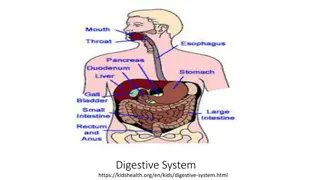
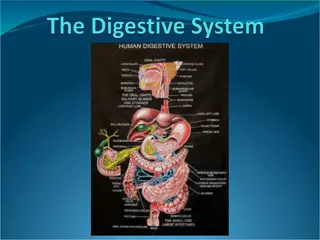
Understanding the Human Digestive System
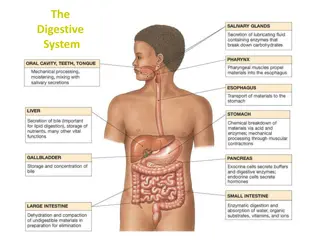
The human digestive system is a complex pathway that starts from the mouth and ends at the anus, involving various organs like the mouth, pharynx, esophagus, and stomach. Each part plays a crucial role in breaking down food particles, absorbing nutrients, and eliminating waste products. From chewing in the mouth to peristalsis in the esophagus and gastric motility in the stomach, each step is essential for proper digestion and nutrient absorption.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Gastrointestinal System NUR 194 'The human digestive system' illustration for About Science Book 3 by Science Press Source:http://www.labyrinth.net.au/~daviddic/dig estion.jpg
Quick Review: A&P GI tract 25 ft pathway from mouth to anus Function of GI tract: Break down food particles into molecules for digestion Absorb into the bloodstream the small molecules produced by digestion Eliminate undigested and unabsorbed foodstuffs and other waste products from the body
Mouth Food entry Process of digestion begins with chewing (mastication) to break down foods into small particles that can be swallowed and mixed with digestive enzymes Saliva: First secretion that comes in contact with food; contains water and mucus; lubricant for swallowing Contains salivary amylase (enzyme: ptyalin) digests starches Produced in 3 pairs of glands: parotid, submaxillary, and sublingual. Approx. 1L of saliva is produced daily
Pharynx The pharynx or throat extends from the soft palate to the esophagus. It is lined with mucous membrane and contains 3 pairs of organs: the adenoids, the lingual tonsils, and the tonsils.
Esophagus Responsible for food passage from mouth to stomach Distends Smooth muscle contracts in rhythmic sequence (peristalsis) from upper esophagus to stomach to propel food along Upper Esophageal Sphincter (UES) (entry). Closed at rest to prevent air entering the esophagus during respiration. passes through diaphragm at opening called diaphragmatic hiatus Lower esophageal sphincter (LES)relaxes to allow food to enter stomach then closes tightly to prevent reflux of stomach contents back into esophagus. about 24cm or 10 inches long
Stomach Lined with smooth muscle that promotes gastric motility. Expandable pouch, stores and mixes food with secretions; holds approx. 1500ml Parietal cells line wall and secrete hydrochloric acid (HCl) Breaks down food Kills most ingested bacteria Gastric secretions contain pepsin for protein digestion Gastric mucosa secretes intrinsic factor to combine with Vitamin B12 in food to be absorbed in ileum Parietal cells also produce intrinsic factor, which works to facilitate the absorption of Vit B12. Absence of the intrinsic factor causes pernicious anemia. Chyme: food particles mixed with gastric secretions
Stomach Inlet: esophagogastric junction surrounded by smooth muscle (lower esophageal sphincter or cardiac sphincter) which contracts and closes off stomach from esophagus 4 anatomic regions: Cardia (entrance) Fundus Body or corpus Pylorus or antrum: outlet Outlet: Pyloric sphincter circular smooth muscle that controls the opening of the stomach to the intestine
3 phases of gastric secretion Cephalic- begins with sight, smell, and taste of food and is regulated by the vagus nerve. Gastric- begins with the presence of food in the stomach. Intestinal- begins as the chyme passes from the stomach into the duodenum, causing distention. Secretin : a hormone that inhibits further acid production and decreases gastric motility.
