Comprehensive Guidelines for Hypertension Management in Canada 2020
The Hypertension Canada's 2020 Comprehensive Guidelines provide insights on prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. The guidelines emphasize standardized blood pressure measurement, risk factors, and the use of out-of-office monitoring for accurate diagnosis. In Canada, approximately 23% of adults have hypertension, making it a prevalent risk factor for cardiovascular disease. These guidelines aim to improve the management of hypertension and reduce associated health risks among the Canadian population.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Hypertension Canadas 2020 Hypertension Canada s 2020 Comprehensive Guidelines Comprehensive Guidelines Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension
Seven Hypertension Sections 2020 1. Measurement and Diagnosis 2. CV Health Promotion 3. Management: Uncomplicated 4. Management: Complex Comorbidities 5. Resistant Hypertension 7. Special Populations 6. Care Delivery Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
1. Measurement and Diagnosis 1. Measurement and Diagnosis
Key Messages 1. Hypertension remains the most prevalent risk factor for cardiovascular disease in Canada 2. Standardized BP measurement, using validated protocols and devices, continues to be recommended to screen for cases of hypertension 3. Frequency and timing of screening can be tailored to each patient s risk of hypertension. Common risk factors for hypertension include: e: Diabetes mellitus Chronic kidney disease Low level of consumption of fresh fruits and vegetables Sedentary behaviour Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Key Messages 4. Use of out-of-office measurement (24-hour ambulatory BP monitoring [ABPM] or home BP monitoring [HBPM]) is recommended for all adults with: High in-office BP to rule out white coat hypertension Suspected hypertension (including adults with diabetes) to rule out masked hypertension Adults with confirmed diagnosis of hypertension should have a baseline assessment of: Cardiovascular risk factors (including screening for diabetes, hyperlipidemia, and renal disease); Target organ damage Routine lab testing. The possibility of pregnancy should be considered in all women of reproductive age with a new diagnosis of hypertension, and during follow-up visits 5. 6. Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Hypertension in Canada Almost 1 in 4 Canadian Adults have Hypertension Approximately 23% of Canadian adults have hypertension More prescriptions for hypertension than for any other medical disorder 4 million prescriptions every month in Canada Cost of hypertension approaches 10% of all health care spending In 2010, hypertension cost the Canadian health care system over 13 billion dollars annually Robitaille C, et al. CMAJ 2012;184:E49-56. Morgan S. Med Care 2004;42:635-42. Campbell NR, et al.. J Hypertens 2003;21: 1591-7. World Health Organization. 2008-2013 action plan for global strategy for the prevention and control of noncommunicable diseases, 2008. Available at: http://www.who.int/nmh/publications/9789241597418/en/. Weaver CG et. al, Hypertension. 2015;66:502-508.
Blood Pressure Management Blood Pressure Management
Office Blood Pressure Measurement Automated Office Blood Pressure (AOBP) Performed using an automated devices Takes a series of oscillometric measurements Patient is left unattended in a private area while 3-6 consecutive readings are taken Office Blood Pressure Measurements (OBPM) Performed with the provider in the room Oscillometric or electronic devices are preferred Auscultatory mercury or aneroid if electronic is not available Preferred Method of In-Office Measurement Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Out-of-Office Blood Pressure Assessment Ambulatory blood pressure monitoring (ABPM) A validated oscillometric device which must be worn by the patient for a 24-hour period, Measurements taken at 20-to 30-minute intervals Home Blood Pressure Monitoring (HBPM) Self-monitoring method Requires the patient to measure their blood pressure twice in the morning and evening for 7 days 2020 Preferred Method of Out-of-Office Measurement Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Four Approaches to Assess Blood Pressure* Displayed mean SBP 135 mmHg or DBP 85 mmHg is high Mean SBP 130-139 mmHg or mean DBP 85-89 mmHg is high-normal Mean SBP 140 mm Hg or DBP 90 mmHg is high Mean awake SBP 135 mmHg or DBP 85 mmHg or mean 24-hour SBP 130 mmHg or DBP 80 mmHg are high Mean SBP 135 mmHg or DBP 85mm Hg are high and associated with an increased overall mortality risk AOBP OBPM ABPM HBPM * Note These values are for most individuals, thresholds for persons with diabetes have not been validated by are likely lower. Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Diagnosis and Follow Diagnosis and Follow- -Up Up
