Understanding Special Pathogens for Infection Prevention and Control
Pathogens such as Mycobacterium tuberculosis, Clostridium difficile, and antibiotic-resistant organisms like MRSA and VRE pose significant challenges to infection prevention programs. This content discusses the impact of these pathogens, transmission of tuberculosis, and clinical forms of TB. Antibiotic-resistant bacteria in healthcare settings and preventive measures are also highlighted.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Pathogens Important to Infection Prevention and Control
Learning objectives December 1, 2013 1. List special pathogens of interest to IP&C, and for each, describe the impact on the IP&C programme 2. Explain how antibiotic-resistant bacteria cause problems in healthcare 3. Outline preventive measures for a given special pathogen 2
Time involved December 1, 2013 90 minutes 3
Special pathogens December 1, 2013 Everyday problem microorganisms for infection prevention and control include: Mycobacterium tuberculosis Clostridium difficile Antibiotic resistant organisms MRSA, VRE Gram-negative multiply resistant organisms Enterobacteria (Escherichia coli, Klebsiella pneumoniae) Pseudomonas aeruginosa Acinetobacter baumanii 4
Mycobacterium tuberculosis December 1, 2013 Mycobacterium tuberculosis causes tuberculosis (TB) TB affects 1/3 of the world s population 9.4 million new cases in 2008 1.8 million deaths in 2008 Leading cause of death in people living with human immunodeficiency virus (HIV) 5
Transmissionand pathogenesis of TB - 1 December 1, 2013 Spread by the airborne route when someone with active disease and positive sputum smear coughs, talks, sneezes, or spits Bigger droplets spread up to 1 m, smaller spread by air Bacteria inhaled into lungs In lung tissue and lymph nodes the bacteria grow and reproduce Can travel to any location in the body 6
Transmission and pathogenesis of TB- 2 Latent TB bacteria contained in the body 10% of people with latent TB will develop active disease Most commonly affected organ - Lungs Untreated, a person with active disease can infect 10 to 15 people a year December 1, 2013 7
Clinical forms Pulmonary TB (active) Cough with thick cloudy, sometimes bloody sputum Tiredness Appetite loss/unexplained weight loss Night sweats Fever/chills Shortness of breath Extra pulmonary TB Signs and symptoms vary with site of infection Other common sites include central nervous system, bones, joints, and genitourinary system December 1, 2013 8
Risk Factors December 1, 2013 Weakened immune system Contact with someone with active TB Caring for active TB patients Living or working in crowded conditions with someone with active TB e.g., prisons, nursing homes, homeless shelters Poor access to healthcare Alcohol or drug abuse Travel to places where TB is endemic Being born in a country where TB is endemic Some medications for rheumatoid arthritis 9
Vaccination December 1, 2013 BCG strain of Mycobacterium bovis is used as a vaccine BCG is given to infants (best soon after birth) Vaccination against TB does not protect against infection but only against severe forms of disease Meningitis Disseminated TB (miliary) 10
Diagnosis & Management December 1, 2013 Chest x-ray Sputum smear for acid fast bacilli Tuberculin skin test (TST) Can take up to 3 months for those newly exposed to develop positive test May be falsely positive because of BCG vaccination Interferon gamma release assays (IGRA) in vaccinated persons Culture (can take up to six weeks) and sensitivity test 11
Management & Treatment December 1, 2013 Management of Exposure Confirmation of positive infection Medical evaluation to determine follow up Treatment of patients Treatment for latent or active TB should follow World Health Organization recommendations Incomplete treatment can cause resistance Adherence to therapy is critical 12
IP&C Measures December 1, 2013 Engineering controls Negative pressure rooms High efficiency particulate air (HEPA) filtration system Enhanced ventilation Ultraviolet irradiation (only in empty room) Sunlight exposure Open window (last resort if no other options) 13
Negative presssure room December 1, 2013 HEPA filter Air flow Patient with active TB isolated in negative pressure room 14
IP&C Measures - 1 December 1, 2013 Administrative Controls Identify patients with signs and symptoms of TB Additional precautions for patients suspected to have active TB Prompt treatment Vaccination of healthcare personnel Respiratory etiquette 15
IP&C Measures - 2 December 1, 2013 Personal Protective Equipment* N-95 fit tested masks for healthcare workers If not available, then surgical masks Surgical masks for patients leaving their rooms * Typically used for pulmonary TB if the patient is expectorating or has an open lesion 16
Conclusion December 1, 2013 Despite the high global impact of TB, it is treatable and preventable Occupation exposures remain a significant risk for healthcare workers IP&C measures are needed to decrease exposures to patients and healthcare workers 17