Pancreas Gland that lies behind the stomach and extends to the spleen 2 cellular bodies within Pancreas: Exocrine: 80% of the organ and cells secrete enzymes needed for digestion of carbohydrates, fats, and proteins (trypsin, chymotrypsin, amylase and lipase Endocrine- produces glucagon & insulin.
Liver Largest organ of body other than skin Located in RUQ of abdomen. Primary functions: Forms & secretes bile which is necessary for fat breakdown. Bile empties into the duodenum at sphincter of Oddi. If sphincter is closed, the bile is stored in the gallbladder.
Small Intestine Longest segment about 2/3 the total length of GI tract Approx 7000 cm of surface area for secretion and absorption (the process by which nutrients enter bloodstream through intestinal wall --primary fx of small intestine). 3 anatomic parts: Duodenum (upper) Sphincter of Oddi Jejunum (middle) Ileum (lower) Cecum: junction between small and large intestine; ileocecal valve controls passage of contents into large intestine & prevents reflux of bacteria into small intestine. Appendix located at junction of small and large intestine
Small intestine The common bile duct and pancreatic duct join to form the ampulla of Vater, emptying into the duodenum at the duodenal papilla. This papillary opening is surrounded by muscle known as the sphincter of Oddi. Sphincter of Oddi leads to the jejunum.
Small Intestine Duodenum: contains intestinal glands & receives secretions from pancreas, liver, and gallbladder that aid in digestion (contain enzymes and bile) Intestinal glands: secrete mucus, electrolytes, and enzymes: Coat cells and protect mucosa from HCl Hormones, neuroregulators, and local regulators control rate of secretion production; influence GI motility Pancreas: Secretions have alkaline pH due to high bicarbonate concentration; neutralizes acid entering from stomach Digestive enzymes: Trypsin (protein digestion); Amylase (starch); lipase (fats) Liver: secretes bile (emulsify fats making them easier to digest and absorb) know all functions of the liver Chapter 55 Gallbladder: Bile storage Two types of contractions- stimulated by presence of chyme Segmentation: mixing waves; churns Intestinal peristalsis: propels contents of small intestine to colon Vitamins and minerals: absorbed essentially unchanged Absorption begins in jejunum diffusion and active transport
Large Intestine Functions: movement, continuation of absorption and beginning of elimination Ileocecal valve allows passage of residual waste material from terminal ileum into proximal colon restricts reflux of contents back into ileum, Bacteria is major component of large intestine 2 colonic secretions: an electrolyte solution (bicarb to neutralize) and mucus (protects mucosa and provides adherence of fecal mass) Waste materials reach and distend rectum in about 12 hours
Large Intestine Components: Begins at cecum. Ascending segment (R-side of abdomen) Transverse (right to left of upper abdomen) Descending segment (L side of abdomen) Terminal portion: sigmoid and anus Anus -- striated muscles form internal and external anal sphincters
Waste Products Feces 75% fluid, 25% solid materials: foodstuffs, inorganic materials, water and bacteria Brown color comes from breakdown of bile Chemicals formed by bacteria are largely responsible for odor Approx 150 ml of gases are contained in GI tract: methane; hydrogen sulfide; and ammonia either absorbed into portal circulation and detoxified by liver, or expelled through rectum as flatus Process of elimination: Stimulation of rectum causes rectal distention which reflexively initiates contraction of rectal muscles causing the internal anal sphincter to relax (autonomic nervous system). The external anal sphincter is under conscious control of the cerebral cortex once allowed to relax will allow contents to be expelled. Contraction of the abdominal muscles (bearing down or straining) facilitates the emptying of the colon. Average frequency of defecation: once a day, but varies among individuals
GI Changes with Aging Stomach: Decreased gastric HCL -Atrophic gastritis due to bacterial overgrowth Encourage bland foods high in vitamins & iron Assess for epigastric pain Large Intestine: Decreased peristalsis Constipation & Impaction High fiber diet Increased fluid intake (1500ml) if not contraindicated Encourage activity as tolerated Pancreas: Pancreatic duct change Steatorrhea: excess fat in stool. Small frequent feedings Assess for diarrhea Liver: Decreased enzyme activity & cholesterol synthesis Depresses drug metabolism leading to accumulation of drug and possible toxicity Assess for adverse effects of drugs Know Chart 55-1