Hypertension Diagnostic Algorithm Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Mean Office BP 180/110 mmHg Mean office BP 180/110 mmHg or hypertensive emergency No need for additional BP assessment to make the hypertension diagnosis Diagnose with hypertension and initiate treatment Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Hypertension Diagnosis in People with Diabetes OBPM threshold is different in patients with diabetes AOBP and ABPM diagnostic thresholds in diabetes have not yet been validated Potential prognostic value of ABPM and HBPM exist to rule out white coat or masked HT Diagnosis is recommended by OBPM 130/80 mmHg on 3 different days 2020 Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Hypertension Diagnosis Algorithm 1st visit AOBP or OBPM is elevated Consider ABPM (preferred) or HBPM If ABPM or HBPM are elevated, then diagnosis of hypertension can be made Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
White Coat and Masked Hypertension Derived from Pickering TG, et al. Hypertension 2002:40:795-6. 200 180 Ambulatory BP mmHg MASKED HYPERTENSION TRUE HYPERTENSION 160 140 135 WHITE COAT HYPERTENSION 120 NORMOTENSION 100 100 120 140 160 180 200 Manual Office BP mmHg Derived from Pickering TG, et al. Hypertension 2002:40:795-6.
The Prognosis of White Coat Hypertension White Coat and Masked Masked 35 CV events per 1000 patient-year CV Events 30 25 20 15 10 5 0 Normal White coat Uncontrolled Masked Okhubo T, et al. J Am Coll Cardiol 2005;46;508-15
Assessment of Patients with Elevated BP in Visit 1 If AOBP or OBPM elevated: History Physical examination Diagnostic tests for target organ damage (if clinically indicated) CV Risk factors Visit 2 should be scheduled within 1 month
Assess For Target Organ Damage Cerebrovascular disease Stroke (ischemic stroke, TIA, intracerebral hemorrhage, aneurysmal subarachnoid hemorrhage) Vascular dementia Hypertensive retinopathy Left ventricular dysfunction, left ventricular hypertrophy, heart failure CAD (MI, anginal pectoris, ACS) Renal disease (eGFR < 60 mL/min/1.73 m2, albuminuria) Peripheral artery disease (reduced ankle brachial index) Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Assess CV Risk Factors History of clinically overt ASCVD (eg, PAD, stroke, TIA) Nonmodifiable Age 55 years Male sex Family history of premature CVD (age < 55 in men and < 65 in women) Modifiable Sedentary lifestyle Poor dietary habits Abdominal obesity Dysglycemia Smoking Dyslipidemia Stress Nonadherence Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Routine and Optional Lab Testing in People with Hypertension Routine Tests Optional tests (clinical circumstance) Patients with diabetes (ACR, and according to Diabetes Canada guidelines) Pregnancy test Echocardiogram (when clinically relevant) Left ventricular ejection fraction assessment (when evidence of heart failure) Urinalysis Blood chemistry (potassium, sodium, and creatinine) Fasting blood glucose and/or A1C Serum total cholesterol, LDL-C, HDL-C, non-HDL-C and triglycerides Standard 12-lead electrocardiography Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Cardiovascular Risk Assessment Multifactorial risk assessment models can be used to: Predict more accurately an individual s global cardiovascular risk Help engage individuals in conversations about health behaviour change to lower BP Use antihypertensive therapy more efficiently Consider informing patients to promote risk factor modification Terms such as cardiovascular age, vascular age, or heart age to inform patients of their risk status Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Follow-Up Recommendations BP at yearly intervals No hypertension or target organ damage Hypertensive patients modifying health behaviours BP at 3- to 6-month BP every 1 or 2 months for patients with higher BP BP monthly or every 2 months, until readings on 2 consecutive visits are below their target Shorter interval in symptomatic, severe HT, intolerance to medications, or target organ damage BP at 3- to 6-month intervals or as clinically indicated once target BP is reached Follow-up with demonstrated white coat effect Patients on antihypertensives ABPM or HBPM Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
