F/TAF vs. F/TDF for HIV Pre-Exposure Prophylaxis: DISCOVER Study Findings
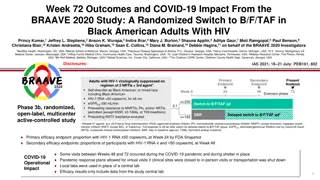
Study results reveal that F/TAF provides rapid onset and longer sustained HIV protection compared to F/TDF in pre-exposure prophylaxis. The randomized noninferiority trial included 2694 participants with a primary analysis at weeks 48 and 96. Disclosure statements indicate involvement of various healthcare organizations in sponsoring the study.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
DISCOVER STUDY for HIV Pre-Exposure Prophylaxis: F/TAF has a more Rapid Onset and Longer Sustained Duration of HIV Protection Compared with F/TDF Christoph D. Spinner1, Jason Brunetta2, Peter Shalit3, Maria Prins4, Michelle Cespedes5, Diana Brainard6, Moupali Das6, Scott McCallister6, Sophia R. Majeed6, Anita Mathias6, Ramin Ebrahimi6, Frederick Cruickshank8, Jason Halperin9, Jay E. Gladstein10, and Patrick W.G. Mallon11 1Technical University Munich, Munich, Germany; 2Maple Leaf Medical Clinic, Toronto, Canada; 3University of Washington School of Medicine, Seattle, USA; 4Public Health Service of Amsterdam (Geneeskundige en Gezondheidsdienst Amsterdam), Netherlands; 5Icahn School of Medicine at Mount Sinai, New York, New York, USA; 6Gilead Sciences, Inc., Foster City, California, USA; 7University of Colorado, Denver, CO, 8Novant Health Presbyterian Medical Center, NC,USA; 9CrescentCare Health and Wellness Center, New Orleans, Louisiana, USA; 10Global Healthcare Los Angeles, California, USA; 11University College Dublin School of Medicine, Ireland Tuesday, July 23 IAS 2019, Mexico City
Thank You! Study participants, partners, families Investigators and site staff Community advisors FRANCE E Cua J-M Molina P Philibert G Pialoux AUSTRIA B Haas A Rieger ITALY A Antinori A Lazzarin UK V Apea A Clarke O Dosekun R Gilson S Kegg C Leen N Nwokolo F Post I Reeves G Schembri S Taylor US D Asmuth A Avery P Benson M Berhe I Brar C Brinson JH Burack T Campbell M Cespedes M Coleman CM Creticos GE Crofoot FA Cruickshank E Daar E DeJesus W Dinges S Doblecki-Lewis T Donovan J Flamm JE Gallant J Gladstein RM Grant R Grossberg J Halperin WD Hardy CB Hare S Hassler R Hengel K Henry T Hodge S Hosek M Iandorio A LaMarca C Lucasti S Mannheimer CT Martorell M Markowitz K Mayer A Mills S Morris K Mounzer O Ogbuagu O Osiyemi A Petroll J Phoenix MN Ramgopal B Rashbaum GJ Richmond PJ Ruane L Salazar AJ Scarsella M Scott P Shalit JL Stephens MA Thompson G Voskuhl BH Wade DA Wohl K Workowski B Young CANADA J Brunetta JJ de Wet B Trottier J Szabo C Tremblay NETHERLANDS M Prins GERMANY H Jessen G Knecht I Krznaric C Spinner SPAIN J Coll M Crespo J del Romero Gerrero D Podzamczer DENMARK J Gerstoft G Kronborg C Larsen D Larsen IRELAND C Bergin P Mallon 2
Disclosures Dr. Spinner has received: Research grants from Gilead, Janssen-Cilag, and ViiV Healthcare Honoraria for speakers bureau and/or advisory boards from Gilead, AbbVie, Janssen, MSD, Teva/Hexal, and ViiV Healthcare This study was sponsored by Gilead Sciences 3
