Understanding the Genus Neisseria: Pathogens and Characteristics
The genus Neisseria comprises important pathogens such as Neisseria meningitidis and Neisseria gonorrhoeae, causing meningitis, gonorrhea, and other infections. This article explores their characteristics, differentiation from non-pathogenic species, properties like Gram-negative diplococci, and serogroups in meningococcus. Additionally, it highlights the role of fimbriae in adherence and intracellular presence in neutrophils. Images and descriptions supplement the detailed information provided.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Neisseria assist. Prof. Zainab Abdul jabar Aldhaher
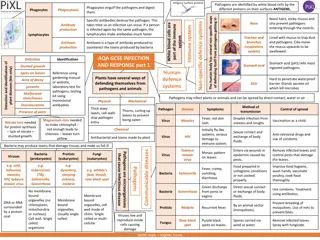
The genus Neisseria contains two important pathogens: 1. Neisseria meningitidis 2. Neisseria gonorrhoeae. N. meningitidis causes meningitis and meningococcemia. N. gonorrhoeae causes gonorrhea,neonatal conjunctivitis (ophthalmia neonatorum) and pelvic inflammatory disease.
There are a number of non- pathogenic species, such as N. mucosa and N. Lactamica which are members of the indigenous flora, including oral mucosa. Hence it is important to differentiate these from the pathogenic species from oral samples.
General characteristics Non motile, Gram- negative cocci ranging from 0.6 m to 1.0 m in diameter. On microscope the cocci are seen as pairs with concave adjacent flattened sides (bean-shaped).
Properties: Neisseriae are gram-negative diplococci ( Bean shaped). Oxidase-positive; i.e., they possess the enzyme cytochrome c and produce oxidase. They are cultured on "chocolate" agar N.meningitidis is maltose fermenter N. gonorrhoeae is maltose non fermenter N.meningititidis produces no beta lactamases. Some of N. gonorrhoeae produce beta lactamases.
Meningococcus has at least 13 serogroups on the basis of capsular polysaccharides. Important ones are A,B,C,Y and W-135. The endotoxin of N. meningitidis is a lipopolysaccharide (LPS) but the endotoxin of N. gonorrhoeae is a lipooligosaccharide (LOS). N.meningitidis is capsulated while N.gonorrhoea has no capsule
The organism is frequently found intracellulary in polymorphonuclear leukocytes (neutrophils) of the gonorrhea pustular exudates. Fimbriae which play a major role in adherence extend several micrometers from the cell surface.
Neisseria meningitidis: Pathogenesis: Humans are the only natural hosts.The organisms are transmitted by airborne droplets Colonize the nasopharynx and become transient flora of the upper respiratory tract. From the nasopharynx, the organism can enter the bloodstream and spread to meninges or cause meningococcemia.
N. meningitidis is the most common cause of meningitis in persons between the ages of 2 and 18 years. Outbreaks of meningitis are most common in winter and early spring, and favored by close contact between individuals. It has three important virulence factors: 1. Polysaccharride capsule. It is antiphagocytic in nature. 2. Endotoxin. It induces septic shock by causing release of cytokines. 3. IgA protease. It cleaves the IgA antibodies present in respiratory mucosa
Clinical Findings: 1. Meningitis 2. Meningococcemia 1.Meningitis. The symptoms are fever, headache, stiff neck, and an increased level of Neutrophils in spinal fluid. 2.Meningococcemia. It occurs due to multiplication of bacteria in the blood stream.
The severe form of it is life-threatening Waterhouse-Friderichsen syndrome. It is the septic shock induced by meningococcus. Also called Fulminant meningococcemia. Feature include high fever, shock, widespread purpura, disseminated intravascular coagulation, thrombocytopenia, and adrenal insufficiency due to bilateral adrenal hemorrhages.
Laboratory Diagnosis: A. Specimens include. 1. Blood for culture and smears 2. Spinal fluid for smear, culture, chemical analysis. B. Blood smears on gram staining show gram negative bean shaped diplococci. C. Culture. The organism grows best on chocolate agar incubated at 37 C in a 5% CO2 atmosphere. Colonies are transparent or opaque.