Clostridium difficile: Background December 1, 2013 There is a global increase in Clostridium difficile infections (CDI) and outbreaks over the past 10 years; however the illness is not a problem in all countries CDI primarily occurs in those patients exposed to antibiotics in healthcare facilities 18
Pathology - 1 December 1, 2013 A Gram-positive spore forming anaerobic bacillus Widely distributed in the environment In its vegetative state Produces toxins Can be killed by antibiotics Spore form Dormant No toxin production Resistant to antibiotics and disinfectants Can persist for months in the environment 19
Pathology - 2 December 1, 2013 Produces 2 toxins Toxin A and Toxin B Bind to intestinal epithelial cells causing inflammation and diarrhea Toxins are cytotoxic and enteropathic Alteration of the gut flora by antibiotics an important risk factor (decrease of normal gut flora) 20
Clinical Significance December 1, 2013 Mild disease Non-bloody diarrhoea, often mucoid and foul smelling, cramping, nausea, dehydration, low grade fever, leukocytosis Severe disease Colitis, watery diarrhoea, abdominal pain, fever, nausea, abdominal distension, pseudomembranes in the gut, toxic mega colon, death 21
New Strain December 1, 2013 Increased incidence of B1/NAP1/027 strain Causes severe disease More resistant to standard therapy More likely to relapse Associated with higher mortality 16x more toxin A; 23x more toxin B Related to excessive use of certain drugs/antibiotics 22
Colonisation December 1, 2013 Approximately 3-5% of healthy adults and 20 to 40% of hospitalised patients may be colonised Colonised patients generally are not symptomatic May be a potential reservoir for transmission Evidence suggest spores on the skin of asymptomatic patients can contaminate the hands of the healthcare worker No recommendations to treat carriers nor to perform admission screening 23
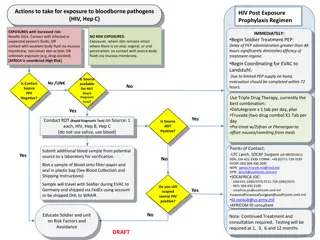
Transmission and Control Measures Patients at Risk Previous antibiotic use Severe underlying illness Prolonged hospital stay Advanced age Gastrointestinal surgery/manipulation History of irritable bowel disease Patients on proton pump inhibitors No Contact Yes Single room preferred Separate toileting facilities May be of benefit to implement a system to designate patients known to be colonised or infected for early notification on readmission Routine cleaning with attention to high touch surfaces and use of a sporicidal agent Consider double-cleaning for outbreak situations No diarrhoea for at least 48 hours December 1, 2013 Admission Screening Route of Transmission Isolation Precautions Accommodation Documentation (flagging of patients) Environmental Cleaning Discontinuation of Precautions Follow-up of Contacts Point Prevalence Additional Outbreak Measures No No Strict cleaning of multi-use equipment between patients Dedicated patient equipment to positive cases Education of staff, patients and visitors Auditing of outbreak unit/area including hand hygiene, isolation practices and environmental cleaning 24
Additional Control Measures December 1, 2013 Discontinuation of all antibiotics in a symptomatic patient (except for CDI) Facility-wide antibiotic control policies Early notification of patients with diarrhoea to the IC team Not recommended Routine identification of carriers Repeat testing post treatment for clearance 25
December 1, 2013 Antibiotic Resistant Microorganisms 26
December 1, 2013 Methicillin Resistant Staphylococcus aureus (MRSA) 27
Background Staphylococcus aureus is a Gram-positive bacteria 30% of people are permanently colonised Nose Pharynx Perineum Transient colonisation occurs, mainly on hands Colonisation although harmless, increases the risk of infection and transmission December 1, 2013 28
Clinical Significanceof MRSA December 1, 2013 First a problem in 1960s Globally has reached epidemic proportions Both community associated (CA) and healthcare associated (HA) strains of MRSA Rates vary by Country Region Individual healthcare facility 29
MRSA Transmission and Control Measures Previous antibiotic use Severe underlying illness Prolonged hospital stay Previous contact with medical facility Use of invasive procedures Close proximity to a patient colonised or infected with MRSA Yes, based on patient risk factors Nares, rectal, wounds, exit sites Patients at Risk December 1, 2013 Admission Screening Sites Contact (plus droplet for symptomatic patients with pneumonia) Route of Transmission Isolation Precautions Accommodation Documentation (flagging of patients) Yes Single room preferred May be of benefit to implement a system to designate patients known to be colonised or infected for early notification on readmission Routine cleaning with attention to high touch surfaces Environmental Cleaning Discontinuation of Precautions Unresolved issue: Some institutions use the following