DISCOVER: A Randomized, Double Blind, Noninferiority Trial F/TAF 200/25 mg qd n=2694 Randomized 1:1 Primary analysis: HIV incidence/100 PY when 100% complete Week 48 & 50% complete Week 96 MSM or TGW Adults 18 y Double-blinded Active controlled F/TDF 200/300 mg qd n=2693 Eligibility criteria Sexual behaviors associated with higher risk of HIV acquisition 2 episodes of condomless anal sex with 2 unique partners in 12 weeks prior to enrollment Diagnosis of rectal gonorrhea, chlamydia, or syphilis in 24 weeks prior to enrollment HIV and HBV negative, prior use of PrEP allowed F/TAF, emtricitabine/tenofovir alafenamide; F/TDF, emtricitabine/tenofovir disoproxil fumarate; HBV, hepatitis B virus; MSM, men who have sex with men; PrEP, pre-exposure prophylaxis; PY, person-years; TGW, transgender women. 4
Primary Efficacy Endpoint: Noninferiority Achieved Incidence Rate Ratio (95% CI) HIV Incidence 0.6 Favors F/TAF Favors F/TDF 0.5 HIV Incidence Rate/ 100 PY (95% CI) 0.4 0.34 NI 0.47 0.3 margin 0.19 1.15 0.2 0.16 0.1 IRR=1, no difference 0 n=2694 7 infections 4370 PY n=2693 15 infections 4386 PY 0 1 2 1.62 Incidence rate ratio (IRR) was 0.47 = (0.16/0.34) 22 HIV infections in 8756 PY of follow-up Noninferiority was confirmed in sensitivity analysis excluding 5 infections suspected at baseline (1 F/TAF; 4 F/TDF); IRR: 0.55 [0.20, 1.48]) CI, confidence interval; NI, noninferiority. 5
Were the Fewer HIV Infections in F/TAF Due to Chance? The incidence rate ratio (IRR) was 0.47 (95% CI 0.19, 1.15) reflecting that the point estimate of the HIV incidence rate was 53% lower in the F/TAF arm compared with F/TDF Probability of the above result due to chance is 3 in 1,000 Post-hoc Bayesian analysis calculated a 96% (95% credible interval) probability that F/TAF is more effective than F/TDF We examined sexual behavior, STI incidence, adherence, and PK to evaluate any differences between F/TAF and F/TDF which could explain the fewer infections in the F/TAF arm 6
Assessments of HIV Risk, STIs, Adherence, and PK/PD All DISCOVER Participants (N=5387): Visits every 12 weeks HIV Risk Behavior Confidential self-report of type and frequency of sexual behaviors, partners Adherence Self-report; pill count Dried Blood Spot analysis STI Incidence GC/CT (rectal, urine, oropharynx by NAAT) and syphilis testing AE reporting Adherence and Efficacy Evaluated adherence and efficacy relationship using exact conditional logistic regression in a nested case-control-study n=22 n=109 Pharmacokinetics TFV-DP in PBMCs (Week 4, n=324; randomized subset) Simulation of duration above threshold of protection with TAF and TDF Case with incident HIV 5 controls matched on: Geography Timing of HIV diagnosis in study Presence or absence of rectal STI AE, adverse event; BMD, bone mineral density; CASI, computer-aided self-interview; DBS, dried blood spot; GC/CT, gonococcus/chlamydia trachomatis; NAAT, nucleic acid amplification test; PBMC, peripheral blood mononuclear cell; STI, sexually transmitted infection. 7
No Difference in Sexual Behaviors or STI Incidence F/TAF F/TDF Number of Condomless Receptive Anal Sex Partners Lab-Based Rectal Gonorrhea/Chlamydia 10 20 Mean No. of Partners (SD) 8 15 Participants, % 6 10 4 5 2 0 0 0 12 24 36 48 60 72 84 96 0 12 24 36 48 60 72 84 96 Week Week AE-based incidence of gonorrhea, chlamydia, and syphilis: F/TAF: 145/100 PY; F/TDF: 139/100 PY *Collection method different at Week 12. SD, standard deviation. 8