D. Oxidase test. Positive E. Manitol fermentation. The difference between N. meningitidis and N. gonorrhoeae is made on the basis of manitol fermentation. Meningococci ferment maltose, whereas gonococci do not. F. Latex agglutination test, which detects capsular polysaccharide in the spinal fluid.
Prevention: Chemoprophylaxis and immunization both used for prevention. Rifampin or ciprofloxacin used for prophylaxis in people who had close contact with the patient There are two forms of the meningococcal vaccine, each contains the capsular polysaccharide of groups A, C, Y, and W-135 as antigens (Tetravalent vaccine) 1. Unconjugated 2. Conjugated
Treatment Penicillin or cefotaxime (or equivalent cephalosporin)
Neisseria gonorrhoeae:(Goonococcus). Neisseria gonorrhoeae possesses a typical G- ve outer membrane composed of protein, phospholipid and lipopolysaccharide (LPS). however, Neisserial LPS is distinguished from enteric LPS by its highly branched basal oligosaccharide structure and the absence of repeating O- antigen subunits, for these reasons, neisserial LPS is reffered to as Lipooligosaccharide (LOS).
N. gonorrheoeae is a relatively fragile organism, susceptible to temperature changes, drying, UV- light and other environmental conditions. Strains of N. gonorrheoeae are variable in their cultural requirements so that media containing hemoglobin (heated blood), Yeast extract and other supplements are needed for isolation and growth of organism.
Cultures are grown at 35-39 C. although the non-pathogenic species can grow at temp. below 24C. Most strains are capnophilic (they require increased carbon dioxide for growth), haemolysed blood and solubilized starch enhance growth.
The surface components of gonococci that may play a role in virulence are: 1-major fimbrial protein (initial binding to epithelial cells) 2-outer membrane protein (contributes to invasion) 3- outer membrane porin (may prevent phagolysome formation in neutrophils and/or reduce oxidative burst).
4-outer membrane (LOS) (elicits inflammatory response, triggers release of TNF) 5-outer membrane receptors (iron acquisition for growth for transferrin) 6- outer membrane receptor (iron acquisition for growth lactoferrin)
Pathogenicity Gonococci possess a number of virulent attributes: 1- pili allow gonococci to adhere and colonize epithelial surfaces and thus cause infection. 2-IgA proteases produced by some gonococci break the heavy chain of immunoglobulin A (IgA ) thereby inactivating it (IgA is a major defence factor present on mucosal surfaces).
3-some isolate of N. gonorrhoeae produce -lactamase which is plasmid- mediated 4- Tracheal cytotoxin damages the ciliated cells of the fallopian tube, leading to scarring and sterility.
Clinical Findings: Transmitted sexually both in males and females. Cause pyogenic infections. Females are usually asymptomatic. N. gonorrhea causes following infections.
1. Genitourinary tract infections ( Gonorrhea) 2. Disseminated infection via spread through blood stream. 3. Rectal infections. 4. Pharyngitis 5. Ophthalmia neonatorum
Babies born to infected woman may suffer "ophthalmia neonatorum", in which the eyes are coated with gonococci as the baby passes down the birth canal. If untreated ophalmia leads rapidally to blindness. It may be prevented in areas of high prevalence by the instillation of 1% aqueous silver nitrate in the eyes of new born babies, alternatively topical erythromycin can be used. Occasionally, disseminated infections occur resulting in dermatitis-arthritis syndrome, endocarditis and meningitis.
Culture and identification Specimens are usually inoculated on to an enriched media (lysed blood or chocolate agar normally) and incubated under 5-10 CO2 (as the species is capnophilic). Small gray, oxidase positive colonies initially become large and opaque on prolonged incubation. Subsequent staining by fluorescent antibody techniques and production of acid from glucose but not from maltose or sucrose coniforms the identification. Gram stained smear usually reveal Gram negative, kidney shaped intracellular cocci in paires.
Treatment Penicillin is a drug of choice. If penicillin is contraindicated because of allergy or bacterial resistance there are many alternative: Fluoroquinolones, Tetracycline, ceftriaxone