Understanding Menstruation and Ovulation Cycle in Women
Menstruation, the cyclic uterine bleeding, is a result of hormonal interplay. It signifies ovarian events controlled by the hypothalamic-pituitary axis. The menstrual cycle, spanning from one period to the next, involves the release of ova and hormones like estrogen and progesterone. Menstruation typically ceases around 45-50 years, lasting 4-5 days with a discharge comprising various components. The cycle is divided into ovarian and endometrial phases with distinct events like ovulation and formation of corpus luteum. The process involves follicle development, ovulation, and corpus luteum degeneration, occurring over a span of four weeks.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Menstruation & Ovulation Dr.Suresh Babu Chaduvula Professor Department of OBGYN College of Medicine
Menstruation Definition: The visible manifestation of cyclic physiologic uterine bleeding due to shedding of the endometrium. Due to invisible interplay of hormones through hypo-thalamo-pituitary-ovarian axis. For menstruation to occur axis should be active , endometrium should be receptive and outflow tract should be patent.
Menstrual Cycle The period extending from first day of period until the 1stday of next period. Normal length of a cycle is between 28-32 days. Mean 28 days. It occurs cyclically between 21-35 days. Menarche: First menstruation Age of onset 11-15 years &average is 13 years
Hypothalamus Menstruation is an external indicator of ovarian events controlled by the hypothalamic- pituitary axis GnRH (gonadotrophin releasing hormone) Pituitary LH FSH + ( gonadotrophins ) Feedback Ovaries Roles of the ovary 1. Gametes (ova) 2. Hormones Steroids (oestradiol, progesterone). Reproductive tract Other targets MENSTRUATION
Menstruation ceases between 45-50 years. Duration 4-5 days Amount 20-80 ml Menstrual discharge consists of blood, mucus, epithelial cells, fragments of endometrium, prostaglandins, enzymes and bacteria.
Menstrual cycle is divided into 1] Ovarian 2] Endometrial cycle
Timing events in the menstrual cycle. 2. LH surge LH Days before Days after Day 1 Day 1 Follicular phase Luteal phase 0 4 8 12 16 20 24 28 Menstruation OVULATION
Ovarian Cycle Development and maturation of a follicle, ovulation and formation of corpus luteum and its degeneration All these events occur in 4 weeks 1] Recruitment of group of follicles 2] Selection and maturation of dominant follicle 3] Ovulation 4] Corpus luteum formation and degeneration
Recruitment of Follicles Out of many primordial follicles only 20 antral follicles are developed in each cycle. All these follicles from 2-5 mm size are influenced by FSH. Those follicles not influenced by FSH will become atretic. Oocyte of each follicle grow out of proportion.Oocyte is surrounded by acellular glycoprotein from follicular cells called Zona pellucida
Flattened outer pregranulosa cells will become Granulosa cells. These cells contain FSH receptors.
Selection of a Dominant follicle and maturation Dominant follicle is called as Graafian Follicle out of 30-50 follicles from many primordial follicle. Starts from 5-7 days Follicle with high oestrogen and with maximum FSH receptors in granulosa cells will become a dominant one. Rest of follicles will become atretic by 8th day.