Assessment Take a complete history; focus on symptoms common to GI dysfunction Read Gordon s functional health patterns-Chart 55-2 Family & Genetic HX * Ex: Familial adenomatous Polyposos(FAP)-rpedisposition to colon cancer Previous hx of GI disease Past and current medication use. Including OTC & herbal products Previous or current treatments Previous surgeries Nutritional/Dietary hx: Food Allergies Tobacco and alcohol use Changes in appetite or eating patterns Anorexia (loss of appetite for food); dysphagia (difficulty swallowing); N/V; dyspepsia (indigestion/heartburn) Unexplained weight gain or loss Stool characteristics Socioeconomic, psychosocial, spiritual, or cultural factors Cultural: food restrictions, use of ingredients. Fasting 80-90% African Americans are lactose intolerant. Lack of enzyme lactase which converts dairy to glucose and galactose. (s/s: bloating, cramping, diarrhea) PE: Abdominal girth; tenderness/guarding; rectal exam; pelvic exam Diagnostics: CBC, urinalysis, abdominal x-rays, EKG, pregnancy test for the female
PQRST P: precipitating or palliative Q: quality or quantity R: region or radiation S: severity scale T: timing
Symptoms Common to GI Dysfunction Pain: can be major symptom; assess character, frequency, location, pattern, time of pain be aware of common sites of referred pain Indigestion: Upper abdominal discomfort or distress; most common symptom; Peristaltic activity may be contributing; BMs may or may not relieve pain. Fatty foods often perpetrator remain in stomach longer. Coarse vegetables and highly seasoned foods may cause distress.
Symptoms Intestinal Gas: Accumulation of gas may leading to belching (expulsion from stomach thorough mouth) or flatus (from rectum) Complaint of bloating, distension, or full of gas Excessive flatulence may be a symptom of gallbladder disease or food intolerance. Nausea and Vomiting: Nausea : usually triggered by odors, activity, or food intake Emesis may vary in color and content; may contain undigested food particles or blood (hematemesis). Blood: If bright red signal of hemorrhage; if dark or has coffee-ground appearance it has been subjected to gastric enzymes
Symptoms Change in Bowel Habits and Stool Characteristics May signal colon disease Diarrhea: abnormal increase in frequency or liquidity of stool Constipation: decrease in frequency of stools; stools that are hard, dry, or of smaller volume than normal
Symptoms Stool Characteristics color and appearance Color: can be affected by foods or meds Blood: can present in several ways Tarry-black: blood shed in upper GI tract Bright red: blood enters in lower portion of GI Dark red: passing rapidly through GI tract Streaking of blood on surface of stool/toilet tissue: may be lower rectal or anal bleeding Common abnormalities of stool: Bulky, greasy, foamy; foul in odor; gray with silvery sheen Light gray or clay-colored caused by absence of urobilin Mucus threads or pus visible on gross inspection Small, dry, rock-hard masses called scybala may be streaked with blood from rectal trauma during passage Loose, watery stool that may or may not be streaked with blood
Physical Assessment Examination includes: Mouth: tongue, buccal mucosa, teeth, gums note any ulcerations, nodules, swelling, inflammation; color changes Abdomen Rectum - anal and perineal areas: rash or excoriation; fissures or fistulas; hemorrhoids. Digital exam: masses or tender areas Performance of the exam must be followed in this order so intestinal activity & bowel sounds are not increased prior to exam. Inspection Auscultation Percussion Palpation
Inspection Skin changes May result from GI Tract disorders such as liver and biliary obstructions Scars trauma, previous surgeries Contour and symmetry Bulging Distension Peristaltic waves Cullen s sign
Auscultation Bowel Sounds all 4 quads using the diaphragm of the stethoscope (best for high-pitch and gurgling): Increased bowel sounds-borborygmus Character Location Frequency Normal sound is heard every 5 to 20 seconds Hypoactive one or two sounds heard in 2 minute period Hyperactive: 5 to 6 sounds heard in less than 30 seconds Absent: No sounds heard in 3 to 5 minutes BRUITS
Percussion and Palpation Percussion: Tympany (high pitched) or dullness Palpation: 2 types: Light: detects large masses & areas of tenderness. Rebound tenderness (Blumberg s sign-used to further evaluate areas of pain). : exert pressure over an area and release quickly is there pain on withdrawal of pressure? If so, report to health care provider. Note any areas of tenderness or guarding for further evaluation during deep palpation. If rigidity noted, indicative of peritoneal inflammation. Deep: identify masses in 4 quads. Current practice is that only MD or APN s perform deep palpation. Used to determine size & shape of organs & masses.
