Understanding Necrotizing Enterocolitis: Detection, Management, and Outcomes
Necrotizing enterocolitis (NEC) is a severe condition affecting premature and low birth weight infants, characterized by high mortality rates and long-term complications. The disease poses challenges in defining risk factors and treatment strategies, with considerable emphasis on prevention. Diagnosis involves a comprehensive work-up, including abdominal examination, laboratory tests, and imaging studies, with medical management focusing on gradual feeding advancement and antibiotic therapy. Post-NEC strictures may require investigations such as contrast enema and upper gastrointestinal studies. Surgical intervention is considered based on absolute and relative indications, emphasizing serial assessments for optimal decision-making.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
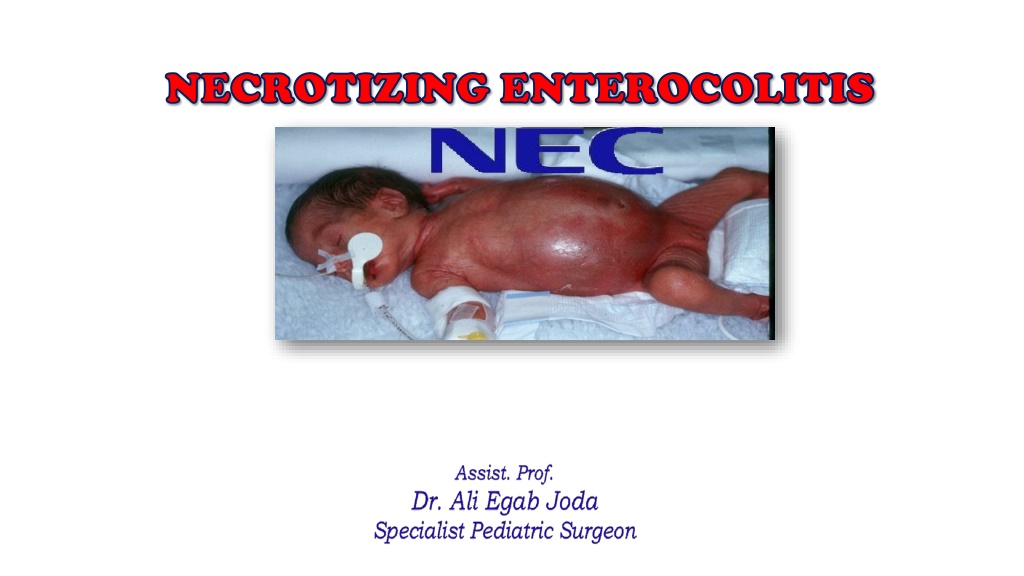
NECROTIZING ENTEROCOLITIS NECROTIZING ENTEROCOLITIS
NEC Disease of premature & low birth weight infant. Difficult to define. Unclear risk factors. What are the best treatment strategies ? What are the optimal prevention ? Considerable mortality & morbidity. Overlooked long term sequelae. Mortality of 15-30%. Mortality increased to 50% when surgery is necessary. Worse long-term outcomes. 90% of cases are preterm. Occasional cases in full-term. Term have the same clinical & patho. Findings but different initiating factors. considerable economic burden. 9- EGF (HB-EGF). 10- balance between constrictor ET-1 & dilator NO. 11- balance between commensal & pathologic Bactria. Epidemiology 2.3-11% of infant with less than 1500kg. Incidence & fatality inversely associated with B.W. BLACK race. Male infant. 2- intestinal digestion. 3- mucous coat. 4- tight junctions. 5- intestinal regeneration. 6- NO. 7- endotoxin (LPS). 8- PAF-AH. Pathophysiologic factors 1- intestinal motility. nNOS eNOS iNOS
Work-up for NEC Abdominal examination History Lab. Test Imaging Abd. Wall discoloration. Abd. distention. Pain, tenderness. Palpable mass. Scrotum. WBC. Platelet. Hb. ABG. Lactic acid. Erect abd film. Lat. decubitus film. Serial X-rays. Finding ? Ileus. Fixed loop. Pneumatosis. Portal V. gas. pneumoperit. Symptoms & signs. Exclude extra-abd. Problems Feeding regimen. Medications
Medical management for NEC Q/ For how long to continue on medical treatment ? 7 10 days. Stop all feeds. Insert NG Gastric decompression Q/ If patient shows clinical improvement ? Start slowly advancing feeds. Specific AB Anti-fungal ? Broad spectrum AB Q /If patient not tolerate feeds ? Repeat episode of NEC. Serial abd. exam, lab. Test & imaging Post-NEC stricture. Clinical deterioration Frequency of serial tests & imaging.