Animated ovarian events Key events in the ovarian cycle LH 1. Follicular growth Day 1 0 4 8 12 16 20 24 28 Menstruation Oestradiol OVULATION
Growth of follicles: Antral follicle Graafian follicle Primordial follicle Oocyte Ovulation Antrum (fluid filled space) Granulosa cells Thecal cells
Many! 30-50 Why is only 1 selected and becomes dominant ? How many follicles are growing at the start of the cycle? When do follicles start growing? Ovulation 2-3 months earlier! Menstruation
What controls follicular growth? OVULATORY FOLLICLE ?????? Gonadotrophin independent FSH + LH Ovulation Menstruation
OVULATORY FOLLICLE FSH + LH Ovulation OESTRADIOL As each follicle grows, it produces increasing amounts of oestradiol. Menstruation
Cumulus oophorus or Discus proligerous anchors the ovum to to the wall of follicle Corona radiata radially arranged cells around the ovum At this stage FSH induces LH receptors in granulosa cells of dominant follicle LH receptor induction is essential for mid cycle LH surge for ovulation and lutenisation of granulosa cells to form corpus luteum and secretion of progesterone
Graafian Follicle Graafian follicle measures 20 mm before ovulation It has following layers from outside inward 1] Theca externa 2] Theca interna 3] Membrana granulosa 4] granulosa cell layer 5] discus proligerous 6] corona radiata woth ovum inside And 7] antrum with fluid
The follicle is the fundamental element of the ovary: Blood vessels Granulosa cells Theca Antrum Cumulus cells Oocyte Zona pellucida (non-cellular glycoprotein coat)
Graafian Follicle and its Fluid Fluid contains: 1]Oestrogens 2] FSH 3] traces of androgens 4] Prolactin 5] OMI-oocyte maturation inhibitor 6] LI lutenisation inhibitor 7] Inhibin 8] Proteolytic enzymes 9] Plasmin
Time for development of a Follicle Total duration - 3 months Upto antral stage of 1mm 2months Upto 5 mm stage 2 weeks Upto 20 mm 2 weeks
Ovulation Causes: 1] LH surge secondary to sustained peak level of estrogens in the late follicular phase. This will cause completion of reduction division in the oocyte and lutenisation of granulosa cells, synthesise progesterone andprostaglandins. 2] FSH rise- leads to plasminogen and it helps in lysis of follicle.
3] Stretching factor Necrobiosis of wall due to passive stretching 4] Contraction of micromuscles in theca externa
Effects of Ovulation Following ovulation the follicle is changed to corpus luteum. Ovum will be picked up by fallopian tube and may fertilise or degenerate.
Corpus Luteum Life cycle is divided into 4 stages: 1] stage of proliferation 2] stage of vascularisation 3] stage of maturation and 4] stage of regression
Stage of Proliferation: Granulosa cells will become polyhedral and enlarged and with lipids looks greyish yellow called granulosa lutein cells Stage of vascularisation: small capillaries grow towards granulosa layer. Stage of maturation: After 1 week reaches 1-2cm and a carotene pigment will give a yellow color Stage of regression: on 22 -23 day regression starts.Lutein cells become atrophic and will become white called Corpus Albicans / if pregnancy occurs it will become Corpus luteum of pregnancy.
Hormones for formation and maintenance of corpus luteum 1] FSH induces LH receptors and LH surge causes lutenisation of granulosa cells and progesterone secretion.LH scretion should be continuous for function of corpus luteum 2]17 alfa OH progesterone and estradiol 3] Low level of prolactin Life span of Corpus luteum is 12-14 days.
Hormones from Corpus luteum 1] Progesterone 2] Oestrogen 3] Inhibin 4] Relaxin In absence of pregnancy levels of O+P+I decreases leading to rise in FSH and this in turn leads to recruitment of new follicles
Luteal- Placental Shift At 7- 10 weeks corpus luteum function will be taken up by Placenta
Endometrial or Uterine Cycle Endometrium contains surface epithelium, glands, stroma and blood vessels Endometrium has 2 zones: 1] Basal [ stratum basalis ] 2] Superficial functional zone
Uterine changes in the menstrual cycle. Endometrial depth More secretion from the glands hence the term secretory phase Oestradiol causes an increase in thickness (the proliferative phase ) 0 4 8 12 16 20 24 28 Menstruation OVULATION
Terminal differentiation of stromal cells decidualisation Characteristic spiral arteries 0 4 8 12 16 20 24 28 Optimal time for implantation Menstruation
Stratum Basalis:[ 1mm ] Ocupies 1/3 of endometrium basal arteries+ Not influenced by hormones Regeneration occurs from it. Functional zone: Responds to hormones like O+P In an ovulatory cycle four stages are seen.
Functional Zone stages 1] Stage of regeneration 2] Stage of Proliferation 3] Secretory phase 4] Menstrual phase
Stage of regeneration: Starts before menstruation and completes after 2-3 days after periods. Measures 2mm. Glands are lined by cubical cells Stage of Proliferation: Extends from 5-6th day to 14th day due to Estrogens.Glands are tubular and perpendicular to surface. Epithelium is columnar with nuclei at base, stromal cells are spindle shaped with spiral vessels upto epithelium. Subepithelial congestion +. Measures 3-4 mm.