criteria: Negative results from all colonised/infected body sites- 3 consecutive cultures taken at least one week apart in the absence of antibiotic therapy Note: Re-colonisation is known to occur so on-going monitoring is recommended Consider maintaining isolation precautions in an outbreak setting Two sets of specimens taken on different days with one taken a minimum of 7 days after the last exposure, especially in an outbreak setting In an outbreak setting: Conduct serial (e.g., weekly) unit specific point prevalence cultures to determine if transmission has decreased or ceased Consider discharge and/transfer screening of patients until transmission has decreased or ceased Strict cleaning of multi-use equipment between patients Dedicated patient equipment to positive cases Education of staff, patients and visitors Auditing of outbreak unit/area including hand hygiene, isolation practices and environmental cleaning Follow-up of Contacts Point Prevalence 30 Additional Outbreak Measures
VISA and VRSA Vancomycin is drug of choice for treating MRSA infections Staphylococcus aureus with decreased (intermediate) susceptibility to vancomycin = VISA Staphylococcus aureus with resistance genes Van A or Van B = VRSA So far only few isolates in different parts of the world December 1, 2013 31
December 1, 2013 Vancomycin Resistant Enterococcus (VRE) 32
Background December 1, 2013 Enterococci are normal gut bacteria May also be present in the oropharynx, vagina, or on skin Causes serious bacterial infections Wound infections Urinary tract infections Endocarditis Sepsis Often resistant to ampicillin (the drug of choice); infections then treated with glycopeptides 33
VRE Epidemiology December 1, 2013 VRE is enterococcus that is resistant to the glycopeptide vancomycin First isolated in the 1980 s Spread globally causing asymptomatic colonization, infections, and outbreaks The prevalence of VRE varies worldwide 34
Clinical Significance December 1, 2013 Clinically relevant strains carry Van A or Van B resistance genes Limited antibiotics to treat VRE infections Transfer of resistance genes to other microorganisms such as MRSA is a great concern 35
VRE Transmission and Control Measures Previous antibiotic use Severe underlying illness Prolonged hospital stay Previous contact with medical facility Use of invasive procedures Close proximity to a patient colonised or infected with VRE Yes, based on patient risk factors. Rectum Contact Patients at Risk December 1, 2013 Admission Screening Sites Route of Transmission Isolation Precautions Accommodation Yes Single room preferred Separate toileting facilities May be of benefit to implement a system to designate patients known to be colonised or infected for early notification on readmission Routine cleaning with attention to high touch surfaces Consider double cleaning in outbreak situations Unresolved issue: Some institutions use the following criteria: Negative results from all colonised /infected body sites- 3 consecutive cultures taken at least one week apart in the absence of antibiotic therapy Note: Re-colonization is known to occur so on-going monitoring is recommended. Consider maintaining isolation precautions in an outbreak setting Two sets of specimens taken on different days with one taken a minimum of 7 days after the last exposure, especially in an outbreak setting In an outbreak setting: Conduct serial (e.g., weekly) unit specific point prevalence cultures to determine if transmission has decreased or ceased Consider discharge and/transfer screening of patients until transmission has decreased or ceased Strict cleaning of multi-use equipment between patients Dedicated patient equipment to positive cases Education of staff, patients and visitors Auditing of outbreak unit/area including hand hygiene, isolation practices and environmental cleaning Documentation (flagging of patients) Environmental Cleaning Discontinuation of Precautions Follow-up of Contacts Point Prevalence Additional Outbreak Measures 36
December 1, 2013 Multi-Drug Resistant Gram- Negative Microorganisms (MDRGN) 37
MDRGN- 1 December 1, 2013 The Enterobacteriaceae family of bacteria are a normal part of the gastrointestinal flora The most frequent isolates are: Escherichia coli Klebsiella pneumoniae Serratia marcescens Enterobacter species 38
Mechanisms of Resistance December 1, 2013 Escherichia coli and Klebsiella pneumoniae can have extended spectrum beta-lactamase (ESBL) enzymes that cause resistance to beta-lactam antibiotics including: Penicillins Cephalosporins Cephamycins Monobactams 39
Epidemiologyof ESBL strains December 1, 2013 There are various types of ESBLs including TEM SHV CTX-M ESBLs were first detected in Europe in 1980s Surveillance data from several surveillance systems indicate high rates of ESBLs in many parts of the world including USA, Canada, Europe, China, India and Latin America 40
