Understanding Carbohydrate Digestion and Absorption
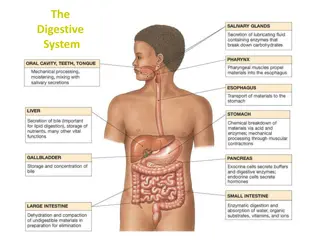
Carbohydrate digestion begins in the mouth with the release of salivary amylase, continues in the stomach where chyme is formed, and is completed in the small intestine with the help of pancreatic enzymes. Absorption of the broken-down sugars occurs in the small intestine, while undigested carbohydrates reach the large intestine where they are processed by intestinal bacteria.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
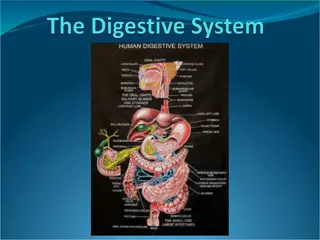
Digestion and absorption
Digestion of carbohydrate:The main function of carbohydrates is to provide your body with energy to support muscular work, brain activity, breathing and other important activities. Carbohydrates are made up of sugars known carbohydrate foods contain many saccharides linked together, which are known as polysaccharides. Carbohydrate digestion begins in the mouth and is complete when the polysaccharides are broken down into single sugars, or monosaccharides, which can be absorbed by the body. as saccharides. Most
Digestion of carbohydrates : Mouth Carbohydrate digestion begins in the mouth. The salivary glands in the mouth secrete saliva, which helps to moisten the food. The food is then chewed while the salivary glands also release the enzyme salivary amylase, which begins the process of breaking down the polysaccharides in the carbohydrate food and converting it to maltose or isomaltose.
Stomach After the carbohydrate food is chewed into smaller pieces and mixed with salivary amylase and other salivary juices, it is swallowed and passed through the esophagus. The mixture enters the stomach where it is known as chyme. There is no further digestion of chyme, as the stomach produces acid which destroys bacteria in the food and stops the action of the salivary amylase.
Pancreas and Small Intestine After being in the stomach, the chyme enters the beginning portion of the small intestine, or the duodenum. In response to chyme being in the duodenum, the pancreas releases the enzyme pancreatic amylase, which breaks the polysaccharide down into a disaccharide, a chain of of only two sugars linked together. The small intestine then produces enzymes called lactase, sucrase and maltase, which break down the disaccharides into monosaccharides. The monosaccharides are single sugars that are then absorbed in the small intestine.
Large Intestine (Colon) Carbohydrates that were not digested and absorbed by the small intestine reach the colon where they are partly broken down by intestinal bacteria. Cellulose ,Fiber, which cannot be digested like other carbohydrates, is excreted with feces or partly digested by the intestinal bacteria.
Absorption of Carbohydrates Essentially all the carbohydrates in the food are absorbed in the form of monosaccharides; only a small fraction are absorbed as disaccharides and almost none as larger carbohydrate compounds. By far the most abundant of the absorbed monosaccharides is glucose, usually accounting for more than 80 percent of carbohydrate calories absorbed. The reason for this is that glucose is the final digestion product of our most abundant carbohydrate food, the starches. The remaining 20 per cent of absorbed monosaccharides are composed galactose and fructose, the galactose derived from milk and the fructose as one of the monosaccharides digested from cane sugar. almost entirely of
Glucose Is Transported by a Sodium Co- Transport Mechanism., Galactose is transported by almost exactly the same mechanism as glucose. Conversely, fructose transport does not occur by the sodium co-transport mechanism. Instead, fructose is transported by facilitated diffusion all the way through the intestinal epithelium but not coupled with sodium transport. Much of the fructose, on entering the cell, becomes phosphorylated, then converted to glucose, and finally transported in the form of glucose the rest of the way into the blood..
Fate of absorbed sugars: Monosaccharides (glucose, galactose and fructose) resulting from carbohydrate digestion are absorbed and undergo the following: A. Uptake by tissues (liver): After absorption the liver takes up sugars, where galactose and fructose are converted into glucose. B. Glucose utilization by tissues: Glucose may undergo one of the following fate:
1. Oxidation: through a) Major pathways (glycolysis and Krebs' cycle) for production of energy. b) Hexose monophosphate pathway: for production of ribose, deoxyribose and NADH + H+ c) Uronic acid pathway, for production of glucuronic acid, which is used in detoxification and enters in the formation of mucopolysaccharide.
