Understanding Hypertension: Types, Pathogenesis, and Management
The article discusses the physiological basis, types, pathogenesis, and genetic predisposition of hypertension. It explains the revision of terminology related to blood pressure and the calculation of mean arterial pressure. Secondary hypertension, causes, and mean arterial pressure determination are also covered in this informative piece.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Physiological Basis of Management of Hypertension Professor Narsingh Verma
Types of Hypertension Primary or Essential Hypertension Secondary Hypertension Pregnancy induced Hypertension White Coat Hypertension Masked Hypertension Malignant Hypertension MESOR Hypertension
Pathogenesis of essential hypertension Multifactorial and complex Humoral mediators Vascular reactivity Circulating blood volume Vascular caliber Blood viscosity Cardiac output Blood vessel elasticity Neural stimulation.
Genetic Predisposition A possible pathogenesis of essential hypertension has been proposed in which multiple factors, including genetic predisposition, excess dietary salt intake, and adrenergic tone, may interact to produce hypertension. Although genetics appears to contribute, the exact mechanisms underlying essential hypertension have not been established.
Revision of Terminology When the left ventricle ejects blood into the aorta, the aortic pressure rises. The maximal aortic pressure following ejection is termed the systolic pressure (Psystolic) As the left ventricle is relaxing and refilling, the pressure in the aorta falls. The lowest pressure in the aorta, which occurs just before the ventricle ejects blood into the aorta, is termed the diastolic pressure (Pdiastolic) The difference between the systolic and diastolic pressures is the aortic pulse pressure, which typically ranges between 40 and 50 mmHg The mean aortic pressure (Pmean) is the average pressure (geometric mean) during the aortic pulse cycle.
Mean Arterial Pressure As blood is pumped out of the left ventricle into the aorta and distributing arteries, pressure is generated. The mean arterial pressure (MAP) is determined by the cardiac output (CO), systemic vascular resistance (SVR), and central venous pressure (CVP) according to the following relationship, which is based upon the relationship between flow, pressure and resistance: Eq. 1: MAP = (CO SVR) + CVP Because CVP is usually at or near 0 mmHg, this relationship is often simplified to: Eq. 2: MAP CO SVR At normal resting heart rates, MAP can be approximated by the following equation MAP = Diastolic Blood Pressure + 1/3 of Pulse Pressure
Secondary hypertension 80% of cases are caused by renal diseases such as diabetic nephropathy, chronic glomerulonephritis, adult polycystic disease, chronic tubulointerstitial nephritis, renovascular disease Endocrine causes Conn s syndrome, adrenal hyperplasia, phaeochromocytma, Cushing s syndrome, acromegaly Congenital cardiovascular diseases coarctation of aorta Drugs contraceptive pills, steroids, sympathomimetics, vasopressin Pregnancy
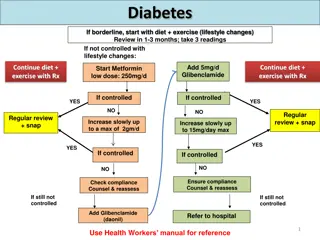
Management Many kinds of treatments are used to manage hypertension The treatment should be chosen according to the cause and also to the age, sex, ethnic origin and physiological status of the patient Both pharmacological and non pharmacological therapies are used in Synergy Hypertensive patients excluding severe or malignant hypertensive ones, should be treated after a period of assessment with repeated blood pressure measurements It should always be combined with advice and non pharmacological therapy.
Non pharmacological treatment:- Lifestyle modification through weight reduction, care of dietary intake, No tobacco and alcohol consumption and dynamic exercise Weight reduction, Controlling Body Mass index (BMI) < 23kg/m2 (may indicate a healthy individual. During exercise blood pressure rises by several mechanisms such as increase in sympathetic activity, cardiac output and heart rate. As this blood pressure rises as immediate effect of exercise. But as a long term effect blood pressure is reduced by exercise. Aerobic exercise that is intended to increase oxygen consumption is recommended for lowering blood pressure in hypertensive patients. Antihypertensive effects of exercise are mediated through several mechanisms. used for all hypertensive patients and borderline hypertensive.
NO level is increased by exercise. It plays a major role in regulating vascular tone and antiatherosclerotic effects, It is a potent vasodilator metabolite. Plasma NO2_ and NO3_ concentration increase significantly by aerobic exercise. And also cGMP concentration which helps to produce NO is increased NO is sensitive to inactivation of superoxide radicals. Relationship between blood pressure lowering effect and NO bioactivity remains unknown. Exercise needs high level of energy. So, excessive adipose tissue that accumulates in obese ones is used to gain energy. It helps to reduce obesity. Because of the reduction of adipose tissue, need of blood flow to them is reduced. This helps to lower cardiac output and blood pressure. Body temperature rises during exercise. To regulate the body temperature, compensatory mechanisms are activated. They increase heat loss by increasing ventilation, radiation, dilatation of skin blood vessels and sweating vasodilatation decreases peripheral resistance and decreasing blood pressure occurs. By sweating, loss of body fluids includes water and electrolytes such as Na+ are increased. It causes reduction of blood volume and blood pressure. As this exercise benefits low blood pressure for hypertensive patients.