Post-NEC stricture Most commonly occur in : the left colon near splenic flexure. But may occur anywhere. What investigation you should consider ? Contrast enema & UGI study. Which is first to perform? & why ?
When to operate on NEC ? I- Absolute indications: Free air. II- Relative indications: best good fair 1- Portal venous gas. 2- positive paracentesis. 3- clinical deterioration. 1- fixed loop. 2- erythema. 3- palpable mass. Severe pneumatosis. Do not decide to operate after one assessment but after serial examinations.
Surgical management Surgical management Peritoneal drain Vs laparotomy ! Mortality ? Early results ? Delayed result ? Patients with peritoneal drain may have worse neurological outcomes 1-2 years after NEC recovery compared to laparotomy patients. Why ??? Neurological outcomes. Focal area of perforation.(drain , laparotomy). Discuss with family. How to decide between drain & laparotomy ? Currently unknown which is better. NEST (necrotizing enterocolitis surgery trial) RCT study. 300 patients. Follow up 18 -22 months after NEC recovery Results are expected in 2016.
Peritoneal drain Technique: Drain management: When to feed ? 3- transverse incision. 4- RIF. 5- penrose drain. 6- avoid too large incision. 7- enter abdominal cavity with hemostate. 8- place the drain carefully. 9- install normal saline to wash abd. Cavity. 9- secure the drain in place. 1- bed side. 2- L.A Irrigate the drain regularly to keep it patent. Start to remove it after 7-10 days. If continued leakage of stool ? If there is feeding intolerance, contrast study If patient doing well, start feeds. Hernia.
Operative management Pre-operative: 1- resuscitate the patient & correct any coagulopathy. 2- set up packed RBC, FFP, platelets for OR. Surgical technique: In the OR or bedside in NICU. Supra-umbilical transverse incision. Abd. Wall is very thin Assess the integrity of intestine, ischemia, necrosis, perforation. Segmental necrosis resection & primary anastomosis. proximal stoma & mucous fistula. stoma creation: Bring the stoma out through the same incision. Bring out the functional stoma & mucous fistula next to each other. Proper fixation of both ends to the fascia. Leave more length of the distal end. It is not necessary to mature the stoma. bowel, liver, spleen injury.
Management of diffuse NEC Usually see diffuse pneumatosis, unhealthy bowel but not necrotic. This is usually occur if you go to OR too early. Need to decide if there is something to resect. If you are unsure, it is better to leave intestine for second look. Consider leaving the abdomen open if there are dilated bowel. diverting stoma. Clipping & dropping: Usually for unstable patient with no time for multiple anastomosis. Only resect the necrotic bowel & return another day to complete the anastomosis when the patient is more stable. the operation & return another day. Continuing the operation will result in more serosal tears & bowel injuries & worse outcome to patient. If possible, identify the proximal bowel & create a diverting stoma. Management of skip lesions Consider resecting all lesions together with one anastomosis. If not, resect individual lesions, multiple anastomosis, proximal Currently no technique can manage such problem. Likelhood of survival through years of TPN to reach liver & intestine transplant is zero %. Just close the abdomen & pursue comfort care for the patient. Discuss with family & give them realistic explanations. The smartest decision a surgeon can make is know when to stop Decompress using angiocath as a temporizing maneuvuer as patient may not be stable enough to go to OR. Management of NEC totalis Management of extremely friable bowel Result from being forced to operate when the inflammatory process in the abdomen is at the peak. Abdominal compartement syndrome may occure from free air. Management of tension pneumoperitoneum
Post - operative management Reversing the stoma: Consider after the patient is stable & tolerating feeds. Wait until the patient is at least 2 kg. Consider re-feeding through mucous fistula if the patient has high output stoma. If there are signs of TPN- induced cholestasis or you cannot nourish the patient because of high output stoma, then consider closing the stoma sooner. Re-feeding through mucous fistula: Recent article shows a substantial decrease in TPN use. Be careful when creating the mucous fistula as they often retracted or get stenosis. Consider leaving a soft catheter in the fistula post- operatively to keep it open. Thank you