VA Healthcare Pilot Projects FY22-23
Six VA-funded pilot projects for FY22-23 focus on improving obstetrical quality of care, outpatient care utilization by Medicare-eligible veterans, fragmented care analysis, referral coordination, virtual care integration, and addressing disparities in access to care. Projects include assessing obstetrical care quality for veterans, studying the impact of the MISSION Act on Medicare-eligible veterans, and analyzing fragmented care networks utilized by veterans for high-cost services. These initiatives aim to enhance healthcare delivery for veterans and optimize care efficiency.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
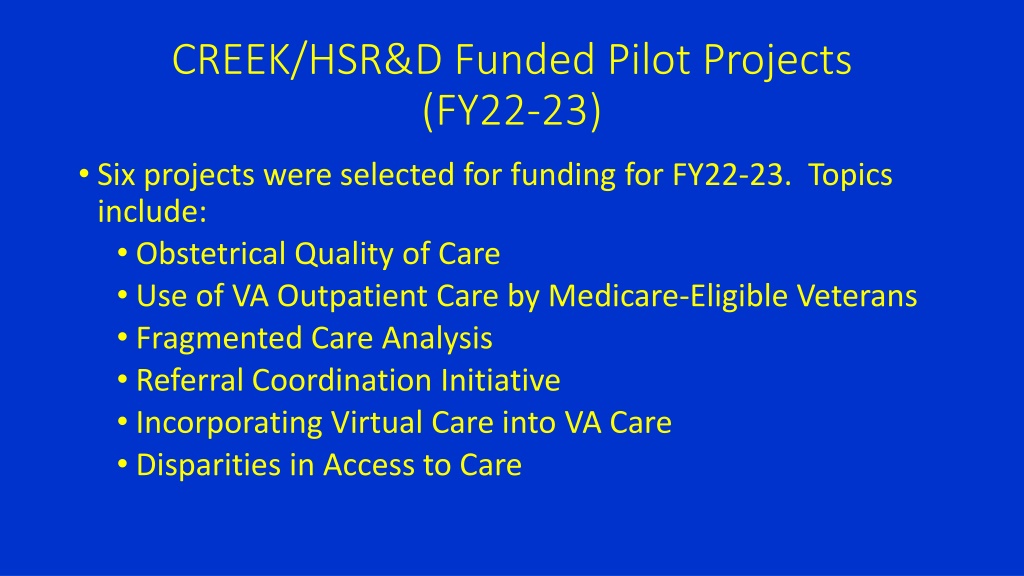
CREEK/HSR&D Funded Pilot Projects (FY22-23) Six projects were selected for funding for FY22-23. Topics include: Obstetrical Quality of Care Use of VA Outpatient Care by Medicare-Eligible Veterans Fragmented Care Analysis Referral Coordination Initiative Incorporating Virtual Care into VA Care Disparities in Access to Care