2. Cardiovascular Health 2. Cardiovascular Health Promotion Promotion
Key Messages 1. Health behaviour change plays an important role in hypertension prevention and BP-lowering in people diagnosed with hypertension 2. Health behaviour change is strongly recommended as a first-line intervention to lower BP in people with hypertension 3. Optimization of lipid levels with the use of statins in higher-risk patients is recommended 4. The use of acetylsalicylic acid (ASA) for primary prevention of cardiovascular disease is no longer recommended in people with hypertension Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Vascular Protection Statin therapy - hypertensive patients with 3 CV risk factors or established ASCVD Tobacco use Assess status regularly and advise patients to quit Advice with combination pharmacotherapy (e.g. varenicline, bupropion or nicotine replacement therapy) should be offered Low dose ASA - The use in the primary prevention of cardiovascular disease has been removed Little overall effectiveness and a significant risk of major bleeding 2020 Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Health Behaviours 30-60 minutes of moderate-intensity dynamic exercise (eg, walking, jogging, cycling, or swimming) 4-7 days per week Higher intensities of exercise are not effective Use of resistance or weight training exercise (such as free-weight lifting, fixed-weight lifting, or handgrip exercise) does not adversely influence BP Assess height, weight and waist circumference and calculate BMI Maintenance of a healthy weight is recommended All hypertensive patients with a BMI > 25 kg/m2 should be advised to lose weight In healthy adults, abstaining from alcohol or reducing alcohol intake to 2 drinks per day or less is recommended to prevent hypertension Physical Exercise Weight Reduction Alcohol 2020 Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Health Behaviours Diet High in fruit, vegetables, low-fat dairy products, whole grain foods rich in dietary fibre and protein from plant sources that is reduced in saturated fat and cholesterol (DASH) Sodium intake to 2000 mg/day Calcium and magnesium Not recommended Potassium If not at risk of hyperkalemia, to reduce BP Stress management In those whom stress might be contributing to high BP, stress management should be considered as an intervention Individualized cognitive-behavioural interventions are more likely to be effective when relaxation techniques are used Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Risk Factors of Hyperkalemia Before advising to potassium intake, assess for those at high risk of hyperkalemia: Patients taking renin-angiotensin-aldosterone inhibitors Patients taking other drugs that can cause hyperkalemia (eg, trimethoprim and sulfamethoxazole, amiloride, triamterene) Chronic kidney disease (glomerular filtration rate < 45 mL/min/1.73 m2) Baseline serum potassium > 4.5 mmol/L Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
3. Management: Uncomplicated 3. Management: Uncomplicated Pharmacotherapy Pharmacotherapy
Key Messages 1. 2. A risk-based approach to treatment thresholds and targets The use of clinical judgement and shared decision making when identifying BP targets to ensure feasibility in the patient s broader clinical, social, and economic context Patients with existing CVD or with elevated CV risk should be considered for intensive SBP targets (ie, SBP 120 mm Hg). First-line in adults with uncomplicated hypertension - ACE inhibitors, angiotensin receptor blockers (ARBs), calcium channel blockers (CCBs), and longer-acting thiazide-like diuretics -Blockers can be used safely as first-line therapy in < 60 years patients only with uncomplicated hypertension When possible, the use of a single-pill combination (SPC) should be used to improve treatment efficacy, efficiency, and tolerability 3. 4. 5. 6. Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
BP Thresholds for Initiation and Targets Patient Population BP threshold (mmHg) for initiation of therapy BP target (mmHg) for treatment Low risk (no target organ damage or CV risk factors) SBP 160 DBP 100 SBP < 140 DBP < 90 High risk of CVD* Diabetes mellitus SBP 130 SBP 130 DBP 80 SBP < 120 SBP < 130 DBP < 80 All others SBP 140 DBP 90 SBP < 140 DBP < 90 * Measured by automated office blood pressure measurement Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
