Understanding Preterm Delivery: Causes, Complications, and Evaluation
Preterm delivery, defined as labor prior to 37 weeks of gestation, affects approximately 12% of pregnancies worldwide, with almost 30% of these deliveries occurring before 34 weeks. The etiology of preterm birth can vary from maternal factors such as PROM to fetal anomalies and multiple gestations. Neonatal complications of prematurity, including HMD, IVH, NEC, and sepsis, can have a significant impact on the infant's health. Evaluation of preterm labor involves clinical examination, cervical assessment, uterine monitoring, and ultrasound, with tests like CBC used to assess for infection and blood loss. Understanding the complexities of preterm delivery is crucial in managing and improving outcomes for both mother and baby.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
PRETERM DELIVERY PATRICK DUFF, M.D.
PRETERM DELIVERY OVERVIEW Etiology Neonatal complications Treatment
PRETERM DELIVERY Definition - labor prior to 37 weeks gestation Frequency - 12 % 500,000 preterm births annually 30% of these births are < 34 weeks
PRETERM DELIVERY IMPACT When anomalies incompatible with life are excluded, complications of preterm birth are responsible for almost 75% of all neonatal deaths
PRETERM DELIVERY ETIOLOGY PROM single most important etiology Abruptio placentae Placenta previa Uterine or cervical anomaly
PRETERM DELIVERY ETIOLOGY Fetal anomaly Polyhydramnios Systemic disease Dehydration
PRETERM DELIVERY ETIOLOGY Multiple gestation Infection lower and upper genital tract and systemic Trauma Idiopathic
NEONATAL COMPLICATIONS OF PREMATURITY HMD IVH NEC Sepsis GBS E. coli
NEONATAL COMPLICATIONS OF PREMATURITY Metabolic derangements Thermal instability Renal dysfunction PDA Apnea and bradycardia
PRETERM LABOR EVALUATION Clinical examination Cervical examination Digital and sonographic Uterine monitoring Ultrasound
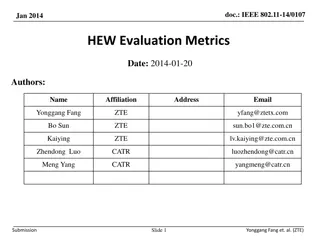
PRETERM LABOR EVALUATION TEST CBC PURPOSE WBC evaluate for infection HCT evaluate for blood loss Identify abruption Coagulation tests
PRETERM LABOR EVALUATION TEST Serology PURPOSE Evaluate for infection Identify UTI Urine culture
PRETERM LABOR EVALUATION CXR PCR for gonorrhea and chlamydia Saline microscopy for BV Culture for GBS Amniocentesis Culture Cytokines
MANAGEMENT OF PRETERM LABOR Treat underlying disorder Assess fetal well being Ultrasound FHR monitoring Doppler Evaluate for tocolysis
MANAGEMENT OF PRETERM LABOR STEROIDS Betamethasone 12 mg i.m. q 24h x 2 doses Dexamethasone 6 mg i.m. q 12h x 4 doses Effects Decrease in RDS Decrease in IVH Decrease in NEC
MANAGEMENT OF PRETERM LABOR ANTIBIOTICS INFECTION Gonorrhea TREATMENT Ceftriaxone, 250 mg i.m. plus Azithromycin, 1000 mg p.o. Azithromycin, 1000 mg p.o. Chlamydia
MANAGEMENT OF PRETERM LABOR ANTIBIOTICS INFECTION Bacterial vaginosis TREATMENT Metronidazole, 500 mg p.o. BID x 7 d Metronidazole, 2 grams p.o. x 1 Ampicillin, 2 g x 1, then 1 g Q 4h until delivery Ampicillin (2 g Q 6h) plus gentamicin (1.5 mg/kg/day) GBS Chorioamnionitis
TOCOLYTICS TERBUTALINE Mode of administration SQ, PO, or IV Dose - 0.25 mg SQ and 5 mg PO Adverse effects - cardiovascular and metabolic Rarely used today because of these side effects
TOCOLYTICS MAGNESIUM SULFATE Mode of administration - IV Dose 4 to 6 g load plus 2-4g/h, titrated to effect Provides tocolysis and neuroprotection Adverse effects Muscle weakness Visual changes Hypocalcemia
TOCOLYTICS INDOMETHACIN Mode of administration - oral Dose - 25 mg Q 6h Adverse effects Stricture of DA Oligohydramnios Should not be used after 32 weeks or for > 48 h
TOCOLYTICS NIFEDIPINE Mode of administration - oral Dose - 10 mg Q 20 minutes x 3, then 10 mg q 4 to 6h Principal adverse effect hypotension Preferred agent because of ease of administration and tolerability
PREVENTION OF PRETERM DELIVERY DRUG Progesterone vaginal suppositories Micronized progesterone tablets 17-OH P DOSING REGIMEN 100 mg daily 200 mg daily 250 mg i.m. weekly Effectiveness approximately 50%
PRETERM LABOR CONCLUSIONS Frequency 12% Multifactorial etiology Single most important cause of neonatal mortality Management Tocolytics Corticosteroids Antibiotics in selected instances Preventive measures in subsequent pregnancy