Dietary control Reducing intake of total fat, saturated fat and salt in diet and taking vegetables, fruits, potassium and fish oil included diet is recommended for hypertensive patients. In addition to that high intakes of vitamin D, protein, amino acid, tea, dark chocolate and foods high in NO3_ help to reduce bl Dietary fat specially unsaturated fatty acids have an effect of increasing circulating lipoproteins. They increase the level of Low Density Lipoprotein (LDL). They may cause increased risk of obesity and atherosclerosis. They also increase arterial stiffness and cause oxidative stress. Those things contribute to increase blood pressure. So reducing intake those things help to reduce blood pressure. Unsaturated fatty acids which are in fish oil also contribute to reduce blood pressure. Vegetables, fruits . Excessive salt intake can cause elevation of arterial pressure mainly by increasing Extracellular Fluid (ECF) volume. Though pure water is excreted by kidney as rapidly as it is taken hypertensive patients are recommended to take diet with low salt content < 6g NaCl per day
No Tobaco and Alcohol Substances in tobacco and cigarette smoke adversely change the structural and mechanical properties of arteries Structural features such as wall thickness and functional features as NO production and bioactivity and endothelin 1 levels may be altered, Smoke reduces NO bioactivity as a result of oxidative stress,increase arterial stiffness. Compliancy of the arteries is reduced and difficult to dilate. Total peripheral resistance is increased resulting increase in cardiac output and blood pressure Alcohol causes arterial stiffness. And also it has psychological effects that lead to increase in blood pressure
Multiple Drugs Can be used as one drug therapy or as drug combinations Using drug combinations is more effective than the other in most of the cases Diuretics, Adrenergic receptor blockers, Angiotensin II receptor antagonists, Angiotensin Converting Enzyme (ACE) inhibitors, Renin inhibitors, Calcium channel blockers, Blockers , Vasodilators and centrally acting drugs are the main classes of drugs that used to treat hypertension
Guidelines Therapy should be based on following guidelines What are the stages that hypertensive therapy should be started Drug therapy should be initiated in subjects with sustained systolic blood pressure 160 or sustained diastolic blood pressure 100 mmHg. Individuals with sustained systolic blood pressure 140-150 or sustained diastolic blood pressure 90- 99 mmHg who have a risk of target organ damage or a 10 years cardiovascular disease risk > 20%.
Targets Start therapy for subjects with systolic blood pressure sustained 140 or diastolic blood pressure sustained 90 mmHg associated with diabetes mellitus. For most patients, a target of 140/85 mmHg is recommended. For patients with diabetes mellitus, renal impairment or cardiovascular disease, a lower target of 130/80 mmHg is recommended
Addressing Variability Most of the hypertensive patients require a combination of drugs to achieve recommended targets In most patients therapy with statins and aspirin is added to reduce the overall cardiovascular risk Repeated blood pressure measurements, Home monitoring and some time ABPM is required to assess Short term, Longterm, visit to visit and seasonal variability
Diuretics Diuretics have prompt natriuretic effect,which increases the excretion of sodium salts in the urine Thiazide diuretics and some loop agents act as mild carbonic anhydrase inhibitors resulting reduce formation of HCO3 & also they reduce reabsorption of Na+, HCO3_, Cl_ and water in proximal convoluted tubule of nephron. 20% of Na+ reabsorption occurs in Loop of Henle. Loop diuretics inhibit this action. Some agents inhibit the active transport of Cl_ ions at the ascending limb of Henle loop Some diuretics competitively bind to aldosterone receptors in distal convoluted tubule and inhibit the action of aldosterone on increasing permeability to Na+ in that tubule----reduce plasma Na+ concentration ---- ------ decrease in fluid volume--------- reduction of preload on the heart----- -------may cause reduction of cardiac output and arterial pressure blood pressure is reduced without changing total peripheral resistance These drugs also reduce the risk of stroke.
