acute Kidney Injury was noted in the ED note. H+P noted baseline creatinine of 2.0 with CKD Is the Acute Kidney Injury: Ruled Out? Resolved? A Current Diagnosis? 16
Acute Renal Failure/Acute Kidney Injury RIFLE criteria Class GFR UO SCr 1.5 or GFR >25% Risk <0.5 mL/kg/h 6 h Injury SCr 2 or GFR >50% <0.5 mL/kg/h 12 h SCr 3 or GFR >75% or if baseline SCr 353.6 mol/L( 4 mg/dL) SCr >44.2 mol/L(>0.5 mg/dL) <0.3 mL/kg/h 24 h or anuria 12 h Failure Complete loss of kidney function >4 weeks Loss of kidney function Complete loss of kidney function >3 months End-stage kidney disease 17
Acute Kidney Injury The KDIGO guidelines Increase in serum creatinine by 0.3 mg/dL ( 26.5 micromol/L) within 48 hours, or Increase in serum creatinine to 1.5 times baseline, which is known or presumed to have occurred within the prior seven days, or Urine volume <0.5 mL/kg/hour for six hours https://www.uptodate.com/contents/definition-and-staging-criteria-of-acute-kidney-injury-in-adults 18
Facility Policy vs Ethical Quandaries Query policies or lack thereof Finance overseeing program Lack of experienced management oversight Consultants driving decision making Physician Advisors becoming more invested (can be good or bad) 19
Developing a Compliant Process It is a healthcare organization s due diligence to confirm the clinical validity of a diagnosis that meets UHDDS criteria as an other diagnosis before it is included as claims data If a diagnosis does not appear to be supported in the health record then a clinical validation query should be submitted. The query should be constructed to comply with current industry guidance The query should make the case through weak clinical indicators why the diagnosis does not appear to be clinical validated 20
Organizational Policies Question: Coding Clinic, Fourth Quarter 2016, page 149, states "A facility may require that a physician use a particular clinical definition or set of criteria when establishing a diagnosis". Would it be appropriate for facilities to develop a policy to omit a diagnosis code based on the provider's documentation not meeting established criteria? ICD-10-CM/PCS Coding Clinic, Fourth Quarter ICD-10 2017 Page: 110 Effective with discharges: October 1, 2017 21
Organizational Policies Response: No. It is not appropriate to develop internal policies to omit codes automatically when the documentation does not meet a particular clinical definition or diagnostic criteria. Facilities may review documentation to clinically validate diagnoses and develop policies for querying the provider for clarification to confirm a diagnosis that may not meet particular criteria. ICD-10-CM/PCS Coding Clinic, Fourth Quarter ICD-10 2017 Page: 110 Effective with discharges: October 1, 2017 22
Organizational Policies Response Continued: Facilities should also work with their medical staff to ensure conditions are appropriately diagnosed and documented. If after querying, the attending physician affirms that a patient has a particular condition in spite of certain clinical parameters not being met, the facility should request the physician document the clinical rationale and be prepared to defend the condition if challenged in an audit. The facility should assign the appropriate code(s) for the conditions documented. ICD-10-CM/PCS Coding Clinic, Fourth Quarter ICD-10 2017 Page: 110 Effective with discharges: October 1, 2017 23
Clinical Validation Query Reconciliation Basically, coders can t decide not to code a reportable diagnosis because it doesn t meet specified criteria The provider must be queried and clarify if the documented diagnosis was ruled out to avoid reporting of the condition IF UHDDS criteria are met 24
Clinical Validation Query Reconciliation If the provider confirms the diagnosis then it should be coded Keep in mind Coding Clinic states the facility should request the provider document the clinical condition, but also keep in mind that providers are not required to provide additional documentation Organizations would be well served to keep all clinical validation queries, even if the provider failed to respond to the query, to demonstrate their due diligence in attempting to clinically validate a diagnosis ICD-10-CM/PCS Coding Clinic, Fourth Quarter ICD-10 2017 Page: 110 Effective with discharges: October 1, 2017 25
Compliance vs. Gaming Accurate reflection of severity of illness Allows for accurate trending and data mining Accurate facility scoring for consumer comparison The right thing to do Documentation of key diagnoses without supporting data High risk for denials Increased provider frustration Non-compliant 26
Handling Different Opinions You are the professional ultimately responsible for determining the need for a query. What if validation queries are not allowed , discouraged, or otherwise frowned upon? Having a hospital policy, administrative support, hospital approved diagnostic criteria sets make this less of an issue, and is highly encouraged. 27
Coding Corner, July 2017, Postprocedural respiratory failure, Richard Pinson, MD For many years, the documentation of post-op respiratory failure or pulmonary insufficiency in patients who require a routine period of mechanical ventilation, even when no pulmonary problem or complication is present, has been a common practice to identify a condition that would support billing of critical care services. However, CMS and other payers frown upon documentation of a condition that a patient really doesn't have, meaning that this traditional practice raises compliance risks. 28
Questions? Happy Friday 29