Secretory Phase: Effects of O+P Oestrogen induces Progesterone receptors and progesterone is responsible for secretory phase. Starts at 15th day to 5-6 days prior to menstruation. Epithelium is more columnar and ciliated. Glands increase in size with taller epithelium with vacuoles formation- subnuclear vacuolation.
First and earliest effect of progesterone is appearence of subnucleolar vacuolation.It will persist upto 21 days. Saw toothed glandular epithelium, glands become corkscrew shaped with marked spiralling of vessels. Measures 6-8 mm. Regresssion of endometrium starts 24-48 hrs prior to periods. Marked spiralling of vessels and withdrawl of hormones causes tissue hypoxia and anoxia.
Menstrual phase Degeneration and casting off endometrium due to regression of corpus luteum with fall in level of O+P. Degeneration is due to stasis of blood and spasm of vessels leading to damage of vessels with escape of blood. Proteolytic enzymes from lysosomes causes local damage.[ Enzymatic autodigestion ]
What causes the onset of menstruation? Steroid levels fall This is followed by the onset of menstruation
How does menstruation stop? Prolonged vasoconstriction Myometrial contraction Local aggregation of platelets Endothelin and platelet activating factor are potent vasoconstrictors.
Regeneration of Endometrium Oestrogens Growth factors
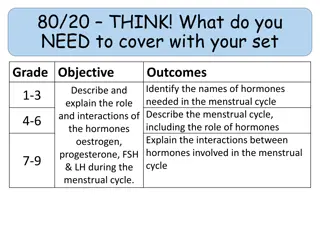
Hormones of ovarian and endometrial cycle At menstruation Oestrogen and inhibin are at low levels and high FSH. Oestrogen increases gradually and FSH decreases and remains static at day 5. O+ LH and androgen increases. Matuaration of follicle is combined effect of FSH and LH/ Peptides Inhibin, Activin and Follistatin Growth Facors IGF, EGF from theca cells modulate FSH,LH and peptide actions. IGF stimulates aromatase activity and progesterone synthesis. Progesterone will increase in secretory phase until 5 days before periods. LH will start declining
Hormones and Ovulation It occurs after 10-12 hrs following LH surge. It occurs after 24-36 hrs following Oestradiol peak of 200 pg/ml Progesterone peaks at 8th day after LH surge.
Datting of endometrium Examination of endometrium Luteal phase defect A discrepancy of more than 2 days in the postovulatory phase when endometrium is examined A woman can have periods without ovulation.
Cervical mucus Abundant mucus - like raw egg white Production of low viscosity mucus increases Cervical mucus Thick, rubbery, high viscosity - impenetrable to sperm. Variable number of dry days 0 4 8 12 16 20 24 28 Menstruation OVULATION
With increasing oestradiol: 1. The mucus becomes more abundant - up to 30x more and its water content increases. 2. Its pH becomes alkaline. 3. Increased elasticity ("spinnbarkeit test") 5. Ferning pattern caused by the interaction of high concentrations of salt and water with the glycoproteins in the mucus. Characteristic fernlike pattern as the mucus dries on a glass slide.
A small (0.5 oC) rise in BBT typically follows ovulation. 38 LH 37.8 37.6 37.4 37.2 37 36.8 36.6 Basal body temperature 36.4 36.2 36 0 4 8 12 16 20 24 28 Menstruation OVULATION
Basal body temperature Plasma oestradiol Plasma progesterone Volume of cervical mucus and sperm penetration Uterine endometrium
There are a number of potential ways of trying to identify the fertile period..: a) Calendar Method - which is essentially based on the previous menstrual history. b) Temperature method - using a midcycle rise in body temperature as a sign when ovulation has occurred. c) Cervical changes - which can be detected by feeling the cervix and cervical mucus. d) Hormonal methods - using over-the-counter "kits" to assess urinary hormone levels.