No Difference in Self-Reported Adherence or Pill Count CASI Self-report 100 Pill Count 100 100 80 80 80 Participants, % 68 Adherence % 69 78 78 60 60 60 79 80 80 80 80 80 80 80 80 81 80 81 81 81 82 82 95 80 <95 40 40 40 <80 20 20 20 25 25 20 19 18 17 18 19 18 18 17 17 17 17 17 16 16 17 16 15 3 2 2 3 2 3 3 3 4 3 2 3 3 3 3 3 3 3 8 7 0 0 0 4 12 24 36 48 60 72 84 96 4 12 24 36 48 60 72 84 96 F/TAF 98% F/TDF 98% F/TAF F/TDF Median Adherence Adherence was high by self-report and pill count By these measures, very few participants had adherence <80% 9
No Difference in Adherence by TFV-DP Levels in DBS PK Cohort Analysis Set (n=536) F/TAF F/TDF 100 100 80 80 Participants, % 60 60 Tablets/wk 84 84 86 87 87 88 88 88 89 90 90 92 92 93 93 96 4 2 3 40 40 <2 20 20 5 11 12 6 3 8 8 7 6 7 3 5 4 6 2 4 9 7 60 6 48 5 48 5 84 5 36 5 36 5 84 5 72 3 24 2 12 5 72 4 60 3 12 4 24 4 96 0 0 96 Week Week 10
Adherence by DBS at HIV Diagnosis Visit Case-Control Study (Cases=22; Controls=109) F/TAF p<0.001 F/TDF p <0.001 2500 2000 2000 Median TFV-DP Concentration, 1500 fmol/punch(es) (Q1, Q3) 1500 Adherence 1000 4 doses/wk 900 700 2 3 doses/wk 450 350 <2 doses/wk 0 0 HIV Cases n=7 HIV-Neg Controls n=35 HIV Cases n=15 HIV-Neg Controls n=75 Low adherence (adherence <2 doses/week) was independently associated with increased risk of HIV acquisition in both groups Similar results from sensitivity analyses excluding 5 suspected baseline infections 11
Summary of Behaviors No Differences Between Arms in HIV Risk, STIs, or Adherence F/TAF F/TDF There were no differences in HIV risk behavior, prevalence or incidence of STIs, or adherence by pill count, self-report, or dried blood spot between F/TAF and F/TDF Low adherence was strongly associated with HIV acquisition in both arms Next we examined pharmacokinetic differences between F/TAF and F/TDF 12
Higher TFV-DP Levels in PBMCs with TAF vs TDF GI TRACT PLASMA PBMC TDF 300 mg TFV 0.4 min TFV-DP HIV Plasma Half-life TFV TAF 25 mg 30 min Plasma TFV levels ~90% lower with TAF vs TDF TAF delivers 4 7 fold higher TFV-DP GI, gastrointestinal. Lee W, et al. Antimicr Agents Chemo 2005;49:1898-1906; Birkus G, et al. Antimicr Agents Chemo 2007;51:543-50; Babusis D, et al. Mol Pharm 2013;10:459-66; Ruane P, et al. J Acquir Immune Defic Syndr 2013; 63:449-5l; Sax P, et al. JAIDS 2014;67:52-8; Sax P, et al. Lancet 2015;385:2606-15. 13
PBMC TFV-DP Levels and HIV Risk Reduction iPrEX Case-Control Study HIV Incidence Rate/100 PY (95% CI) 6 5 PBO 4 50% risk reduction 3 90% risk reduction 2 99% risk reduction 1 F/TDF 0 8 40 83 BLQ (95% CI <3, 18) 25 50 75 (95% CI 15, 150) 100 125 (95% CI 8, 70) TFV-DP, fmol/106 Freshly Lysed PBMCs Relationship between TFV-DP levels in PBMCs and HIV incidence established from iPrEx data1 EC90: TFV-DP level of 40 fmol/106 cells in PBMCs associated with 90% HIV risk reduction2 1. Figure adapted from Anderson PL, et al. Sci Transl Med 2012;4:151ra125; 2. Anderson PL, et al. CROI 2012. 14
DISCOVER: F/TAF Has Higher PBMC TFV-DP Levels vs F/TDF Week 4, n=324 100,000 10,000 TFV-DP Ctau fmol/106 cells 98% 1000 68% of participants >EC90 404 of participants >EC90 100 61 EC90 10 1 F/TAF n=158 F/TDF n=151 Steady-state TFV-DP levels in PBMCs were 6.3-fold higher with F/TAF vs F/TDF Ctau, concentration 20 28 h postdose. Box median, IQR, whiskers min, max 15