Hydrochlorthiazide Chlorthalidone Indepamide Acetazolamide Aldactone
Angiotensin II receptor antagonists; These drugs selectively block the receptors for angiotensin II Angiotensin II is a potent vasoconstrictor and it also stimulates increased secretion of aldosterone by adrenal cortex Aldosterone increase the permeability to Na+ in distal convoluted tubule and collecting tubule and cause Na+ and water retention. It increases fluid volume resulting increase in blood pressure It mediates those actions by binding to specific membrane bound receptors There are two types of receptors, AT1 and AT2. AT1 is responsible for major action on Renin Angiotensin System (RAS) Action of drugs is potentiated by negative salt balance and attenuated by positive salt balance Losartan, Telmesartan, Olmesartan, Azilsartan, Fimasartan
Angiotensin Converting Enzyme (ACE) inhibitors These drugs block the conversion of angiotensin I to angiotensin II It mediates RAS as above description. So, blocking its synthesis those actions are inhibited and lowers the blood pressure also they block the degradation of bradykinin It is a potent vasodilator By dilating vessels it help to reduce blood pressure Captopril, Ramipril, Perendopril, Lisinopril
Renin Inhibitors These drugs directly inhibit the plasma renin activity Renin is released from kidney in response to decrease of renal perfusion pressure and contribute to increase blood pressure by stimulating the conversion of angiotensinogen to angiotensin I By inhibiting this reaction RAS is interrupted reducing arterial pressure eg Alesikerin
Beta adrenoceptor blockers They act by decreasing total peripheral resistance and cardiac output Using 1 selective antagonists is more effective than non-selective drugs They target 1 adrenergic receptor mRNA with antisense oligodeoxynucleotides ( 1-AS-ODN). Main mechanism is to reduce efferent sympathetic activity underlying decrease in plasma noradrenaline level. Reduction of sympathetic activity significantly decreases cardiac contractility displaying a negative inotropic effect According to Starling s law of the heart, force of contraction is proportional to stroke volume. When the contractility is reduced stroke volume and cardiac output decreases and blood pressure lowers As a second mechanism they inhibit RAS to produce sustained antihypertensive effect Newer blocking drugs also reduce blood pressure through NO mediated vasodilatation Atenolol, Metaprolol, Bisoprolol, Acebutol, Sotalol,Carvedolol, Nebiolol
Calcium channel blockers They effectively reduce blood pressure by arteriolar dilatation and some agents also reduce the force of cardiac contraction Ca2+ and Ca channels are more important in contraction of cardiac muscle. Contraction occurs due to movement of actin and myosin filaments When action potential spreads to cardiac muscle membrane, Ca channels are opened. Large amounts of Ca2+ release from transverse tubules and ECF. They diffuse into myofibrils and bind to troponin c. It results in exposing of binding sites for myosin heads on actin. Myosin heads bind to actin and power stroke occur causing cardiac contraction When these drugs block the Ca2+ channels, releasing Ca2+ is reduced and force of contraction reduces. It may cause decrease in cardiac output and blood pressure. L/N type calcium channel blockers inhibit aldosterone production which induced by angiotensin II.
Alpha blockers adrenergic receptors are present in peripheral vascular system and also in Central Nervous System (CNS) All in vascular system are innervated by sympathetic nervous system These agents block postsynaptic 1 receptors Sympathetic activity causes peripheral vasoconstriction. By blocking them, this action is reduced and blood pressure lowering occurs Prazocin, Alfa methyldopa, Minipress XL
Vasodilators These drugs act directly on vascular smooth muscle and relax them without contribution of cell receptors. By relaxing smooth muscle, vasodilatation occurs. This reduces total peripheral resistance and venous return to the heart is reduced through it. As this, lowers the blood pressure. This antihypertensive effect is independent from the sympathetic tone. Some vasodilating agents inhibit sympathetic nervous signals to the kidneys or block the action of sympathetic transmitter substance on renal vasculature. These drugs also directly relax the smooth muscle of renal vasculature and through it block the RAS
Centrally acting drugs These drugs act by central regulation of sympathetic nervous system
Drug Combinations Majority of hypertensive patients need at least two drugs to control blood pressure under the level of 140/90 mmHg Better combinations of antihypertensive drugs use agents from different classes with different primary actions. So, that hypotensive effects are obtained by use of low doses. By combination of drugs we can observe greater blood pressure reductions than mono drug therapy. It may cause fewer side effects than one drug therapy because of using small doses of two drugs. Commonly using combinations are diuretics and blockers, ACE inhibitors and angiotensin II receptor antagonists and as well as ACE inhibitors and calcium channel blockers A+B or A+C or A+D or A+C+D but Never A+A
Management of severe or malignant hypertension Treatment should initiate immediately for patients who have severe hypertension, malignant hypertension or patients with severe hypertensive complications such as cardiac failure. But it is not recommended to reduce blood pressure too rapidly because it may cause cerebral, renal and retinal damage and myocardial infarction Blood pressure response to those therapies must be carefully conducted. In most cases the treatment is aimed to reduce the diastolic blood pressure to 100-110 over 24 hours. It can be normalized over 2-3 days only with oral medication In very severe cases rapid control of blood pressure is required. Intravenous sodium nitroprusside is used to such types of treatments
Management of hypertension in pregnancy The cardiac output is increased in pregnancy, but greater fall in total peripheral resistance occurs. So, blood pressure is reduced than normal But in 8-10% of pregnant women are reported as pregnancy induced hypertensive patients Pre- eclampsia is a syndrome consisting of pregnancy induced hypertension and proteinuria. Reduction of uteroplacental circulation causes hypertension Placental ischaemia leads to dysfunction of maternal vascular endothelium that result in increased formation of endothelin and thromboxane and increased in vascular sensitivity to angiotensin II. And also causes decreased formation of vasodilators such as NO and prostacyclin Maternal blood volume is about 30% above normal. This increases during latter half of pregnancy. Increasing aldosterone and oestrogen cause increased fluid retention by kidneys And also bone marrow produces extra red blood cells Many antihypertensive drugs are contraindicated in pregnancy. When blood pressure is increased to > 160/110 mmHg, treatment is required for protection of the mother Labetalol and methyldopa, nifedipine. intravenous hydralazine