2. Storage: in the form of: a) Glycogen: glycogenesis. b) Fat: lipogenesis. 3. Conversion: to substances of biological importance: a) Ribose, deoxyribose RNA and DNA. b) Lactose milk. c) Glucosamine, galactosamine mucopolysaccharides. d) Glucoronic acid mucopolysaccharides. e) Fructose in semen.
Digestion and Absorption of Proteins Protein digestion begins in the stomach with the action of pepsin. Some amino acids are liberated in the stomach, but the major products of pepsin digestion are short-chain polypeptides, Pepsin digestion helps to produce a more homogenous chyme, but it is not essential for the complete digestion of protein that occurs even in people with total gastrectomies in the small intestine.
Most protein digestion occurs in the duodenum and jejunum. The pancreatic chymotrypsin, and elastase cleave peptide bonds in the interior of the polypeptide chains. These enzymes are thus grouped together as endopeptidases. Enzymes that remove amino acids from the ends of polypeptide chains, by contrast, are exopeptidases. These include the pancreatic juice enzyme removes amino acids from the carboxyl-terminal end of polypeptide chains, and the brush border enzyme aminopeptidase, Aminopeptidase cleaves amino acids from the amino-terminal end of polypeptide chains. juice enzymes trypsin, carboxypeptidase, which
As a result of the action of these enzymes, polypeptide chains are digested into free amino acids, dipeptides, and tripeptides. The free amino acids are absorbed by cotransport with Na+ into the epithelial cells and secreted into blood capillaries. The dipeptides and tripeptides enter epithelial cells by the action of a single membrane carrier . This carrier functions in secondary active transport using a H+ gradient to transport dipeptides and tripeptides into the cell cytoplasm. Within the cytoplasm, the dipeptides and tripeptides are hydrolyzed into free amino acids, which are then secreted into the blood .
The rate of action of these protein digestive enzymes is influenced by a number of factors. Some of them are concentration and amount of the enzyme, amount of protein food needed to be digested, temperature of the food, acidity of the food, acidity of the stomach and presence of antacids or other inhibitors of digestion. They leave the stomach and enter the small intestine with the help of peristalsis movement of the body. The entire process of protein digestion in the stomach takes about 4 hours.
http://images.flatworldknowledge.com/ballgob/ballgob-fig20_006.jpghttp://images.flatworldknowledge.com/ballgob/ballgob-fig20_006.jpg
Fate of aminoacids: 1- protein synthesis:- One possible fate of absorbed amino acids is to become incorporated into a new protein. the cells create new proteins as needed, determined by chemical signals within the cells that direct the genes to specify the order of amino acids required for that particular protein. Individual amino acids join together in a specific sequence, with the amino group of one linking to the carboxyl group of the next. When all necessary amino acids have joined together in this manner, the different R-groups interact to cause the protein to take on a certain conformation. For example, some R-groups may cause the amino acid chain to twist into a spiral or to fold into a sheet, causing the protein to take on a specific shape.
2-Metabolism If not needed for protein synthesis, amino acids can take part in metabolism. the body has the ability to manufacture a subset of amino acids, known as non-essential because the body don t have an absolute requirement for them in the diet. the cells can make non-essential amino acids by modifying other amino acids or from what's left over after excess amino acids are broken down. The body can also break down amino acids and use their components either as a fuel source for the cells or as a precursor to fatty acids that then store in adipose tissue.
There are 20 amino acids that can be part of proteins. Nine amino acids are essential for adults, meaning that you must get them from food since your body is unable to produce them. Essential amino acids include histidine, isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan and valine. Eleven amino acids are nonessential. Your body gets non-essential amino acids either from essential amino nonessential amino acids or from food. Nonessential amino acids for adults include alanine, arginine, asparagine, aspartic acid, cysteine, glutamic acid, glutamine, glycine, proline, acids that produce serine and tyrosine.
Digestion and Absorption of Lipids The salivary glands (newborns) produce lipases. In adults, however, very little lipid digestion occurs until the lipid globules in chyme arrive in the duodenum. the arrival of lipids (primarily triglyceride, or fat) in the duodenum serves as a stimulus for the secretion of bile. In a process called emulsification, bile salt micelles are secreted into the duodenum and act to break up the fat droplets into tiny emulsification triglycerides. Note that emulsification is not chemical digestion the bonds joining glycerol and fatty acids are not hydrolyzed by this process. and stomach of neonates droplets of
Digestion of Lipids The emulsification of fat aids digestion because the smaller and more numerous emulsification droplets present a greater surface area than the unemulsified fat droplets that originally entered the duodenum. Fat digestion occurs at the surface of the droplets through the enzymatic action of pancreatic lipase, which is aided in its action by a protein called colipase (also secreted by the pancreas) that coats the emulsification droplets and anchors the lipase enzyme to them. Through hydrolysis, lipase removes two of the three fatty acids from each triglyceride molecule and thus liberates free fatty acids and monoglycerides .