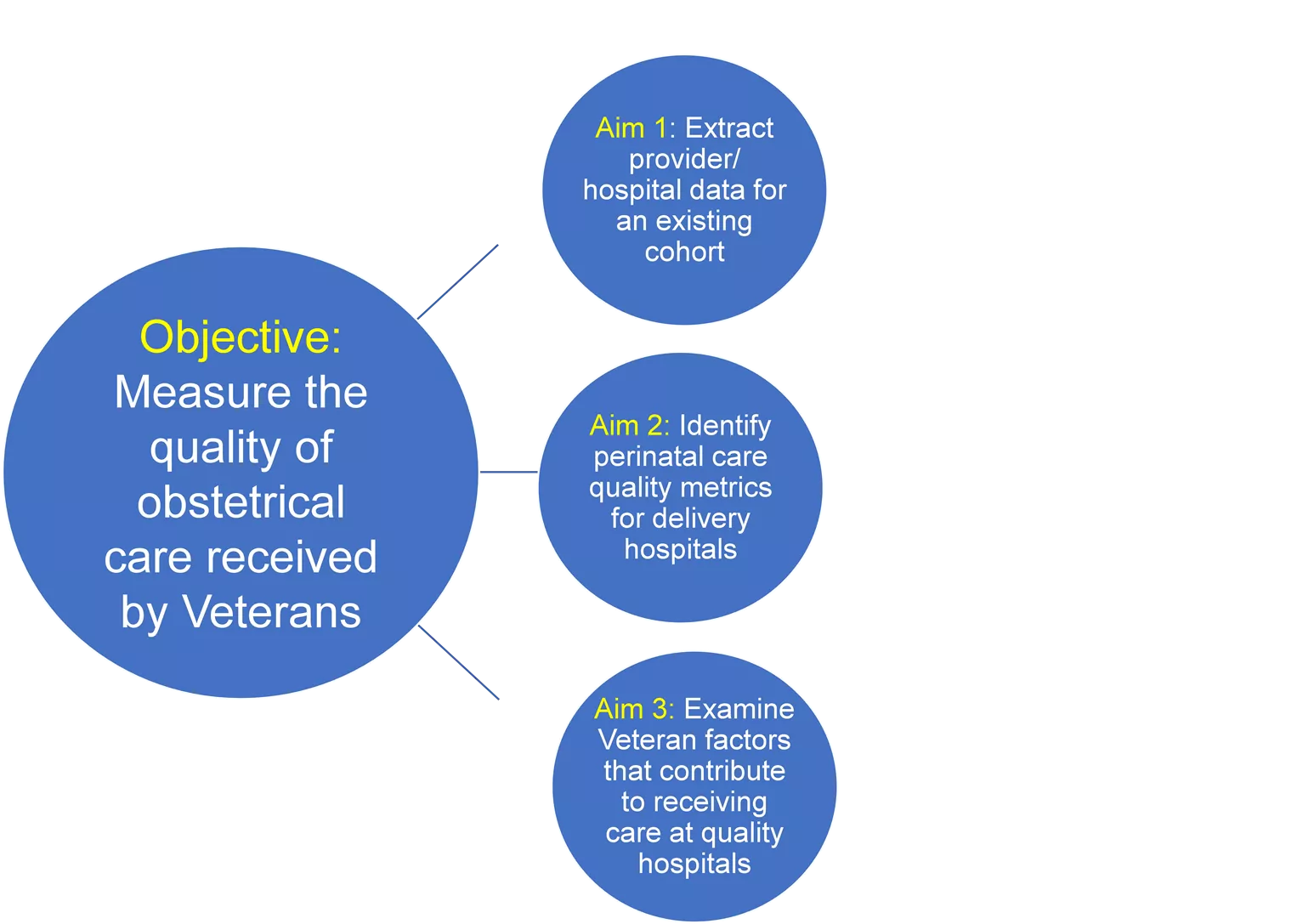
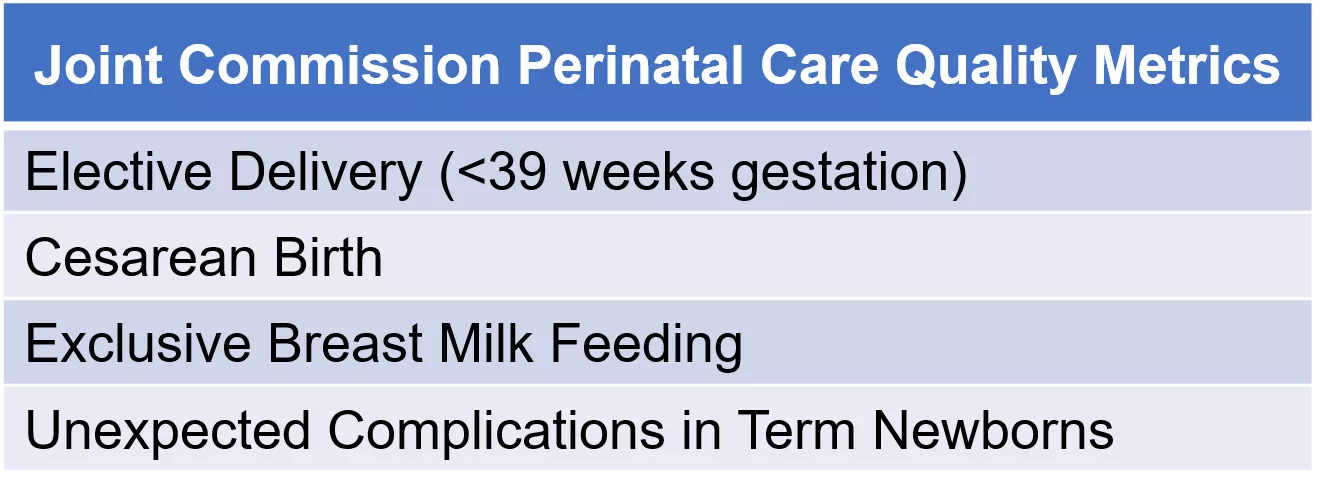
Assessing the Quality of Community Obstetrical Care for Veterans (Dr. Aimee Kroll-Desrosiers, VA Central Western MA) Aim 1: Extract provider/ hospital data for an existing cohort Joint Commission Perinatal Care Quality Metrics Elective Delivery (<39 weeks gestation) Cesarean Birth Exclusive Breast Milk Feeding Unexpected Complications in Term Newborns Objective: Measure the quality of obstetrical care received by Veterans Aim 2: Identify perinatal care quality metrics for delivery hospitals Research Questions: What proportion of Veterans delivered in a hospital with acceptable PC quality indicators? Aim 3: Examine Veteran factors that contribute to receiving care at quality hospitals Are Veteran characteristics associated with hospital PC quality measures?