Diagnostics Blood Tests: CBC, PT, Carcinoembryonic antigen (CEA and the CA19-9); total calcium, Potassium, Albumin levels AST, ALT, amylase and lipase bilirubin, ammonia. Serum Cholesterol and Triglycerides Urine Tests: amylase; urobilinogon Stool Tests ( FOBT)-Fecal Occult Blood Test , FIT, Stool samples for ova/ parasites; stool test for clostridium difficile Know: Labs: Chart 55-3 for normal ranges
Diagnostics contd Abdominal Ultrasound Plain films of the abdomen Upper GI Study Lower GI study PTC CT
Endoscopy Endoscopy: direct visualization of GI tract with a flexible fiberoptic endoscope. Used to evaluate bleeding, ulceration, inflammation, tumors, and cancer of esophagus, stomach, biliary system, or bowel. May obtain specimans for biopsy or studies (H.pylori). Requires Informed consent by patient prior to procedure. EGD- examines esophagus, stomach & duodenum. May be used to dilate an esophageal stricture (during procedure) ERCP- includes exam of liver, gallbladder, bile ducts, and pancreas to identify cause & location of obstruction(s). Uses contrast so x-rays may be obtained. May obtain biopsies, or remove gallstones.Lasts 30 minutes to 2 hours. Reqiures Iv access for moderate sedation drugs and contrast.
Colonoscopy Colonoscopy: endoscopic exam of entire large bowel.. Recommended every 10 years for all persons age 50+. More frequently if family hx of colon cancer. Evaluates for causes of chronic diarrhea, source of GI bleeding. Prep: Clear liquid diet 12-24 hours prior to procedure. NPO 6-8 hours prior may have water. Avoid aspirin, NSAIDS, and anticoagulants (with MD order) for several days Diabetic patients should check With MD re: diabetic meds as pt is NPO Night before procedure, Pt drinks Sodium Phosphate (Phospho-Soda) to clean bowel. May be repeated the morning of procedure. May prescribe Go-Lytely as a bowel cleanser the day before as well. Chill drinks to improve taste. Have pt drink quickly to avoid N/V. Watery diarrhea begins in about 1 hour. Additional laxatives or cleansing enemas may be required. Procedure: IV access for moderate sedation. Versed. Air is instilled to prmoote better viewing. Endoscopy passed through rectum to cecum. Atropine Sulfate : available in case of bradycardia from vasovagal response. After-Care: NPO until sedation wear off and pt is fully alert. VS every 15 minutes until pt is stable. Siderails up until Pt fully alert. Monitor for rectal bleeding or pain. May expect abdominal cramping for several hours. Monitor for bowel perforation, hypovolemic shock. Chart 55-4.
