COVID-19 Response and Vaccination Impact in Victorian Health Unit
In the COVID-19 Employee Forum by Rhonda L. Stuart from Monash Health South Eastern Public Health Unit, various aspects like the current state, data from the last 6 months, and hospitalizations are discussed. It also highlights the effects of vaccination in preventing hospitalizations, ICU admissions, and deaths. The presentation delves into the next phase of the Victorian COVID-19 response, emphasizing the importance of vaccination and the roadmap for opening up. Additionally, the approach to case and contact management, including quarantine guidelines and testing procedures, is detailed.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
COVID-19 Employee Forum Rhonda L Stuart Monash Health South Eastern Public Health Unit
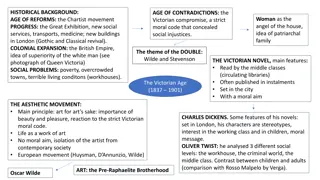
Effect of Vaccination 100 90 80 70 60 50 40 30 20 10 0 Hospitalised Admitted to ICU Total deaths Not vaccinated Partially Vaccinated Double Vaccinated
Next Phase of the Victorian COVID-19 Response To From 90%+ Vaccinated No Vaccination National Plan & Roadmap to Opening Up (Living with COVID) Reactive Lockdowns & COVID Zero Self Sufficient & Individual Responsibility Government Directed Rules & Restrictions Pandemic Legislation & Readiness Emergency Management & Powers Empowerment and Public Health Education Control
Approach to Case and Contact Management Continue to mandate households and household-like contacts of positive cases to quarantine for 7 days (vaccinated includes 0 11-year-olds) or 14 days (unvaccinated) Continue to contact positive cases and mandate to isolate for ten days (community) 1 2 Includes support around COVID positive pathways, welfare relief and enforcement Close contacts Recommended use of RAT workplace and school contacts in the 7 days since exposure, particularly before attending a sensitive setting Cases Plan 4 3 Required to get a PCR test and quarantine until receiving a negative result; no further quarantine requirements regardless of vaccination status Advised (by the case) to get a PCR test and isolate until a negative result with no further quarantine requirements, regardless of vaccination status Workplace/ School contacts Social contacts Recommended use of RAT workplace and school contacts in the 7 days since exposure, particularly before attending a sensitive setting
Contact Definitions Close Contact An individual that resides or stays overnight in the same premises as a confirmed case or has had a total of four or more hours of contact (cumulative) in a residential setting during their infectious period. A close contact can also be designated by an LPHU director/Med lead, DCHO or CHO for example in the context of an outbreak.
Workplace and Education Contact Defined as an individual who does not meet the close contact definition and who in any workplace or education facility - has had: at least 15 minutes face to face contact, or greater than 2 hours within the same room* with a confirmed case of COVID-19 *Same room refers to a smaller indoor space (<100m2), for example a classroom or shared office.
Social Contact Defined as an individual who does not meet the close contact definition and who outside a workplace or education facility has had: at least 15 minutes face to face contact, or greater than 2 hours within the same room with a confirmed case of COVID-19 during their infectious period.
Exposed Person An individual who may have been exposed to a confirmed case of COVID-19 at a higher risk non-sensitive setting as identified via the Service Victoria Digital Visitation Register (DVR) system.
HCW quarantine requirements Hospital Requirement Community Requirement COVID Positive HCW 10 days furlough 10 days isolation Household (HH) contact 7 days furlough, neg PCR D6 7 days quarantine Non-HH contact Surveillance testing neg PCR D6 Nil High risk internal exposure (red) 7 days furlough, neg PCR D6 Nil Low risk internal exposure (yellow) Surveillance testing neg PCR D6 Nil International Travel 7 days furlough, neg PCR D6 Nil
Patient quarantine requirements Patient and Healthcare exposure type Management in Hospital Community Requirement Vaccinated Patient High risk exposure = Household-like contact (> 4 hours in same room/area) 7 days isolation Tier 3 precautions neg PCR D6 7 days quarantine neg PCR D6 Unvaccinated Patient High risk exposure = Household-like contact (> 4 hours in same room/area) 14 days isolation Tier 3 precautions neg PCR D13 14 days quarantine neg PCR D13 Vaccinated Patient Low risk exposure = non-household-like contact (< 4 hours in same room/area) 7 days isolation Tier 3 precautions neg PCR D6 Nil quarantine Unvaccinated Patient Low risk exposure = non-household-like contact (< 4 hours in same room/area) 14 days isolation Tier 3 precautions neg PCR D13 Nil quarantine
International Travel Staff Patients Visitors Vaccinated Leave sCOVID for 7 days plus negative test D6 Cannot enter for 7 days plus negative test D6 7 days plus negative test D6 Exempt Leave sCOVID for 14 days plus negative test D13 Cannot enter for 14 days plus negative test D13 14 days plus negative test D13 Unvaccinated N/A sCOVID for 14 days plus negative test D13 Not permitted (except under compassionate grounds)
HCW surveillance testing background Healthcare settings high-risk for COVID-19 outbreaks, transmission, and exposure of vulnerable Asymptomatic surveillance testing of HCW - assist early detection to minimise/prevent outbreaks HCW are at risk of infection from COVID-19 patients/staff and when community prevalence is high With the current level of community transmission, main risk for HCW is community/household Primary objective of HCW surveillance is for early identification of infected HCW to reduce the risk of onward transmission to other HCW and patients. Surveillance can help identify HCW who have an asymptomatic or pre-symptomatic infection As at 11 November 2021 the guidance on HCW surveillance testing by the Department of Health was revised in recognition of levels of community transmission meaning increased risk of HCW to HCW and HCW to patient transmission as a result of community and household exposures for HCW, high levels of vaccination and PPE use, the need for sustainable levels of laboratory testing, and the introduction of rapid antigen testing as an option for asymptomatic surveillance.
New HCW surveillance Cohort Testing Symptomatic HCW PCR on nose-throat specimen 3 x week PCR saliva ( < 72 hours between tests) Asymptomatic HCW For covid wards, ED, ICU and after an exposure event Simpler Maintains sensitivity and frequency Wait more guidance on RATs Testing as per the regime defined in the HCW contact assessment and management guidance for PCCs. HCW following exposure event