Intended and Unintended Consequences of the MISSION Act for Medicare-Eligible Veterans VA Palo Alto project team: Rose, Vashi, Tran, Wagner Continuation of work examining how the MISSION Act is shaping VA Medicare has been the primary source of inpatient care for VA enrollees Show that VA enrollees shifted emergency care from Medicare -> VA Trying to examine this in outpatient services primary and specialty office visits, psychology, elective surgery, physical therapy/rehab, more Current status: a bit stuck with slow VA IRB, but pushing forward with the data we have Also continuing to engage with operations partners that are trying to slow down the growth in community care costs Goals: Work some results into HSR&D conference presentation + IIR submission
Fragmented Care Analysis GeoMapped Encounter Networks (FRAGMENT) (Dr. Zachary Hahn, VA Maine) Project Aims: Map the observed VA care network that Veterans use for high-cost services (Cardiology, Nephrology, Oncology, Sleep). Map the community care network that Veterans use for those same high-cost services. Develop and apply analytic tools to quantify the degree of VA care fragmentation. Analyze VA care network efficiency and develop strategies for care delivery optimization. Progress: IRB and local R&D approvals Generic implementation of analysis tools on synthetic data DART request for CDW data access in process
Incorporating Virtual Care into VA Care Options to Encourage Veterans to Remain in VA Care VA Teams: Garvin, Harvey (Boston), Zulman, Jacobs (Palo Alto), McInnes, Meterko (Bedford), Wray (San Francisco) Purpose: Evaluating Veteran attitudes and intentions toward (1) VA and Community Care for (2) multiple services and (3) modalities (in-person, video and phone telehealth) considering virtual care as periodic alternative to in-person Mixed methods study guided by Unified Theory of Acceptance and Use of Technology (UTAUT) National sample of 800 Veterans in the past year who had: VA in-person visit, VA Video Connect visit, and Community Care visit Mail push-to-web survey: Veterans attitudes and intent to use services: primary care, mental health, 9 specialties, rehab, CIH and ED/urgent care (14 service lines telehealth) Status: IRB approval expected Sept, Survey in Oct-Nov
Impact of the Referral Coordination Initiative on Veterans Decisions to Use Community Care Anna Zogas, PhD Anna Zogas, PhD anna.zogas@va.gov Amy Linsky, MD, MSc Problem: Kristin Mattocks, PhD, MPH Evaluating organizational approaches to creating a specialty care referral process that is patient-centered and best leverages VA and Community Care (CC) options Megan McCullough, PhD Varsha Vimalananda, MD, MPH Leslie Chatelain, MPH Ryann Engle, MPH Research objective: What influenced Veterans understanding and choice? 2. 1. Understand options? Value of referral coordination process? Factors in choosing VA or CC? System-, team-, individual-level factors in decision-making Refine with cognitive interviews with Veterans Develop Patient Survey Veteran Interviews Significance: Insight about referral coordination conversations and Veterans subsequent decisions about VA and CC Survey to be used in future studies to identify structures and processes that most influence the relative contribution of different factors in Veterans decisions
Examining the Impact of the MISSION Act on Disparities in Access to and Utilization of Primary Care (Dr. Deborah Gurewich, VA Boston) Study Aims Study Aims National- and facility-level; overall and by Race/Ethnicity & rurality Aim 1: Utilization Aim 2: Access (wait times and drive times) Aim 3: Quality of providers in CCN (available vs. used) Study Progress Study Progress Obtained VA data (FY20-FY22) and identified study sample Completed descriptive analysis of utilization trends of primary care in VA and CC overall and by sub-groups, and preparing multivariate analysis Acquired data for access analysis