Endovascular Interventions at Mount Sinai Hospital: Case Study
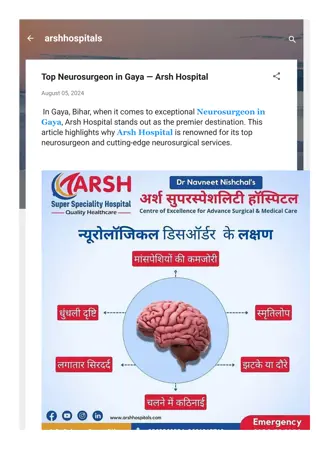
Division of Endovascular Interventions at Mount Sinai Hospital, New York, treated a 71-year-old female patient with bilateral lower extremity claudication using endovascular procedures. The patient had a history of hypertension, diabetes, hyperlipidemia, and smoking, with peripheral artery disease and prior interventions. Post-intervention imaging revealed stenosis in the right superficial femoral artery and occlusion in the left, presenting challenges in treating chronic total occlusions. The case highlights the complexities of endovascular treatment strategies for femoropopliteal disease.
- Endovascular Interventions
- Mount Sinai Hospital
- Peripheral Artery Disease
- Chronic Total Occlusions
- Femoropopliteal Disease
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Division of Endovascular Interventions Mount Sinai Hospital New York 04/22/2019
Patient history Female, 71 y/o Complains of bilateral LE claudication which progressed to resting pain (Rutherford 4) PMH: Hypertension, DM (insulin therapy), Hyperlipidemia, Smoking. PAD s/p RSFA intervention using DES (Eluvia) Medication: Lipitor, Insulin, Lisinopril, Lopressor, HCTZ, Aspirin, Clopidogrel, Glucophage. ABI: R 0.82 and Left 0.64
Non-invasive Imaging Post RSFA intervention Right: Superficial Femoral Artery: B-mode and spectral analysis is consistent with a 20-50% stenosis in the superficial femoral artery (proximal). The distal external iliac artery, common femoral artery and proximal profunda femoral artery appear patent by B-mode, color and spectral analysis without significant stenosis. Left: Superficial Femoral Artery: The superficial femoral artery (proximal) is occluded. The distal external iliac artery, common femoral artery and proximal profunda femoral artery appear patent by B-mode, color and spectral analysis without significant stenosis.
Previous angiogram ATK BTK
CTO of femoropopliteal arteries PCTOs are encountered in 40%-50% of patients presenting intermittent claudication or CLI These patients often have coexistent cardiovascular and cerebrovascular disease which increases the 5-year mortality rate by: 50% in patients with intermittent claudication 60%-70% in patients with CLI (critical limb ischemia)
Problem during PTA of Femoropopliteal Chronic Total Occlusions -Unsuccessful procedure in ~ 20 %, due to inability to reenter distal
ApproachTo FP/Tibial CTO 1. Define lesion Imaging, image analysis, CTO Classification 2. Define approach Antegrade, retrograde, hybrid 3. Define device Wire-catheter, CTO crossing device 4. Define Rx strategy Stent, non-stent Banerjee TCT 2017
Approach for endovascular treatment of femoropopliteal CTO J INVASIVE CARDIOL 2019;31(4):111-119.
Classification of CTO based on morphology J INVASIVE CARDIOL 2019;31(4):111-119.
Anticipated access Antegrade ipsilateral/ contralateral CFA Retrograde via pedal arteries
11 FP CTO Classification & Initial Crossing Approach J INVASIVE CARDIOL 2019;31(4):111-119.
Patient selection for tibiopedal access - Advanced PAD or CLI - Inability to lie flat for prolonged periods of time (severe osteoarthritis, lower back pain, CHF, COPD) - Hostile groins: morbid obesity, infected groins, severely scarred/ fibrotic groins. - Flush occlusion of the ostium of the SFA - The proximal CTO cap has an antegrade convex morphology. - Long suprapopliteal CTO
Crossing techniques and success definition J INVASIVE CARDIOL 2019;31(4):111-119.