High-Risk Adult Patients - Intensive Management Clinical or subclinical cardiovascular disease; or Chronic kidney disease (nondiabetic nephropathy, proteinuria < 1 g/d, eGFR 20-59 mL/min/1.73 m2); or Estimated 10-year global cardiovascular risk 15%y; or Age 75 years Patients with 1 or more clinical indications should consent to intensive management Target Systolic Blood Pressure < 120 mmHg Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Managing Diastolic and Isolated Systolic Hypertension Diastolic hypertension systolic hypertension Initial therapy Thiazide/thiazide-like diuretic with longer-acting diuretics preferred -blockers (< 60 years) ACEi (non-black) ARB Long-acting CCB If not at target on standard dose monotherapy Add additional first-line agents Isolated systolic hypertension Initial therapy Thiazide/thiazide-like diuretic Long-acting CCB ARB If not at target on standard dose monotherapy Add additional first-line agents Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
4. Management: Complex 4. Management: Complex Comorbidities Comorbidities
Key Messages 1. Hypertension frequently coexists with other conditions that influence therapeutic decision making. Polypharmacy and competing risks need to be considered carefully. 2. Adults with diabetes and certain forms of chronic kidney disease might benefit from more intensive BP targets (ie, SPB 130 mm Hg or 120 mm Hg). Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
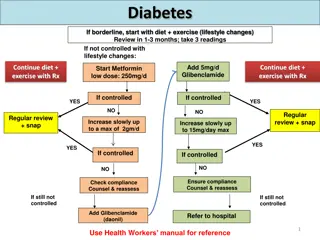
Managing Hypertension in Diabetes Mellitus Target SBP < 130 mmHg and DBP < 80 mmHg Patient with diabetes and either ASCVD, CKD or CV risk factors: ACE inhibitor or ARB as initial therapy Patient with diabetes without these indications ACE inhibitor, ARB, dihydropyridine CCBs or thiazide/thiazide-like diuretics as initial therapy If not at target on standard dose monotherapy Add additional first-line agents If taking ACE inhibitor, a dihydropyridine CCB is preferable to a thiazide/thiazide-like diuretic Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Hypertension in Chronic Kidney Disease Individualize BP targets in patients with CKD. Consider intensive targets (SBP < 120 mm Hg) in appropriate patients. For patients with hypertension and proteinuric CKD, initial therapy should be: ACE inhibitor or an ARB In most cases, combination therapy with other antihypertensive agents might be needed to reach target BP levels Combination of an ACE inhibitor and ARB is not recommended 2020 Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
SBP Targets in Patients with Nondiabetic CKD 2020 Nondiabetic CKD Systolic BP Target < 120 mmHga < 110 mmHgb < 140 mmHgc Patients meeting SPRINT criteria* Patients with adult polycystic kidney disease All other patients with nondiabetic CKD * Patients > 50 years of age, at elevated cardiovascular risk with systolic BP 130-180 mm Hg. a. Measurement is on the basis of automated office BP b. Measurement is on the basis of HBPM c. Measurement is on the basis of office BP. Further reduction in SBP target may be individualized at the discretion of the treating physician considering the patient s specific kidney disease, comorbidities, and age. Moreover, we recommend that potential benefits and adverse events related to lower systolic BP targets be discussed with each patient and therapeutic decisions should be shared Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Hypertension and Stroke BP management in acute ischemic stroke (onset to 72 hours) Refer to the current Canadian Stroke Best Practices recommendations (www.strokebestpractices.ca/recommendations) BP management after acute ischemic stroke Consider initiating antihypertensive therapy after the acute phase Target BP < 140/90 mmHg ACE inhibitor and thiazide/thiazide-like diuretic combination is preferred For patients with stroke, the use of an ACE inhibitor with an ARB is not recommended BP management in hemorrhagic stroke (onset to 72 hours) Refer to the current Canadian Stroke Best Practices recommendations Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Hypertension with CAD Initial Therapy ACE inhibitor or ARB Combination ACE inhibitor and a dihydropyridine CCB is preferable to an ACE inhibitor and a thiazide/thiazide-like diuretic Stable angina pectoris (without HF, MI, or CABG) -blocker or CCB Avoid Short-acting nifedipine Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Hypertension with a Recent Myocardial Infarction Initial Therapy -blocker as well as ACE inhibitor ARB can be use in those intolerant to ACE inhibitor Additional therapy CCBs can be used after MI when -blockers are contraindicated Avoid non-dihydropyridine CCBs when there is heart failure Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Hypertension and Heart Failure Initial therapy (LEVF <40%) ACE inhibitor (ARB if intolerant) -blocker Additional therapy Mineralocorticoid receptor antagonists can be added Other diuretics can be added as needed Hydralazine and isosorbide dinitrate (ACE inhibitor or ARB cannot be used) Other therapy Angiotensin receptor-neprilysin inhibitor can be used in place of ACE inhibitor or ARB for patients with HFrEF (LEVF <40%) who remain symptomatic despite initial therapy Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Hypertension and Left Ventricular Hypertrophy Initial therapy ACE inhibitors ARBs Long-acting CCBs Thiazide/thiazide-like diuretics Avoid Direct arterial vasodilators such as hydralazine or minoxidil Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
5. Resistant Hypertension 5. Resistant Hypertension
Key Messages 1. Resistant hypertension is defined as BP above target despite 3 or more BP-lowering drugs at optimal doses preferably including a diuretic (and usually a renin-angiotensin-aldosterone system blocker and a CCB). 2. Accurate office and out-of-office BP measurement is essential. 3. Other reasons for apparent resistant hypertension should be eliminated before diagnosing true resistant hypertension, including nonadherence, white coat effect, and secondary hypertension. 4. Pharmacotherapy with the additional use of spironolactone, bisoprolol, doxazosin, amiloride, eplerenone, or clonidine with the baseline regimen decreases BP significantly, with the greatest BP-lowering shown with spironolactone. Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Resistant Hypertension Resistant hypertension High BP despite use of 3 BP-lowering drugs at optimal doses Patients are at high risk of adverse cardiovascular outcomes Patients with resistant hypertension should be referred to providers with expertise in diagnosis and management of hypertension Therapy A combination of ACE inhibitor/ARB, CCB, and a diuretic are used to ensure that different mechanisms for increases in BP are blocked 2020 Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Diagnostic Aspects in Suspected Resistant Hypertension Accurate office blood pressure measurement Out-of-office blood pressure measurement, preferably with a 24-hour ambulatory blood pressure monitoring Optimize blood pressure-lowering drug choice and dosage Evaluation of target organ damage Review adherence Indirect measures (eg, pill counts, pharmacy refill data) Direct measures as appropriate (therapeutic drug monitoring, direct observed testing) Assess for sleep apnea Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Therapeutic Strategies in Resistant Hypertension Review and reiterate healthy lifestyle measures Improve adherence When possible, eliminate drugs and substances that cause higher blood pressure Add pharmacotherapy Evidence of significant blood pressure-lowering exists for: Spironolactone, eplerenone, amiloride, a- and b-adrenergic antagonists, Clonidine Evaluate and refer if secondary hypertension suspected Primary aldosteronism Renovascular hypertension Pheochromocytoma and paraganglioma Other causes of secondary hypertension Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086
Assessment for Renovascular Hypertension 2 of the following, investigate for fibromuscular dysplasia (FMD)- related renal artery stenosis Significant (> 1.5 cm), unexplained asymmetry in kidney sizes; Abdominal bruit without apparent atherosclerosis; FMD in another vascular territory; Family history of FMD 2 of following suggest investigation: Sudden onset or worsening of hypertension and age > 55 or < 30 years Presence of an abdominal bruit Hypertension resistant to 3 drugs in sCR 30% associated with use of an ACE inhibitor or ARB; Other ASCVD, particularly in patients who smoke or have dyslipidemia Recurrent pulmonary edema associated with hypertensive surges Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology. 2020;36(5):596-624. doi:10.1016/j.cjca.2020.02.086