Tests cont. Gastric Analysis, Gastric Acid Stimulation Test(Histolog), pH monitoring Ultrasonography, Endoscopic ultrasonography Liver-spleen scan
The nurses role Is to prepare the client, explain the procedure, and provide the necessary post procedure care. Read and know the procedures so you can explain them to the client.
Oral and Esophageal Disorders Chapter 56 Examining the Lips, Mouth, and Gums: Examples of Lip Conditions : lips-ppd-s herpes%25202 Cold Sore Chancre Contact Dermititis
Stomatitis/Candidiasis Stomatitis is a painful ulceration of the oral mucosa that appear as inflammation and denudation of the oral mucosa, known as canker sores Candidiasis is a fungal/yeast infection resulting from an overgrowth of normal flora. Type of secondary stomatitis. Overgrowth may be caused by long term antibiotic use, chemotherapy, radiation, and HIV. White plaque on tongue. Red and painful underneath.
Mouth Candidiasis Hairy Leukoplakia Lichen planus
Mouth and Gums Aphthous Stomatitis (Canker Sore) Periodontitis
Salivary Glands Acute Sialadenitis: Inflammation of salivary glands Causes: dehydration; radiation therapy, malnutrition, improper oral hygiene. Invasion of staph a.; streptococcus viridans;or pneumococcus S/Sx: Pain, swelling, purulent discharge Tx: Antibiotics; massage, hydration, corticosteroids; surgery to drain; analgesics, warm compresses, use of lemon slices & fruit/citrus flavor candy to stimulate saliva Best prevented by good routine oral hygiene. Xerostomia-very dry mouth . Usually caused by exposure of glands to radiation.
Esophagus Chapter 57 Dysphagia: difficulty swallowing Most common symptom of esophageal disease Odynophagia: acute pain on swallowing Motility disorders: Achalasia: rare disorder. absent or ineffective peristalsis; accompanied by the esophageal sphincter that fails to relax during swallowing resulting in sensation of food sticking in lower esophagus. Diffuse spasm: Motor disorder with unknown cause; stress produces contractions of the esophagus
Esophagus Gastroesophageal Reflux Disease (GERD) Caused by an incompetent lower esophageal sphincter, pyloric stenosis, or a motility disorder that allows backflow of gastric or duodenal contents S/Sx: Pyrosis (burning sensation in the esophagus); dyspepsia (indigestion); regurgitation; dysphagia; odynophagia- Chart 57-1 & Table 57-1 Tx: Low-fat diet; avoid caffeine, tobacco, beer, milk; peppermint/spearmint; carbonated beverages; avoid eating 3 hours before bedtime; maintain a healthy weight; avoid tight- fitting clothes; elevated head and/or HOB; surgical intervention for severe cases not responding to medical intervention. Chart 57-2
GERD Tx: Meds: Antacids; Histamine receptor blockers (prevent or block the production of gastric acid): Cimetidine (Tagamet); Famotidine (Pepcid); Nizatidine (Axid); Ranitidine (Zantac) Proton Pump Inhibitors (decrease gastric acid production): Prevacid (lansoprazole), Aciphex (rabeprazole); Prilosec (Omeprazole); Nexium (esomeprazole magnesium) Prokinetic Agents (accelerate gastric emptying): Urecholine (bethanechol); Motililium (domperidone) and Reglan (metroclopramide) Untreated GERD can lead to Barrett s Esophagus a precancerous condition
Esophagus Hiatal Hernia: opening in the diaphragm (through which the esophagus passes) becomes enlarged and the upper part of the stomach moves up into the lower part of the thorax. 2 major types: Sliding HiatalHernia Heartburn, regugitation, chest pain, dyshapgia, belching Paraesophageal Hernia Feels full after eating, breathless after eating, feeling of suffocation, chest pain mimics angina, s/s worse in recumbent position. Diverticulum: (Of esophagus). Herniation of mucosa into surrounding tissue. S/S: dysphagia, reflux, bad breath, nocturnal cough.DX by EGD. Small meals of semisoft foods, elevate HOB. May require surgical removal:
Gastric Disorders-Chapter 58 Gastritis: inflammation of the gastric (stomach) mucosa; membranes become edematous and hyperemic (congested with fluid and blood) and begin to erode. Leads to ulceration and a potential for hemorrhage Acute: lasts hours to a few days; infection with Helicobactor pylori. usually caused by eating contaminated foods; highly seasoned foods; overuse of aspirin or NSAIDs; excessive alcohol intake; bile reflux; radiation therapy; or the ingestion of a strong acid or alkali. S/Sx: Acute: abdominal pain; headache; N&V; anorexia; hiccoughing Tx: Usually self-limiting; mucosa able to repair itself; refrain from food and alcohol until resolved; non-irritating diet during recovery; IV fluids. Acids or alkalis: dilution and neutralization; acids (common antacids), alkali (diluted vinegar or lemon juice)
Gastric Disorders Gastritis: Chronic: repeated exposure to irritating agents; recurring episodes of acute gastritis Causes: Prolonged inflammation-- benign or malignant ulcers; bacteria Helicobacter pylori; autoimmune diseases (pernicious anemia) B12 deficiency; caffeine; medications; alcohol; smoking; reflux of intestinal contents. S/Sx: anorexia; heartburn; belching; N&V; sour taste in the mouth Tx: Modify diet; promote rest; reduce stress; pharmacotherapy antibiotics; proton pump inhibitors; bismuth salts (Pepto-Bismol).
Gastric and Duodenal Ulcers Peptic Ulcer: musocsal lesion of the stomach or duodenum. Peptic Ulcer Disease (PUD): occurs when mucosal defenses are impaired and no longer protect the epithelium from the effects of acid and pepsin. Types of Peptic Ulcers: Gastric: occurs when break in mucosal barrier and HCL acid injuries lining. Delays gastric emptying resulting in regurgitation of duodenal contents. Deep & penetrating ulcers. Duodenal: chronic break in duodenal mucosa and leaves a scar after healing. High gastric acid secretion.. Most common ulcer. Stress Ulcers: acute lesions that occur after an acute medical crisis or trauma. Gastritis may lead to stress ulcers. Review Table 58-2
Gastric and Duodenal Ulcers Stress and anxiety formerly thought to be the cause Caused by infection with gram-negative bacteria Helicobacter pylori Familial tendency may predispose; Blood Type O at greater risk; also associated with chronic pulmonary disease or chronic renal disease Associated with chronic use of NSAIDs, alcohol ingestion, and excessive smoking
Gastric and Duodenal Ulcers S/Sx: May come and go; days to weeks to months and then disappear then reappear often without identifiable cause Dull, gnawing pain; usually relieved with eating Burning sensation in midepigastrium or back Pyrosis (heartburn); belching N&V (vomiting usually is indicative of complication and often follows a bout of pain and bloating; usually consists of undigested food ) Constipation or diarrhea (usually as a result of medication or diet regimen)
Gastric and Duodenal Ulcers Assessment: Pain and epigastric tenderness; abdominal distention Diagnostics: Barium study of Upper GI; Endoscopy; Stool testing for occult blood; biopsy and histology with culture, breath test, or serological testing for H. pylori Tx:Medications:Antibiotics for h. pylori; histamine 2 (H2) receptor antagonists; proton-pump inhibitors for ulcers not associated with h. pylori. Also, lifestyle changes and surgical intervention Surgical Intervention read p.1278
Nursing Considerations Relieving pain: meds; avoid aspirin, caffeine; regular meals; relaxation techniques to manage stress and pain; smoking cessation Reduce anxiety: Answer questions, explain diagnostic tests; administer meds on schedule; encourage family support. Maintain optimal nutrition: Assess for malnutrition and wt loss; teach about importance of complying with med and dietary regimen. Promote self-care teach clients to manage disease and factors that help or aggravate; medication regimen; dietary considerations; smoking cessation