Wire diameter selection ILIAC SFA BTK 0.014" PLATFORM Most suitable for small vessels Compatible with lowest profile balloons 0.035" PLATFORM Designed to provide highest support and stability Compatible with iliac treatment platforms 0.035" PLATFORM Designed to provide highest support & stability Compatible with most SFA balloons/stents 0.018" PLATFORM Less traumatic Well suited to distal SFA/popliteal More steerable and flexible Supports lower profile devices 0.014" PLATFORM Least traumatic Least support May be useful in some situations e.g., re-entry 0.018" PLATFORM Specific feature needed, i.e., high support, good device crossing Abbott 2017
Wire selection Connect 250T Steelcore 0.18 Command 18 LT Command 18 ST Connect Flex Connect Winn 40 Winn 200T 0.14 Command ES Spartacore Winn 80 Pedal Frontline Tortuous Anatomy Loop Calcific Lesions Maximum Delivery Support Tortuous Straight
Crossing devices (true lumen) TruePath Front Runner Crosser Crossing devices Gentle forward pressure WildCat Let device do the work Exploit micro-channels Mechanical or vibrational energy to break up calcium
Sub-Intimal Dissection with Re-Entry Enteer Pioneer Re-entry often occurs at transition to healthy vessel Outback Re-entry devices can assist this process: Outback (Cordis) Enteer (Medtronic) Off-Road Off-Road (Boston Scientific) Pioneer (Volcano)
The Constellation of FP Technologies: Nitinol Stents PTA FPA Exercise Rehab Stent Grafts Atherectomy Vessel Prep +/- DCB DES
Algorithmic Approach to FP Intervention: FP PAD Claudicant/CLI Long Lesions Ostial SFA P2-P3 Heavy calcification CTO ISR >200 mm >100 mm 200 mm 100 mm DCB DAART DCB DCB DCB DAART Limited Stenting DAART: Directional Atherectomy and Anti-Restenotic Therapy S. Banerjee TCT 2016
Bare metal stents: Supera stent studies Nitinol stent studies Vascular Health and Risk Management 2015:11
Supera stent (BMS): Source: US Supera Peripheral Stent System Instructions for US Post-hoc analysis
Strongest predictor for poor patency rate: Calcium and lesion length 12 Month Primary Patency 100%100%100% P a t e n c y 90% 90%88% 100% 80% 50% 50% 60% 40% 20% 0% 1a 1b 2a 2b 3a 3b 4a 4b Ansel, G. VIBRANT 1 year results. LINC 2010. Rocha-Singh, K. J., et al. (2015). Durability II 3 year data. CCI 86(1): 164-170. Bosiers, M., et al. (2011). DURABILITY 200. J VS 54(4): 1042-1050. Gray, W. A., et al. (2015). STROLL 1 year results. JVIR 26(1): 21-28. Laird, J. R., et al. (2012). RESILIENT 3 year results. JEVT 19(1): 1-9. Dake, M. D., et al. (2016). Zilver PTX 5 year results. Circ. Innova IFU. Garcia, L., et al. (2015). SUPERB 1 year results. Circ-CI 8(5). Ohki, T., et al. (2016). OSPREY 1 year results. JVS 63(2): 370-376 e371. Lammer, J., et al. (2011). STRIDES 1 year results. JVS 54(2): 394-401. Jaff, M. STROLL 3 year results. ISET 2014. Geraghty, P. J., et al. (2013). VIBRANT 3 year results. JVS 58(2): 386-395 e384. Minimal Calcificationa High Calcification aCalcium burden quantified with computed tomography angiography (CTA), digital subtraction angiography (DSA), and intravascular ultrasound (IVUS). Fanelli F, et al. Cardiovasc Intervent Radiol. 2014 ;37(4):898-907.
Tools for Vessel Preparation Balloons Plain Balloons Cutting Balloons Scoring Balloons Other Specialty Balloons (e.g. Chocolate PTA balloon catheter) Atherectomy Directional Orbital Rotational Laser *
Atherectomy devices for peripheral arteries with published data Circulation. 2016;134:2008 2027.
Compliance 360 (Superficial Femoral Artery) Diamondback 360 Balloon Angioplasty Average maximum balloon pressures 4.0 atms (p<0.001) 9.1 atms 30% residual stenosis without stenting 86.8% (p<0.001) 18.5% 15.8% (p=0.02) Dissections 48.1% Bail-out stenting (for residual over 30%) 5.3% (P<0.001) 77.8% Freedom from revascularization (1 yr) 81.2% (P=NS) 78.3% J Invasive Cardiol. 2014 Aug;26(8):355-60