F/TAF Achieves EC90 More Rapidly than F/TDF Phase 1 Study in Healthy Volunteers First Dose 10000 Median TFV-DP Concentration, F/TAF F/TDF 1000 fmol/106 cells (Range) 100 EC90 10 1 0.1 0 2 4 6 8 10 12 Hours 14 16 18 20 22 24 With F/TAF, median TFV-DP concentrations exceeded EC90 within 1-2 h, all within 4 h, consistent with 2 prior studies1-3 In contrast, 3 daily doses of F/TDF are needed to achieve EC90 in PBMCs4 EC90, 90% effective concentration. 1. Schwartz JL, et al. R4P 2018.; 2. data on file; 3. Cottrell ML, et al. J Antimicrob Chemother 2017; 4. Anderson PL, et al. CROI 2012 16
F/TAF has a Longer Duration > EC90 After Last Dose Simulation Based on Observed TFV-DP at Steady State F/TAF F/TDF 10,000 10,000 Median TFV-DP, fmol/106 cells 1000 1000 100 100 EC90 EC90 10 10 16 days 10 days 1 1 4 8 Days Post Last Dose 12 16 20 24 28 4 8 Days Post Last Dose 12 16 20 24 28 1 1 At steady state, after the last dose, F/TAF would provide TFV-DP levels in PBMCs above EC90 for 16 days compared to 10 days with F/TDF Shading represents 5th 95th percentiles. 1. Anderson PL, et al. CROI 2012; 2. Custodio J, et al. EACS 2017; 3. Custodio J, et al. ASM 2016; 4. Hawkins J Acquir Immune Defic Syndr 2005;39:406-11. 17
Conclusions: F/TAF Has a More Rapid Onset and Longer Sustained Duration of Protection than F/TDF Noninferiority of F/TAF to F/TDF was established by the lower HIV incidence of F/TAF compared with F/TDF Risk behavior, STIs, and Adherence were similar between arms HIV prevention efficacy PK parameters differed between F/TAF vs F/TDF: TFV-DP levels in PBMCS were 6.3 fold higher with F/TAF vs F/TDF 98% in the F/TAF arm are above EC90 compared with 68% in F/TDF arm F/TAF achieved EC90 within 1 2 hrs of first dose vs 3 days of daily doses of F/TDF F/TAF expected to remain above EC90 for 16 days vs 10 days for F/TDF The more rapid onset and longer duration of protection may be the most probable explanation for the higher prevention efficacy of F/TAF F/TAF is a safer, potentially more efficacious option than F/TDF for prevention of HIV 18
BACK-UPS 19
Weight Gain in PrEP Trials HPTN 0772 (Wk 41) iPrEx1 DISCOVER p=0.66 2 2 1.5 +1.0 kg Placebo F/TDF F/TAF * * +1.1 kg F/TDF Median % Weight 1 1 Median Weight Change (SEM) +1.0 kg * Change, kg 1 * 0 0 0 kg 0.5 -1 -1 -2 0 -2 0 24 48 0 12 24 Week 36 48 CAB PBO Week *p <0.05 analysis of covariance (ANCOVA) model including baseline F/TDF for PrEP and treatment as fixed effects and baseline weight as a covariate. CAB, cabotegravir; SEM, standard error of mean. 1. Adapted from Glidden DV, et al. Clin Infect Dis 2018;67:411-9. 2. Landovitz RJ, et al. Clin Infect Dis 2019 May 24. 20
Fasting Lipid Changes From Baseline at Week 48 F/TAF F/TDF Total Cholesterol p <0.001 LDL Cholesterol p <0.001 HDL Cholesterol p <0.001 Triglycerides p=0.002 Total Cholesterol:HDL p=0.73 1 15 10 Median Change From Median Change From 0.5 4 Baseline, mg/dL 5 0.1 0.1 1 Baseline 0 0 0 -1 -2 -5 -5 -0.5 -7 -10 -11 -15 -1 173 173 99 100 49 50 93 93 3.4 3.5 Baseline, mg/dL Baseline There were minimal clinically significant changes in lipids in the F/TAF arm, with some small decreases in the F/TDF arm There was no change in the TC: HDL ratio p-values were from the 2-sided Wilcoxon rank sum test to compare the 2 treatment groups. HDL, high-density lipoprotein; LDL, low-density lipoprotein. 21