Epidemiologyof CRE December 1, 2013 Carbapenem antibiotics are the treatment of choice for serious infections due to ESBL- producing bacteria Carbapenem Resistant Enterobacteriaceae (CRE) has also been reported Carbapenemases of importance include KPC, VIM, OXA and NDM-1 CREs have been reported in many areas of the world and have also been associated with outbreaks 41
MDRGN- 2 December 1, 2013 The following bacteria are present in aquatic environments Acinetobacter baumannii Pseudomonas aeruginosa Opportunistic pathogens in humans A major cause of healthcare-associated infections Septicemia Ventilator-associated pneumonia Urinary tract infections 42
MDR P. aeruginosa and MDR A. baumannii December 1, 2013 These microorganisms have intrinsically lower susceptibility to antibiotics Acquiring additional resistance genes (ESBL genes, other genes for resistance to beta lactam antibiotics, resistance genes for aminoglycosides and fluoroquinolones) very often means that they are susceptible only to carbapenems or colistin or resistant to all antibiotics (panresistant) 43
Clinical Significance December 1, 2013 MDRGN (including ESBLs, CREs, MDR PA and MDR AB) pose a significant treatment challenge including Increased length of stay Increased mortality Increased cost Contributes to the global crisis of antimicrobial resistance Control requires an aggressive world-wide strategy 44
MDRGN Transmission and Control Measures Previous antibiotic use Severe underlying illness Prolonged hospital stay Previous contact with medical facility Contact with a facility with known outbreaks with MDRGN organisms Yes, based on local epidemiology and patient risk factors. Rectum Patients at Risk December 1, 2013 Admission Screening Sites Contact (plus droplet for symptomatic patients with pneumonia) Yes Route of Transmission Isolation Precautions Single room preferred Accommodation May be of benefit to implement a system to designate patients known to be colonised or infected for early notification on readmission Routine cleaning with attention to high touch surfaces Documentation (flagging of patients) Environmental Cleaning Unresolved issue: Some institutions use the following criteria: Negative results from all colonised /infected body sites- 3 consecutive cultures taken at least one week apart in the absence of antibiotic therapy Note: Re-colonisation is known to occur so on-going monitoring is recommended Consider maintaining isolation precautions in an outbreak setting Based on local epidemiology and patient risk factors Discontinuation of Precautions Follow-up of Contacts In an outbreak setting: Conduct serial (e.g., weekly) unit specific point prevalence cultures to determine if transmission has decreased or ceased Consider discharge and/transfer screening of patients until transmission has decreased or ceased Strict cleaning of multi-use equipment between patients Dedicated patient equipment to positive cases Education of staff, patients and visitors Auditing of outbreak unit/area including hand hygiene, isolation practices and environmental cleaning Point Prevalence Additional Outbreak Measures 45
Management of Pathogens in Low Resource Countries December 1, 2013 IP&C measures vary based on institutional setting and available resources Hand hygiene should be a routine part of patient care in all settings Additional precautions may be considered depending on the pathogen, the institutional setting and outbreak circumstances 46
Conclusion December 1, 2013 Antimicrobial resistance is a world-wide public health problem Solutions require a multi-faceted approach Improving behaviours is essential Global awareness and surveillance is required Implementation of appropriate IP&C practices and antimicrobial stewardship processes may be beneficial 47
Key Points December 1, 2013 Tuberculosis and multi-drug resistant bacteria are important infection prevention and control issues Many have developed resistance to antimicrobials making them less effective Control measures vary by organism, setting and resources 48
Further reading December 1, 2013 Apisarnthanarak A, Fraser VJ. Feasibility and efficacy of infection control interventions to reduce the number of nosocomial infections and drug resistant microorganisms in developing countries: what else do we need? CID 2009;48:22-24 EARS-Net. http://www.ecdc.europa.eu/en/activities/surveillance/EARS -Net/Pages/index.aspx WHO 2010. Global tuberculosis control http://www.who.int/mediacentre/factsheets/fs104/en/inde x.html Special pathogens, in Damani N. Manual of infection prevention and control, 3rd ed. Oxford University Press, Oxford, 2012:183-249. 49
Quiz December 1, 2013 1. When a patient with active tuberculosis has to leave the isolation room for tests, s/he has to wear a N95 mask. T/F? Admission screening for MRSA encompasses the following specimens: a. Nares alone b. Nares, wounds, exit sites c. Nares, wounds d. Nares, exit sites ESBL genes are transmitted by plasmids and are restricted to Enterobacteriaceae. T/F? 2. 3. 50