Free fatty acids, monoglycerides, and lysolecithin, which are more polar than the undigested lipids, quickly become associated with micelles of bile salts, lecithin, and cholesterol to form mixed micelles These micelles then move to the brush border of the intestinal epithelium where absorption occurs. http://t1.gstatic.com/images?q=tbn:ANd9GcRyvZJG3FPMPzxH8iwIuwXKR1iLw-UnuS_nPfFjYPPw5kmToC4ohQ
Absorption of Lipids Free fatty acids, monoglycerides, and lysolecithin can leave the micelles and pass through the membrane of the microvilli to enter the intestinal epithelial cells. There is also some evidence that the micelles may be transported intact into the epithelial cells and that the lipid digestion products may be removed intracellularly from the micelles. In either event, these products are used to resynthesize triglycerides and phospholipids within the epithelial cells. This process is different from the absorption monosaccharides, which pass through the epithelial cells without being altered. Triglycerides, phospholipids, and cholesterol are then combined with protein inside the epithelial cells to form small particles called chylomicrons. of amino acids and
These tiny lipid and protein combinations are secreted into the central lacteals (lymphatic capillaries) of the intestinal villi . Absorbed lipids thus pass through the lymphatic system, eventually entering the venous blood by way of the thoracic duct . By contrast, amino acids and monosaccharides enter the hepatic portal vein.
http://humanphysiology2011.wikispaces.com/file/view/18.35.jpg/224359414/733x365/18.35.jpghttp://humanphysiology2011.wikispaces.com/file/view/18.35.jpg/224359414/733x365/18.35.jpg
Transport of Lipids in the Blood Once the chylomicrons are in the blood, their triglyceride content is removed by the enzyme lipoprotein lipase, which is attached to the endothelium of blood vessels. This enzyme hydrolyzes triglycerides and thus provides free fatty acids and glycerol for use by the cells. The remaining remnant particles, containing cholesterol, are taken up by the liver. This is a process of endocytosis that requires membrane receptors for the protein part (or apoprotein) of the remnant particle
Cholesterol and triglycerides produced by the liver are combined with other apoproteins and secreted into the blood as very-low-density lipoproteins (VLDLs), which deliver triglycerides to different organs. Once the triglycerides are removed, the VLDL particles are converted to low-density lipoproteins (LDLs), which transport cholesterol to various organs, including blood vessels. This can contribute to the development of atherosclerosis . Excess cholesterol is returned from these organs to the liver attached to high-density lipoproteins (HDLs). A high ratio of HDL-cholesterol to total cholesterol is believed to afford protection against atherosclerosis.
Absorption of Water and electrolytes By the time the ingesta enters the large intestine, approximately 80% of this fluid has been absorbed. Net movement of water across cell membranes always occurs by osmosis, and the fundamental concept needed to understand absorption in the small gut is that there is a tight coupling between water and solute absorption. Another way of saying this is that absorption of water is absolutely dependent on particularly sodium. absorption of solutes,
Vitamins As food is broken down by digestive juices, the intestines also absorb necessary vitamins for use in a variety of body functions, from fighting inflammation to repairing nerve damage. Water soluble vitamins such as B complex and C are only absorbed through the intestinal walls to the extent that the body has an immediate need for them; any excess is excreted in the urine, and new quantities of these vitamins must be consumed each day for optimal health. Fat soluble vitamins such as A, D, E and K are absorbed through the intestinal walls and stored in the liver and adipose tissue, or body fat, for use when needed.
Defecation After electrolytes and water have been absorbed, the waste material that is left passes to the rectum, leading to an increase in rectal pressure, relaxation of the internal anal sphincter, and the urge to defecate. If the urge to defecate is denied, feces are prevented from entering the anal canal by the external anal sphincter. In this case the feces remain in the rectum, and may even back up into the sigmoid colon. The defecation reflex normally occurs when the rectal pressure rises to a particular level that is determined, to a large degree, by habit. At this point, the external anal sphincter relaxes to admit feces into the anal canal. During the act of defecation, the longitudinal rectal muscles contract to increase rectal pressure, and the internal and external anal sphincter muscles relax.
Excretion is aided by contractions of abdominal and pelvic skeletal muscles, which pressure, The raised pressure helps to push the feces from the rectum, through the anal canal, and out of the anus raise the intra-abdominal